Dr. Robert Mcdougall and the Saskatchewan Roughriders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Matter of Inches My Last Fight
INDEPENDENT PUBLISHERS GROUP A Matter of Inches How I Survived in the Crease and Beyond Clint Malarchuk, Dan Robson Summary No job in the world of sports is as intimidating, exhilarating, and stressridden as that of a hockey goaltender. Clint Malarchuk did that job while suffering high anxiety, depression, and obsessive compulsive disorder and had his career nearly literally cut short by a skate across his neck, to date the most gruesome injury hockey has ever seen. This autobiography takes readers deep into the troubled mind of Clint Malarchuk, the former NHL goaltender for the Quebec Nordiques, the Washington Capitals, and the Buffalo Sabres. When his carotid artery was slashed during a collision in the crease, Malarchuk nearly died on the ice. Forever changed, he struggled deeply with depression and a dependence on alcohol, which nearly cost him his life and left a bullet in his head. Now working as the goaltender coach for the Calgary Flames, Malarchuk reflects on his past as he looks forward to the future, every day grateful to have cheated deathtwice. 9781629370491 Pub Date: 11/1/14 Author Bio Ship Date: 11/1/14 Clint Malarchuk was a goaltender with the Quebec Nordiques, the Washington Capitals, and the Buffalo Sabres. $25.95 Hardcover Originally from Grande Prairie, Alberta, he now divides his time between Calgary, where he is the goaltender coach for the Calgary Flames, and his ranch in Nevada. Dan Robson is a senior writer at Sportsnet Magazine. He 272 pages lives in Toronto. Carton Qty: 20 Sports & Recreation / Hockey SPO020000 6.000 in W | 9.000 in H 152mm W | 229mm H My Last Fight The True Story of a Hockey Rock Star Darren McCarty, Kevin Allen Summary Looking back on a memorable career, Darren McCarty recounts his time as one of the most visible and beloved members of the Detroit Red Wings as well as his personal struggles with addiction, finances, and women and his daily battles to overcome them. -

Hockey in Wartime Canada, 1939-1945
FOR CLUB OR COUNTRY? HOCKEY IN WARTIME CANADA, 1939-1945 BY Gabriel Stephen Panunto, B.A. A thesis submitted to the Faculty of Graduate Studies and Research in partial fulfillment of the requirements for the degree of Master of Arts Department of History Carleton University Ottawa Ontario July 19, 2000 Q copyright 2000 Gabriel Stephen Panunto National Library Bibliothèque nationale I*I of Canada du Canada Acquisitions and Acquisitions et Bibliographie Services services bibliographiques 395 Wellington Street 395, rue Wellington Ottawa ON KtA ON4 OnawaON KlAON4 Canada Canada The author has granted a non- L'auteur a accordé une licence non exclusive licence allowing the exclusive permettant à la National Library of Canada to Bibliothèque nationale du Canada de reproduce, loan, distribute or sel1 reproduire, prêter, distribuer ou copies of this thesis in microform, vendre des copies de cette thèse sous paper or electronic formats. la forme de microfiche/film, de reproduction sur papier ou sur format électronique. The author retains ownership of the L'auteur conserve la propriété du copyright in this thesis. Neither the droit d'auteur qui protège cette thèse. thesis nor substantial extracts fiom it Ni la thèse ni des extraits substantiels may be printed or otherwise de celle-ci ne doivent être imprimés reproduced without the author's ou autrement reproduits sans son permission. autorisation. ABSTRACT Sports reflect the societies that support them, and hockey in Canada during World War Two is no exception. Popular hockey history has defined the era as one of great sacrifices by the National Hockey League. largely because academic research is non- existent. -

Pickers World SELLER MANAGED Business Online Auction - Princess Street
