Immunologic Adverse Reactions of Β-Blockers and the Skin (Review)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Class Review Beta Adrenergic Blockers
Drug Class Review Beta Adrenergic Blockers Final Report Update 4 July 2009 Update 3: September 2007 Update 2: May 2005 Update 1: September 2004 Original Report: September 2003 The literature on this topic is scanned periodically. The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of, or recommendation for, any particular drug, use, or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Mark Helfand, MD, MPH Kim Peterson, MS Vivian Christensen, PhD Tracy Dana, MLS Sujata Thakurta, MPA:HA Drug Effectiveness Review Project Marian McDonagh, PharmD, Principal Investigator Oregon Evidence-based Practice Center Mark Helfand, MD, MPH, Director Oregon Health & Science University Copyright © 2009 by Oregon Health & Science University Portland, Oregon 97239. All rights reserved. Final Report Update 4 Drug Effectiveness Review Project TABLE OF CONTENTS INTRODUCTION .......................................................................................................................... 6 Purpose and Limitations of Evidence Reports........................................................................................ 8 Scope and Key Questions .................................................................................................................... 10 METHODS................................................................................................................................. -
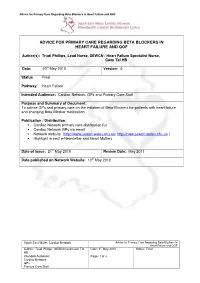
Advice for Primary Care Regarding Beta Blockers in Heart Failure and Qof
Advice for Primary Care Regarding Beta-Blockers in Heart Failure and QOF ADVICE FOR PRIMARY CARE REGARDING BETA BLOCKERS IN HEART FAILURE AND QOF Author(s): Trudi Phillips, Lead Nurse, SEWCN / Heart Failure Specialist Nurse, Cwm Taf HB Date: 20 th May 2010 Version: 4: Status Final Pathway: Heart Failure Intended Audience: Cardiac Network, GPs and Primary Care Staff Purpose and Summary of Document: To advise GPs and primary care on the initiation of Beta Blockers for patients with heart failure and changing Beta Blocker medication. Publication / Distribution: • Cardiac Network primary care distribution list • Cardiac Network GPs via email • Network website ( http://www.sewcn.wales.nhs.uk ; http://nww.sewcn.wales.nhs.uk ) • Highlight in next e-Newsletter and Heart Matters Date of Issue: 21 st May 2010 Review Date: May 2011 Date published on Network Website: 10 th May 2010 South East Wales Cardiac Network Advice for Primary Care Regarding Beta-Blockers in Heart Failure and QOF Author: Trudi Phillips. SEWCN and Cwm Taf Date: 7th May 2010 Status: Final HB Intended Audience: Page: 1 of 3 Cardiac Network GPs Primary Care Staff Advice for primary care regarding Beta-blockers in Heart Failure and QOF Carvedilol, Bisoprolol and Nebivolol (in the elderly) are the only three beta-blockers currently licensed for use in heart failure in the UK. Beta-blockade therapy for heart failure should be introduced in a ‘ start low, go slow ’ manner, with assessment of heart rate, blood pressure, and clinical status after each titration. Beta blocker Starting dose Maximum target dose Bisoprolol 1.25 mg od 10 mg od Carvedilol 3.125 mg bd 25mg bd Nebivolol (in the elderly) 1.25 mg od 10 mg od For patients with mild to moderate heart failure maximum dose of Carvedilol is 50 mg twice daily if weight more than 85 kg How to use: • Start with a low dose (see above). -

Research Article
z Available online at http://www.journalcra.com INTERNATIONAL JOURNAL OF CURRENT RESEARCH International Journal of Current Research Vol. 11, Issue, 12, pp.8946-8949, December, 2019 DOI: https://doi.org/10.24941/ijcr.37495.12.2019 ISSN: 0975-833X RESEARCH ARTICLE SKIN: A WINDOW FOR THYROID DISEASE 1Neethu Mary George, 2,*Amruthavalli Potlapati and 3Narendra Gangaiah 1 Resident, Department of Dermatology, Sri Siddhartha Medical College, Karnataka 2Assistant Professor, Department of Dermatology, Sri Siddhartha Medical College, Karnataka 3Professor and HOD, Department of Dermatology, Sri Siddhartha Medical College, Karnataka ARTICLE INFO ABSTRACT Article History: Introduction: Endocrine conditions form a major bulk of those visiting physicians and most of the Received 24th September, 2019 conditions warrant immediate and long term treatment which otherwise can indirectly affect all the Received in revised form organ systems and adversely affect the ‘health’ of a person. Thyroid diseases are one of the most 28th October, 2019 common endocrinological conditions with varying skin and appandageal manifestations. Skin is an Accepted 15th November, 2019 organ that is visible to naked eyes and can at times show certain manifestations which point to an Published online 31st December, 2019 underlying disease. Unless the clinician has high index of suspicion, such conditions can go undetected. Hence it becomes imperative for clinicians and Dermatologists to have an idea about the Key Words: cutaneous manifestations of endocrinological conditions and hence the study assess the skin Hyperthyroid, Hypothyroid, Cutaneous manifestations in recently detected hyper and hypothyroid patients. Objectives: To evaluate the cutaneous, hair and nail findings and associated conditions in acquired thyroid disorders. Manifestations, Pincer Nail. -

