Bulletin May 2003
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Matas Bibliography
Matas Bibliography 1. This is a brief explanation of the information in the different note fields that encountered in this bibliography. Notes: indicates where the citation came from. Several different bibliographies were consulted to create this master list, including Dr Matas’ personal bibliography, and bibliographies compiled by various librarians and physicians throughout the 20th century. LIBRARY HAS: indicates Matas Library holdings. If there is no LIBRARY HAS: then the citation has not been verified as being possessed by Matas library. Some call numbers where placed after Note: or LIBRARY HAS: field, this means it is in our library. This bibliography is a copy of 2002 PDF bibliography compiled by Matas Librarians. It was reworked by Maureen Knapp in March 2014 to reduce PDF file size. For assistance email [email protected] 2. ( 1) Address on the History and Significance of the Violet Hart Award for Outstanding Achievements in Vascular Surgery; and (2) Presentation and Citation of Dr. Mont R. Reid; first recipient of the "Matas Medal" of the Violet Hart Fund. Report of proceedings at Dixon Hall, N.O., January 23. American Journal of Surgery. 1934; 24(1, April):1-35. Notes: Matas- His Chronologic Bibliography... 3. 1915-1941 and the years between. With special references to the antagonism and perpetual menace of the old imperial and the new Nazi Germany to the peace and security of the United States. Mississippi Doctor. 1941 Jul; 19:55-67. 4. Abstract from the Acceptance of the President of the American College of Surgeons upon the occasion of the dedication of the Murphy Memorial-quoted from the Chicago Daily Tribune. -

A Century of International Progress and Tradition in Surgery
Liebermann-Meffert, White A Century of International Progress and Tradition in Surgery A Century of International Progress and Tradition in Surgery An Illustrated History of the International Society of Surgery D. Liebermann-Meffert, H.White In collaboration with H.J. Stein, M. Feith and V. Bertschi Kaden Verlag Heidelberg IV liebermann-meffert · white Die Deutsche Bibliothek – CIP-Einheitsaufnahme Liebermann-Meffert, Dorothea; White, Harvey: A Century of International Progress and Tradition in Surgery; An Illustrated History of the International Society of Surgery / by Dorothea Liebermann-Meffert, Harvey White. In collab. with H.J. Stein, M. Feith, V. Bertschi. – Heidelberg : Kaden, 2001 ISBN 3-922777-42-2 © 2001 Kaden Verlag, Heidelberg, Germany Typesetting: Ch. Molter, Kaden Verlag, 69115 Heidelberg, Germany Printing and Binding: Wesel Druckerei GmbH & Co. KG, 76534 Baden-Baden, Germany ISBN 3-922777-42-2 This book is protected by copyright. Reprinting, translation, copying of illustrations, copying by means of photomechanical devices or similar, storage in data processing systems or on electronic data storage media, as well as provision of the content in the Internet or other systems of communication only with previous written permission from the publisher. Any infringement of these rights, even in the form of excerpts, is punishable by law. a century of international progress and tradition in surgery V Foreword As the International Surgical Society (ISS)/Societé Internationale de Chirurgie (SIC) celebrates its centenary at this 39th Congress in Brussels, the city where the Society was founded and where its Secretariat was located for many years, it is an opportune time for a history of the Society to be published. -
Rudolph Matas Library of the Health Sciences
Rudolph Matas Library of the Health Sciences Index of Diplomas and Certificates Listed by name of individual awarded the diploma or certificate. Click on the letter to navigate quickly to that section. A-C D-L M-N O-R S-Z --------------------------------------------------------------------- ----------- A-C Back to Top --------------------------------------------------------------------- ----------- Beaumont, William. Appointment, Surgeon, United States Army. 1826 Nov 26. 14x18. Berthelot, William H. Diploma, Doctor of Medicine, University of Louisiana Medical Department. 1856. 20x24. Bonner, Samuel L. Diploma, Doctor of Medicine, University of Louisiana Medical Department. 1860 Mar 20. 20x24. Bonner, William. Diploma, Doctor of Medicine, University of Louisiana Medical Department. 1851. 20x24. Bowman, Martin Luther. Biographical information. 14x18. Bowman, Martin C. Diploma, Doctor of Medicine, University of Louisiana Medical Department. 1878. 20x24. Bowman, Martin Luther. Translation of diploma. 20x24. Brickell, William Edwin. Certificate for passing medical examinations, University of Pennsylvania. 1853. 20x24. Brickell, William Edwin. Certificate of attendance, Edward Parrish's School of Practical Pharmacy, Philadelphia. 1853 Oct 10. 20x24. Brickell, William Edwin. Certificate of attendance, The Obstetrics Institute of Philadelphia. 1854 Jan 24. 20x24. Brickell, William Edwin. Diploma, Doctor in Medical Arts, University of Pennsylvania. 1853. 24x31. Burthe, Joseph Leopold. Certificate of attendance, Medical Department of Tulane University. 1896 Apr 1. Course in Microscopical and Bacteriological Laboratory. 11x14. Burthe, Joseph L. Certificate of externe student, Charity Hospital. 1896 Apr 1. 16x20. Burthe, Joseph Leopold. Certificate of residency, Charity Hospital. 1897. 11x14. Burthe, Joseph Leopold. Certificate, Charity Hospital Ambulance Service, Ambulance Surgeon. 1897 Apr 5. 11x14. Burthe, Joseph Leopold. Certificate to practice medicine, Board of Health, State of Louisiana. 1897 Apr 20. -