09/28/21 12:47:52 Kingston (Ontario, Canada) Pickers World SELLER MANAGED Business Online Auction - Princess Street Auction Opens: Tue, Mar 29 5:45pm ET Auction Closes: Tue, Apr 5 8:30pm ET Lot Title Lot Title 0001 Sidney Crosby Hockey Card Collection Of 10 0032 Gilbert Perreault Signed Hockey Card 0002 Wayne Gretzky Hockey Card Lot Of 15 0033 Patrick Marleau & Dany Heatly Autographed 0004 Corey Perry Upper Deck Autographed Card Card 0005 Clyde Gates Game Worn Jersey Card NFL 0034 Brad Richards Signed Rookie Card Dolphins. 0035 Pavel Bure Hand Signed Hockey Card 0006 1986 Mario Lemieux Hockey Card 0036 Mike Modano Hand Signed Hockey Card 0007 1960-1961 Parkhurst Johnny Bower Card 0037 Teemu Selanne Hand Signed Hockey Card 0008 1960-1961 Parkhurst Bobby Baun Card 0038 1950's Bee Hive Johnny Bower Photo 0009 1962-1963 Frank Mahovlich Parkhurst Card 0039 1950's Bee Hive Tim Horton Photo 0010 1962-1963 Dave Keon Parkhurst Card 0040 1950's Bee Hive Bob Pulford Photo 0011 1961-1962 Dick Duff Parkhurst Card 0041 1977 Blue Jays Vs Red Sox Ticket 0012 1961-1962 Carl Brewer Parkhurst Card 0042 1977 Blue Jays Vs Rangers Ticket 0013 1961-1962 George Armstrong Parkhurst Card 0043 1970's Baseball Round Cards Lot Of 4 0014 1959-1960 Tim Horton Parkhurst Hockey Card 0044 1962 Sherriff Salada Hockey Coin Lot Of 8 0015 1974-1975 OPC Dennis Potvin Rookie Card 0045 1963 Shirriff Dave Keon Hockey Metal Coin 0016 1970-1971 Bobby Hull OPC All Star Hockey 0046 1963 Shirriff Frank Mahovlich Hockey Metal Card Coin 0018 1959-1960 Parkhurst Doug Harvey Hockey Card -

Franchise Record Book
FRANCHISE RECORD BOOK All-Time WHL Franchise Record: (1961-1967) 424 games - 200 wins - 202 losses - 22 ties - 422 points - .498 winning percentage Home record: 212 games – 131 wins – 74 losses – 7 ties – .634 winning percentage Away record: 212 games – 69 wins – 128 losses – 15 ties – .361 winning percentage All-Time NHL Franchise Record: (1967-1978) 858 games - 229 wins - 488 losses - 141 ties - 599 points - .349 winning percentage Home record: 429 games - 156 wins - 180 losses - 93 ties - 405 points - .472 winning percentage Away record: 429 games - 73 wins - 308 losses - 48 ties - 194 points - .226 winning percentage All-Time NHL Franchise Record as: California Seals (1967): 25 games - 6 wins - 14 losses - 5 ties - 17 points - .340 winning percentage Home record: 12 games - 5 wins - 3 losses - 4 ties - 14 points - .583 winning percentage Away record: 13 games - 1 win - 11 losses - 1 tie - 3 points - .115 winning percentage Oakland Seals (1967-1970): 203 games - 60 wins - 106 losses - 37 ties - 157 points - .387 winning percentage Home record: 101 games - 39 wins - 43 losses - 19 ties - 97 points - .480 winning percentage Away record: 102 games - 21 wins - 63 losses - 18 ties - 60 points - .294 winning percentage California Golden Seals (1970-1976): 470 games - 116 wins - 281 losses - 73 ties - 305 points - .324 winning percentage Home record: 236 games - 84 wins - 100 losses - 52 ties - 220 points - .466 winning percentage Away record: 234 games - 32 wins - 181 losses - 21 ties - 85 points - .182 winning percentage Cleveland Barons -

Hockey Hall of Fame Is the Perfect Place for Such a Deal
Dec. 21, 2008----- TORONTO, Ont.----A young friend just married a huge sports fan. He's the kind of guy who likes to drive around North America taking in essential sites like minor league baseball stadiums in Toledo, Ohio. She, not so much. But the promise of travel over the next 50 years gives her a chance to shop, sightsee and check out regional cuisine. This prevents any marriage from becoming cold steel on ice. The Hockey Hall of Fame is the perfect place for such a deal. The hall of fame opened in 1993 at Brookfield Place in downtown Toronto. The soul of the hall is where the Stanley Cup resides -- under a stained glass skylight inside a Bank of Montreal building. Constructed in 1885, this part of the hall had been the oldest bank building in North America. The rest of the museum is