ORIGINAL ARTICLE a Clinical and Histopathological Study of Lichenoid Eruption of Skin in Two Tertiary Care Hospitals of Dhaka
ORIGINAL ARTICLE A Clinical and Histopathological study of Lichenoid Eruption of Skin in Two Tertiary Care Hospitals of Dhaka. Khaled A1, Banu SG 2, Kamal M 3, Manzoor J 4, Nasir TA 5 Introduction studies from other countries. Skin diseases manifested by lichenoid eruption, With this background, this present study was is common in our country. Patients usually undertaken to know the clinical and attend the skin disease clinic in advanced stage histopathological pattern of lichenoid eruption, of disease because of improper treatment due to age and sex distribution of the diseases and to difficulties in differentiation of myriads of well assess the clinical diagnostic accuracy by established diseases which present as lichenoid histopathology. eruption. When we call a clinical eruption lichenoid, we Materials and Method usually mean it resembles lichen planus1, the A total of 134 cases were included in this study prototype of this group of disease. The term and these cases were collected from lichenoid used clinically to describe a flat Bangabandhu Sheikh Mujib Medical University topped, shiny papular eruption resembling 2 (Jan 2003 to Feb 2005) and Apollo Hospitals lichen planus. Histopathologically these Dhaka (Oct 2006 to May 2008), both of these are diseases show lichenoid tissue reaction. The large tertiary care hospitals in Dhaka. Biopsy lichenoid tissue reaction is characterized by specimen from patients of all age group having epidermal basal cell damage that is intimately lichenoid eruption was included in this study. associated with massive infiltration of T cells in 3 Detailed clinical history including age, sex, upper dermis. distribution of lesions, presence of itching, The spectrum of clinical diseases related to exacerbating factors, drug history, family history lichenoid tissue reaction is wider and usually and any systemic manifestation were noted. -

C.O.E. Continuing Education Curriculum Coordinator
CONTINUING EDUCATION All Rights Reserved. Materials may not be copied, edited, reproduced, distributed, imitated in any way without written permission from C.O. E. Continuing Education. The course provided was prepared by C.O.E. Continuing Education Curriculum Coordinator. It is not meant to provide medical, legal or C.O.E. professional services advice. If necessary, it is recommended that you consult a medical, legal or professional services expert licensed in your state. Page 1 of 199 Click Here To Take Test Now (Complete the Reading Material first then click on the Take Test Now Button to start the test. Test is at the bottom of this page) 5 hr. Nail Structure and Growth & TCSG Health and Safety Outline Why Study Nail Structure and Growth? • The Natural Nail • Nail Anatomy • Nail Growth • Know Your Nails Objectives After completing this section, you should be able to: C.O.E.• Describe CONTINUING the structure and composition of nails. EDUCATION • Discuss how nails grow. • Identify diseases and disorders of the nail All Rights Reserved. Materials may not be copied, edited, reproduced, distributed, imitated in any way without written permission from C.O. E. Continuing Education. The course provided was prepared by C.O.E. Continuing Education Curriculum Coordinator. It is not meant to provide medical, legal or professional services advice. If necessary, it is recommended that you consult a medical, legal or professional services expert licensed in your state. 1 CONTINUING EDUCATION All Rights Reserved. Materials may not be copied, edited, reproduced, distributed, imitated in any way without written permission from C.O. -