William Stewart Halsted in the History of American Surgery
醫 史 學 제12권 제1호(통권 제22호) 2003년 6월 Korean J Med Hist 12∶ 66– 87 June 2003 大韓醫史學會 ISSN 1225– 505X W illiam S tew art Hals ted in the His tory of Am erican S urg ery KIM Ock– Joo* The Johns Hopkins Hospital founded in 1889 inspiring teachers most of whom had research and the Johns Hopkins Medical School opened in experience in European medical centers medical 1893 provided young men and women with a students were trained as medical scientists both in unique environment for medical research For the laboratories and at the bedside The influence of first time in America a teaching hospital was the Johns Hopkins Hospital and University on established as an integral part of a medical school American medicine and medical education was far within a university 1) The hospital staff and reaching 2) The Johns Hopkins stimulated other medical school faculty played an important role in universities and hospitals to adopt research– introducing the institutions and ideals of scientific oriented medical education 3) Many investigators research to the United States from Europe Under trained at Johns Hopkins established similar * Department of Medical Education, College of Medicine, Korea University 1) The Johns Hopkins Hospital was unique compared to other teaching hospitals in America In successive papers Kenneth Ludmerer has shown that teaching hospitals in America arose mainly from unions between voluntary hospitals founded in the nineteenth century and university medical schools in the 1910s and 1920s He claims that the primary reason for the backwardness -

The Complex Life of Rudolph Matas
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector The complex life of Rudolph Matas John Ochsner, MD, New Orleans, La I am fortunate to have known Dr Matas for many between Brownsville, Tex, and New Orleans. Using years. I can vividly recall as a child spending many days Butler’s position, they were able to get these supplies during the Mardi Gras season at his home to review the through the Union blockade. After many trips, Narciso parades. I also had the opportunity to read to him later in became a very wealthy man. Needless to say, the life when his eyesight failed. Confederate New Orleanians were not fond of Narciso The life of Rudolph Matas was unique and compli- Matas. They felt he was a traitor. Before the end of the cated.1 He was one of the most scholarly individuals who war, Narciso took his fortune and family back to ever lived and was a medical pioneer extraordinaire. Catalonia. Unfortunately, he invested his money in a rail- Because of time constraints, I will not dwell on his profes- way project that was wrecked by the Spanish political sional life, but highlight his personal life, which unfortu- empire. Therefore, he needed to return to America in the nately was filled with tragedies and heartaches. To hope that he could recoup his fortune. At this time in New understand the man, one must also understand his family. Orleans, the yellow fever epidemic was rampant, and Rudolph Matas’ father, Narciso Matas, was born in the Narciso began working with all available medical person- Catalonian region of Spain. -

Department of Surgery General Surgery Residency Program
Department of Surgery General Surgery Residency Program Chairman: Fabrizio Michelassi, MD, FACS Vice Chair of Education: Thomas J. Fahey, III, MD, FACS Program Director: Thomas J. Fahey, III, MD, FACS Associate Program Director: Abraham Po-Han Houng, MD Program Manager: David Fehling, MA General Surgery Residency Coordinator: Jennifer Cleaver Welcome from the Chairman We are delighted and proud to be an active part of our institution, which is among the top- ranked clinical and medical research centers in the country. Our affiliation with a major academic medical center underscores our departments three-pronged mission: to provide the highest quality of compassionate care, to educate the surgeons of tomorrow, and to pursue groundbreaking research. As members of the clinical staff of NewYork-Presbyterian and Weill Cornell Medicine, our team of experienced surgeons practice at the forefront of their respective specialties, offering patients outstanding, humane and personalized care. As faculty of Weill Cornell Medical College, these physicians are educating future generations of surgeons and advancing state-of-the-art surgical treatment. The history of surgery at the New York Hospital, the second oldest hospital in the United States, reflects the evolution of surgery in America, and is marked by some of the most extraordinary achievements in medicine. The New York Hospital was the cradle of early surgical developments and instruction in America, earning a worldwide reputation for excellence and innovation. Many of today’s practices and techniques arose from our institution. Our department continues to build upon our rich legacy of surgical innovations, making important contributions to the advancement of new surgical procedures. -