adjacent to an office and retail complex and expansive food court. Brookfield Place also is linked to the Allen Lambert Galleria, a dazzling six-story light and glass building designed by Spanish architect Santiago Calatrava, on board for the Chicago Spire. The downtown hockey hall has become one of Toronto's top tourist attractions. My summer visit is on my mind because it is cold in Chicago. And the Blackhawks host the outdoor Winter Classic on New Year's Day before 41,000 fans at a sold-out Wrigley Field. A Chicago angle is apparent the minute you enter the Hockey Hall of Fame. One of the first things I saw was smiling Blackhawk Bill Mosienko, the pucks and stick from his fastest hat trick -- three goals in one game -- in National Hockey League (NHL) history. -

Ken Dryden. the Game.Pdf
O-Pee-Chee/Hockey Hall of Fame Frank Prazak/Hockey Hall of Fame PRAISE FOR THE GAME “A first-rate discussion of hockey by one of hockey’s first-rate players and first-rate minds …. Essential reading for anyone serious about hockey as an important part of Canadian life.” —Hamilton Spectator “The Game is a beautifully written, insightful, perceptive, revealing look at hockey.” —Toronto Star “We always wondered what he was thinking about whenever the play stopped and he struck his characteristic pose resting his chin on his goal stick. Now we know. He was composing one of the best hockey books ever written …. There is a ‘you are there’ quality to the prose as the author-goalie lets you see everything through his eyes, spicing his vivid descriptions with personal reflections and observations …. The Game succeeds both as an inside look at hockey and a portrait of an articulate athlete who knew when to quit.” —Winnipeg Free Press “The Game is a brilliant adventure into ourselves. It makes all other books about the sport look preliminary.” —Calgary Herald “A book about Ken Dryden, about Quebec, about the rest of Canada, and most of all, a loving book about a special sport.” —New York Times “The best Canadian sports book in years.” —Calgary Sun “An incredible memoir, a poetic journey through the life of Les Canadiens. It rises above being just a book about hockey. It’s a book about people, the fragile, delicate moments on the edge of fame and glory, failure and disillusionment. Dryden’s The Game is the complete hockey book.” —Windsor Star “As Dryden reminisces, we are presented with a portrait, in broad and vivid strokes, of the players who comprised the best team in professional hockey…. -

Legacy Hockey Stars Cards for HOCKEY BLAST
2 ✁ 3 ★ 4 ✁ 5 ✁ 6 ✁ ✁ 7 ✁ ✁ 8 ✁ ✰ 9 ✁ Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Bill King Hap Red Tom Gus Kenny Jimmy BARILKO CLANCY DAY HORNER JOHNSON MORTSON REARDON THOMSON D • Legacy All-Stars D • Legacy All-Stars D/W • Legacy All-Stars D • Legacy All-Stars D • Legacy All-Stars D • Legacy All-Stars D • Legacy All-Stars D • Legacy All-Stars HIT SPEED ▼ HIT HIT HIT HIT HIT HIT HIT ■ SKILL SMART SKILL ■ SMART ■ SKILL SMART SKILL ■ SMART ■ ■ SMART POWER STAR POWER STAR POWER POWER POWER POWER POWER FO FIGHT INJ PEN FO FIGHT INJ PEN FO FIGHT INJ PEN FO FIGHT INJ PEN FO FIGHT INJ PEN FO FIGHT INJ PEN FO FIGHT INJ PEN FO FIGHT INJ PEN 4 A 2.0 3 A 1.5 3 A 1.0 5 A 2.5 2 A 1.0 4 A 1.5 5 B 2.0 3 B 1.0 ### ★★ ★★★ ### ★✰ ✰★ ### ★★★ ★★ ### ★★ ✰★ ### ★★ ✰ ### ★ ★ ### ✰ ✰★★ ### ★★ ★★ Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Skater_DataSHOT ASST Toe Lorne Gordie Busher Aurele Howie Bert Sweeney BLAKE CARR DRILLON JACKSON JOLIAT MEEKER OLMSTEAD SCHRINER W • Legacy All-Stars W • Legacy All-Stars W • Legacy All-Stars W • Legacy All-Stars W • Legacy All-Stars W • Legacy All-Stars W • Legacy All-Stars W • Legacy All-Stars SPEED ▼ SPEED ▼ SPEED ▼ SPEED ▼ HIT SPEED HIT ▼ HIT SPEED ▼ SKILL ✪ SMART SKILL SMART SKILL ✪ SMART SKILL SKILL SMART SKILL ● SMART ■ SMART SKILL SMART STAR STAR STAR STAR POWER STAR POWER STAR FO FIGHT INJ -

Turning Points