General Dermatology an Atlas of Diagnosis and Management 2007
An Atlas of Diagnosis and Management GENERAL DERMATOLOGY John SC English, FRCP Department of Dermatology Queen's Medical Centre Nottingham University Hospitals NHS Trust Nottingham, UK CLINICAL PUBLISHING OXFORD Clinical Publishing An imprint of Atlas Medical Publishing Ltd Oxford Centre for Innovation Mill Street, Oxford OX2 0JX, UK tel: +44 1865 811116 fax: +44 1865 251550 email: [email protected] web: www.clinicalpublishing.co.uk Distributed in USA and Canada by: Clinical Publishing 30 Amberwood Parkway Ashland OH 44805 USA tel: 800-247-6553 (toll free within US and Canada) fax: 419-281-6883 email: [email protected] Distributed in UK and Rest of World by: Marston Book Services Ltd PO Box 269 Abingdon Oxon OX14 4YN UK tel: +44 1235 465500 fax: +44 1235 465555 email: [email protected] © Atlas Medical Publishing Ltd 2007 First published 2007 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, without the prior permission in writing of Clinical Publishing or Atlas Medical Publishing Ltd. Although every effort has been made to ensure that all owners of copyright material have been acknowledged in this publication, we would be glad to acknowledge in subsequent reprints or editions any omissions brought to our attention. A catalogue record of this book is available from the British Library ISBN-13 978 1 904392 76 7 Electronic ISBN 978 1 84692 568 9 The publisher makes no representation, express or implied, that the dosages in this book are correct. Readers must therefore always check the product information and clinical procedures with the most up-to-date published product information and data sheets provided by the manufacturers and the most recent codes of conduct and safety regulations. -

Different Beta-Blocking Effects of Carvedilol and Bisoprolol in Humans
Journal of Clinical and Basic Cardiology An Independent International Scientific Journal Journal of Clinical and Basic Cardiology 2001; 4 (1), 53-56 Different beta-blocking effects of carvedilol and bisoprolol in humans Koshucharova G, Klein W, Lercher P, Maier R, Stepan V Stoschitzky K, Zweiker R Homepage: www.kup.at/jcbc Online Data Base Search for Authors and Keywords Indexed in Chemical Abstracts EMBASE/Excerpta Medica Krause & Pachernegg GmbH · VERLAG für MEDIZIN und WIRTSCHAFT · A-3003 Gablitz/Austria ORIGINAL PAPERS, CLINICAL CARDIOLOGY Different Beta-Blocking Effects of Carvedilol and Bisoprolol J Clin Basic Cardiol 2001; 4: 53 Different Beta-Blocking Effects of Carvedilol and Bisoprolol in Humans G. Koshucharova, R. Zweiker, R. Maier, P. Lercher, V. Stepan, W. Klein, K. Stoschitzky Bisoprolol is a beta1-selective beta-adrenergic antagonist while carvedilol is a non-selective beta-blocker with additional blockade of alpha1-adrenoceptors. Administration of bisoprolol has been shown to cause up-regulation of β-adrenoceptor density and to decrease nocturnal melatonin release, whereas carvedilol lacks these typical effects of beta-blocking drugs. The objective of the present study was to investigate beta-blocking effects of bisoprolol and carvedilol in healthy subjects. We compared the effects of single oral doses of clinically recommended amounts of bisoprolol (2.5, 5 and 10 mg) and carvedilol (25, 50 and 100 mg) to those of placebo in a randomised, double-blind, cross-over study in 12 healthy male volun- teers. Three hours after oral administration of the drugs heart rate and blood pressure were measured at rest, after 10 min. of exercise, and after 15 min. -

Supporting Information a Analysed Substances
Electronic Supplementary Material (ESI) for Analyst. This journal is © The Royal Society of Chemistry 2020 List of contents: Tab. A1 Detailed list and classification of analysed substances. Tab. A2 List of selected MS/MS parameters for the analytes. Tab. A1 Detailed list and classification of analysed substances. drug of therapeutic doping agent analytical standard substance abuse drug (WADA class)* supplier (+\-)-amphetamine ✓ ✓ S6 stimulants LGC (+\-)-methamphetamine ✓ S6 stimulants LGC (+\-)-3,4-methylenedioxymethamphetamine (MDMA) ✓ S6 stimulants LGC methylhexanamine (4-methylhexan-2-amine, DMAA) S6 stimulants Sigma cocaine ✓ ✓ S6 stimulants LGC methylphenidate ✓ ✓ S6 stimulants LGC nikethamide (N,N-diethylnicotinamide) ✓ S6 stimulants Aldrich strychnine S6 stimulants Sigma (-)-Δ9-tetrahydrocannabinol (THC) ✓ ✓ S8 cannabinoids LGC (-)-11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THC-COOH) S8 cannabinoids LGC morphine ✓ ✓ S7 narcotics LGC heroin (diacetylmorphine) ✓ ✓ S7 narcotics LGC hydrocodone ✓ ✓ Cerillant® oxycodone ✓ ✓ S7 narcotics LGC (+\-)-methadone ✓ ✓ S7 narcotics Cerillant® buprenorphine ✓ ✓ S7 narcotics Cerillant® fentanyl ✓ ✓ S7 narcotics LGC ketamine ✓ ✓ LGC phencyclidine (PCP) ✓ S0 non-approved substances LGC lysergic acid diethylamide (LSD) ✓ S0 non-approved substances LGC psilocybin ✓ S0 non-approved substances Cerillant® alprazolam ✓ ✓ LGC clonazepam ✓ ✓ Cerillant® flunitrazepam ✓ ✓ LGC zolpidem ✓ ✓ LGC VETRANAL™ boldenone (Δ1-testosterone / 1-dehydrotestosterone) ✓ S1 anabolic agents (Sigma-Aldrich) -

Copyrighted Material
Part 1 General Dermatology GENERAL DERMATOLOGY COPYRIGHTED MATERIAL Handbook of Dermatology: A Practical Manual, Second Edition. Margaret W. Mann and Daniel L. Popkin. © 2020 John Wiley & Sons Ltd. Published 2020 by John Wiley & Sons Ltd. 0004285348.INDD 1 7/31/2019 6:12:02 PM 0004285348.INDD 2 7/31/2019 6:12:02 PM COMMON WORK-UPS, SIGNS, AND MANAGEMENT Dermatologic Differential Algorithm Courtesy of Dr. Neel Patel 1. Is it a rash or growth? AND MANAGEMENT 2. If it is a rash, is it mainly epidermal, dermal, subcutaneous, or a combination? 3. If the rash is epidermal or a combination, try to define the SIGNS, COMMON WORK-UPS, characteristics of the rash. Is it mainly papulosquamous? Papulopustular? Blistering? After defining the characteristics, then think about causes of that type of rash: CITES MVA PITA: Congenital, Infections, Tumor, Endocrinologic, Solar related, Metabolic, Vascular, Allergic, Psychiatric, Latrogenic, Trauma, Autoimmune. When generating the differential, take the history and location of the rash into account. 4. If the rash is dermal or subcutaneous, then think of cells and substances that infiltrate and associated diseases (histiocytes, lymphocytes, mast cells, neutrophils, metastatic tumors, mucin, amyloid, immunoglobulin, etc.). 5. If the lesion is a growth, is it benign or malignant in appearance? Think of cells in the skin and their associated diseases (keratinocytes, fibroblasts, neurons, adipocytes, melanocytes, histiocytes, pericytes, endothelial cells, smooth muscle cells, follicular cells, sebocytes, eccrine -