TURNING POINTS Ten Landmark Moments That Defined California’s Seals BY STEVE CURRIER he franchise best known as the California against the Seattle Totems, the Seals faced another 3–1 Golden Seals existed from 1961 to 1978, in various deficit, even though the entire series was played at the Tleagues, under different names and in numerous Cow Palace in San Francisco due to a scheduling con- locations. Its first five years were spent in the minor-pro flict in Seattle. The Seals rallied to win the next two con- Western Hockey League (whl) as the San Francisco tests and force a climactic seventh game. Seals. In 1966, the club was purchased by a group led by Before a league-record crowd of 12,404, the Seals fell Barry van Gerbig, relocated to Oakland and renamed behind 2–0 in the second period, but San Francisco’s the California Seals; it later became one of the nhl’s 1967 Duke Edmundson and Moe Mantha drew the two teams expansion franchises. After an early, lukewarm recep- even before the period-ending buzzer sounded. Danny tion from Oakland fans, the team was rechristened the Belisle then put the Seals up 3–2 at 5:09 of the third, but Oakland Seals in December 1967. When Charles O. Fin - Seattle’s Jim Powers tied it up just a minute later, forcing ley purchased the struggling franchise in 1970, he overtime for the fourth time in the series. decided, two games into the new season, to rename the Throughout the overtime period, it sounded as though team the California Golden Seals, which is the name that fans were stomping their feet or pounding their fists on stuck until the team moved to Cleveland in 1976. -
1987 SC Playoff Summaries
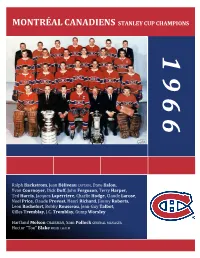
MONTRÉAL CANADIENS STANLEY CUP CHAMPIONS 1 9 6 6 Ralph Backstrom, Jean Béliveau CAPTAIN, Dave Balon, Yvan Cournoyer, Dick Duff, John Ferguson, Terry Harper, Ted Harris, Jacques Laperriere, Charlie Hodge, Claude Larose, Noel Price, Claude Provost, Henri Richard, Jimmy Roberts, Leon Rochefort, Bobby Rousseau, Jean-Guy Talbot, Gilles Tremblay, J.C. Tremblay, Gump Worsley Hartland Molson CHAIRMAN, Sam Pollock GENERAL MANAGER Hector “Toe” Blake HEAD COACH © Steve Lansky 2010 bigmouthsports.com NHL and the word mark and image of the Stanley Cup are registered trademarks and the NHL Shield and NHL Conference logos are trademarks of the National Hockey League. All NHL logos and marks and NHL team logos and marks as well as all other proprietary materials depicted herein are the property of the NHL and the respective NHL teams and may not be reproduced without the prior written consent of NHL Enterprises, L.P. Copyright © 2010 National Hockey League. All Rights Reserved. 1966 STANLEY CUP SEMI-FINAL 1 MONTRÉAL CANADIENS 90 v. 3 TORONTO MAPLE LEAFS 79 GM SAM POLLOCK, HC HECTOR ‘TOE’ BLAKE v. GM PUNCH IMLACH, HC PUNCH IMLACH CANADIENS SWEEP SERIES Thursday, April 7 Saturday, April 9 TORONTO 3 @ MONTREAL 4 TORONTO 0 @ MONTREAL 2 FIRST PERIOD FIRST PERIOD 1. TORONTO, Eddie Shack 1 (Bob Pulford, Red Kelly) 2:12 NO SCORING 2. MONTREAL, J.C. Tremblay 1 (unassisted) 12:06 PPG 3. TORONTO, Frank Mahovlich 1 (George Armstrong, Larry Hillman) 18:06 PPG Penalties – Horton T 0:34, Larose M 3:55, Baun T Pulford T (10-minute misconduct) 7:33, Stemkowski T 10:11, Horton T Hillman T Harris M J.C. -
2017 in the Game Stickwork Hockey Final Checklist
2017 In The Game Stickwork Hockey Final Checklist Set Subset Name Checklist Bronze Red Platinum Silver Gold Emerald Plates 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Adam Oates GAT-01 25 12 5 3 1 2 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Al MacInnis GAT-02 25 12 5 3 1 4 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Alex Delvecchio GAT-03 25 9 5 3 1 1 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Alexander Ovechkin GAT-04 25 12 5 3 1 3 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Andy Bathgate GAT-05 25 12 5 3 1 4 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Bob Gainey GAT-06 25 12 5 3 1 4 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Bobby Clarke GAT-07 25 9 5 3 1 4 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Bobby Hull GAT-08 25 12 5 3 1 4 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Bobby Orr GAT-09 25 12 5 3 1 5 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Borje Salming GAT-10 25 12 5 3 1 3 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Brad Park GAT-11 25 9 5 3 1 4 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Brendan Shanahan GAT-12 25 12 5 3 1 1 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Chris Chelios GAT-13 25 12 5 3 1 4 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Darryl Sittler GAT-14 25 12 5 3 1 3 NO 2017 In The Game Stickwork Hockey 100 Greatest of All-Time Dave Keon GAT-15 25 12 5 3 1 1 NO -
Sport-Scan Daily Brief
SPORT-SCAN DAILY BRIEF NHL 5/16/2020 Anaheim Ducks Montreal Canadiens 1184601 Q&A: Ducks prospect Brayden Tracey adjusted in a 1184628 Max Domi’s future with the Canadiens is stuck between a season of major change rock and a hard place Boston Bruins Nashville Predators 1184602 This Date in Bruins History: B's lose Game 1 of 1990 1184629 Predators' Ryan Ellis goes from defenseman to handyman Stanley Cup Final in 3OT during quarantine 1184603 Bruins' historic playoff collapse vs. Flyers still stings a 1184630 Catching up with Tomas Vokoun, from expansion in decade later Nashville to the Panthers 1184604 The accidental Bruin: How Chris Wagner beat the odds to join his hometown team New Jersey Devils 1184631 Bad season and all, Devils’ P.K. Subban brags he’s still Buffalo Sabres one of NHL’s best blueliners 1184605 Former Sabres captain Jason Pominville hired as youth hockey coach in Quebec NHL 1184606 MSG's 'Sabres Classics' to hold Greatest Moments Week 1184632 CHL settles lawsuits filed by current and former players 1184607 Assistant GM Randy Sexton shares how the Sabres are over backpay approaching an unusual draft 1184608 What kind of impact could Dylan Cozens have if he joins Ottawa Senators the Sabres next season? 1184633 Some NHL general managers aren't willing to think outside the box Calgary Flames 1184634 Work out like an Ottawa Senators player – at home 1184609 ‘We’ll walk together forever’: An oral history of 1184635 Finding an NHL comparable for 10 of the Senators’ best Lightning-Flames, Game 7 prospects Chicago Blackhawks Philadelphia -

In Defence of the Classic Tudor Page 1 of 3
In defence of the classic Tudor Page 1 of 3 Publication: National Post; Date:2004 Dec 11; Section:Post Homes; Page Number: PH4 H OM E O F T H E W E E K In defence of the classic Tudor B Y C O N N I E A DA I R National Post 5010 Sideline 8 Rd. (Durham Road 5 and Sideline 8) Asking price: $1.189-million Taxes: $5,742 (2003) The Boomer, legendary Toronto Maple Leafs defenceman Bobby Baun, once owned this English Tudor home in the hamlet of Claremont. Baun, best known for scoring the winning goal in an overtime game against the Detroit Red Wings in the 1964 Stanley Cup Final (he played an overtime period with a broken ankle), became a Maple Leaf in 1956, the same year this Claremont home was built. An aficionado of English Tudor homes, Baun purchased it in about 1991. The current owners bought it in 1998 and renovated the home extensively in 2001, says listing agent Richard Ling, of Harvey Kalles Real Estate Ltd. The 12-room stone-and-wood home offers more than 6,000 square feet of living space with soaring ceilings, a grand foyer with floating oak stairs, interior water fountains, a floor-to-ceiling stone fireplace, slate and ceramic floors. The master suite is in a separate wing from the other bedrooms, Mr. Ling says. The more than 1,000-sq.-ft. master suite occupies the north wing, and features a built-in closet and a six-piece ensuite bathroom. The guest suite, which consists of two bedrooms and a sitting room, is in the south wing on the second level.