Different Effects of Propranolol, Bisoprolol, Carvedilol and Doxazosin on Heart Rate, Blood Pressure, and Plasma Concentrations of Epinephrine and Norepinephrine K
Journal of Clinical and Basic Cardiology An Independent International Scientific Journal Journal of Clinical and Basic Cardiology 2003; 6 (1-4), 69-72 Different Effects of Propranolol Bisoprolol, Carvedilol and Doxazosin on Heart Rate, Blood Pressure, and Plasma Concentrations of Epinephrine and Norepinephrine Stoschitzky K, Donnerer J, Klein W, Koshucharova G Kraxner W, Lercher P, Maier R, Watzinger N, Zweiker R Homepage: www.kup.at/jcbc Online Data Base Search for Authors and Keywords Indexed in Chemical Abstracts EMBASE/Excerpta Medica Krause & Pachernegg GmbH · VERLAG für MEDIZIN und WIRTSCHAFT · A-3003 Gablitz/Austria ORIGINAL PAPERS, CLINICAL CARDIOLOGY Alpha- Versus Beta-Blockers J Clin Basic Cardiol 2003; 6: 69 Different Effects of Propranolol, Bisoprolol, Carvedilol and Doxazosin on Heart Rate, Blood Pressure, and Plasma Concentrations of Epinephrine and Norepinephrine K. Stoschitzky1, G. Koshucharova1, R. Zweiker1, P. Lercher1, R. Maier1, N. Watzinger1, W. Kraxner1, W. Klein1, J. Donnerer2 Background: Despite of its beta-blocking effects, carvedilol has been shown not to decrease resting heart rate in healthy subjects. Therefore, we compared haemodynamic effects of carvedilol (an alpha- and beta-blocker), propranolol (a non-selec- tive beta-blocker), bisoprolol (a beta1-selective beta-blocker), doxazosin (an alpha-blocker) and placebo, at rest and during exercise. In addition, we measured plasma levels of epinephrine and norepinephrine. Methods: Twelve healthy males received single oral doses of 80 mg propranolol, 5 mg bisoprolol, 50 mg carvedilol, 4 mg doxazosin and placebo according to a randomized, double-blind, crossover protocol. Three hours after drug intake, heart rate and blood pressure were measured at rest, after 10 min of exercise, and after 15 min of recovery. -
Copyrighted Material
1 Index Note: Page numbers in italics refer to figures, those in bold refer to tables and boxes. References are to pages within chapters, thus 58.10 is page 10 of Chapter 58. A definition 87.2 congenital ichthyoses 65.38–9 differential diagnosis 90.62 A fibres 85.1, 85.2 dermatomyositis association 88.21 discoid lupus erythematosus occupational 90.56–9 α-adrenoceptor agonists 106.8 differential diagnosis 87.5 treatment 89.41 chemical origin 130.10–12 abacavir disease course 87.5 hand eczema treatment 39.18 clinical features 90.58 drug eruptions 31.18 drug-induced 87.4 hidradenitis suppurativa management definition 90.56 HLA allele association 12.5 endocrine disorder skin signs 149.10, 92.10 differential diagnosis 90.57 hypersensitivity 119.6 149.11 keratitis–ichthyosis–deafness syndrome epidemiology 90.58 pharmacological hypersensitivity 31.10– epidemiology 87.3 treatment 65.32 investigations 90.58–9 11 familial 87.4 keratoacanthoma treatment 142.36 management 90.59 ABCA12 gene mutations 65.7 familial partial lipodystrophy neutral lipid storage disease with papular elastorrhexis differential ABCC6 gene mutations 72.27, 72.30 association 74.2 ichthyosis treatment 65.33 diagnosis 96.30 ABCC11 gene mutations 94.16 generalized 87.4 pityriasis rubra pilaris treatment 36.5, penile 111.19 abdominal wall, lymphoedema 105.20–1 genital 111.27 36.6 photodynamic therapy 22.7 ABHD5 gene mutations 65.32 HIV infection 31.12 psoriasis pomade 90.17 abrasions, sports injuries 123.16 investigations 87.5 generalized pustular 35.37 prepubertal 90.59–64 Abrikossoff -

Wednesday, June 12, 2019 4:00Pm
Wednesday, June 12, 2019 4:00pm Oklahoma Health Care Authority 4345 N. Lincoln Blvd. Oklahoma City, OK 73105 The University of Oklahoma Health Sciences Center COLLEGE OF PHARMACY PHARMACY MANAGEMENT CONSULTANTS MEMORANDUM TO: Drug Utilization Review (DUR) Board Members FROM: Melissa Abbott, Pharm.D. SUBJECT: Packet Contents for DUR Board Meeting – June 12, 2019 DATE: June 5, 2019 Note: The DUR Board will meet at 4:00pm. The meeting will be held at 4345 N. Lincoln Blvd. Enclosed are the following items related to the June meeting. Material is arranged in order of the agenda. Call to Order Public Comment Forum Action Item – Approval of DUR Board Meeting Minutes – Appendix A Update on Medication Coverage Authorization Unit/Use of Angiotensin Converting Enzyme Inhibitor (ACEI)/ Angiotensin Receptor Blocker (ARB) Therapy in Patients with Diabetes and Hypertension (HTN) Mailing Update – Appendix B Action Item – Vote to Prior Authorize Aldurazyme® (Laronidase) and Naglazyme® (Galsulfase) – Appendix C Action Item – Vote to Prior Authorize Plenvu® [Polyethylene Glycol (PEG)-3350/Sodium Ascorbate/Sodium Sulfate/Ascorbic Acid/Sodium Chloride/Potassium Chloride] – Appendix D Action Item – Vote to Prior Authorize Consensi® (Amlodipine/Celecoxib) and Kapspargo™ Sprinkle [Metoprolol Succinate Extended-Release (ER)] – Appendix E Action Item – Vote to Update the Prior Authorization Criteria For H.P. Acthar® Gel (Repository Corticotropin Injection) – Appendix F Action Item – Vote to Prior Authorize Fulphila® (Pegfilgrastim-jmdb), Nivestym™ (Filgrastim-aafi),