Warren Commission, Volume XVII: CE
?rosidont =rived in "'.:0 1":crgency Room .: exactly 12 :43 7 ..^... in his limousine . I:o was in the back seat, Gov. Ccaally was in the front seat of the same car, Gov . Connally was brou£ht out firstand and was put in room two . ?resident was brought out next put in room one . Dr . Clark pronci :nCad the ?residort dead at the 1 p .m . exactly . All of "_esident's bolor2ings except his watch were given to the Sccrot Service . Isis W---Ch was given to Xr . 0 . P. -i a iio loft the Emergency Room, the president, at about 2 p .m . in an O'Neal ambulance . ite was put :r. a bronze colored plastic casket after hoing wrapped in a blanket and was taken out of the hospital . lie was rc:oved from the hospital, . The Gov. was taken from the Emergency Room to the Operating Room . Tha President's wife ro .-"us,:~ :o take off her bloc" grove ., clothes . She did take a tow.: and wipe her face . She took her wedding ring of- r.nc and placed. it on one of tha President's fingers. f 561 COMMISSION EXHIBIT 392 Kasi - S 20, the 2n! W H_ 1 ns in cha ,._at of his of L"O in this C". to Saa t'.1z Zzesident was Dr . jx as Ca:.:.icQ, L 3~"ido= in General surgery. !1Z . Carrico noted thL zo have .. -~a,, agGnt- raspirazory- efforts . K'a COwld a narrzbLat but found in pulse or blood to -:-- ~-ascnt . - t::-:c Z:-.c~a Z- n- ' \:a ew-tarra! wounds, one in of the in zh~ coci?ital ~:agion of terior neck, the other the were noted . -

Ronald V. Maier, MD President 2000–2002
30 Ronald v. Maier, MD President 2000–2002 Dr. David H. Livingston When did you decide to do trauma and critical care as a career path? Dr. Ronald V. Maier Well, as you know, I went to Duke Medical School and, until my fourth year, I was planning on joining the new specialty of interventional cardiology because I liked working with my hands and it was an exciting and interesting new field. In addition, my favorite mentor and role mod- el at Duke was Eugene Stead, MD, who was an internationally famous cardiologist and superb clinician of the day. However, if there is a theme that should run through my message today it would be my increasing recognition of the relevance of good mentorship and how important it is for anyone’s career. So I had planned on being a cardiologist but, in my fourth year of medical school, I did an elective on surgery—Dr. David Sabiston’s service—with Drs. Bob Anderson, Bill Gay, Bill Devries, Walt Wolf, Brad Rogers and other future stars in cardiothoracic surgery. It was an unbelievable experience, mainly because of the quality of the residents that were on the service, who have almost all gone on to be chairmen and academic leaders. Again, role models and mentors were critical. They convinced me, by their example, that my personality fit with surgery. So I switched fields at the last second and applied to general surgery. A very difficult decision came when Dr. David Sabiston asked me to stay at Duke but I was also accepted at Parkland Memorial Hospital, working for Dr. -
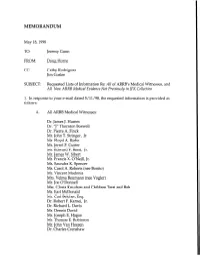
DH Memo: Requested Lists of Information
MEMORANDUM May I&l998 TO: Jeremy Gunn FROM: Doug Horne cc: Cathy Rodriguez Jim Goslee SUBJECT: Requested Lists of Information Re: All of ARRB’s Medical Witnesses, and All New ARRB Medical Evidence Not Previously in JFK Collection 1. In response to your e-mail dated 5/11/98, the requested information is provided as follows: A. All ARRB Medical Witnesses: Dr. James J. Humes Dr. “J” Thornton Boswell Dr. Pierre A. Finck Mr. John T. Stringer, Jr. Mr. Floyd A. Riebe Mr. Jerrol F. Custer Mr. Edward F. Reed, Jr. Mr. James W. Sibert Mr. Francis X. O’Neill, Jr. Ms. Saundra K. Spencer Ms. Carol A. Roberts (nee Bonito) Mr. Vincent Madonia Mrs. Velma Reumann (nee Vogler) Mr. Joe O’Donnell Mrs. Gloria Knudsen and Children Terri and Bob Mr. Earl McDonald Mr. Carl Belcher, Esq. Dr. Robert F. Karnei, Jr. Dr. Richard L. Davis Mr. Dennis David Mr. Joseph E. Hagan Mr. Thomas E. Robinson Mr. John Van Hoesen Dr. Charles Crenshaw 2 Ms. Audrey Bell (R.N.) Dr. Robert G. Grossman Dr. Paul Peters Dr. Leonard D. Saslaw, Ph.D. Mr. Robert I. Bouck Mr. Floyd Boring Mr. Donald A. Purdy, Jr., Esq. Mr. Ken Vrtacnik Mr. James Mastrovito Mr. Michael Rhode Ms. Jamie B. Taylor Children of George Burkley (Ms. Isabel Starling, Mr. Richard Burkley, Mr. George Burkley, and Ms. Nancy Denlea) Dr. Janet Travel1 Dr. James B. Rhoads, Ph.D. Ms. Eve Carr (nee Patricia Eve Walkling) Mr. Roger Boyajian Ms. Cindy C. Smolovik Ms. Lois A. Dillard Dr. John Ebersole (posthumously) B. All New ARRB Medical Evidence Not Previously in JFK Collection (Transcripts of Sworn Testimony from Depositions -

Conspiracy- - Of· Si1lence
. I JFK CONSPIRACY- - OF· SI1LENCE Charles A. Crenshaw, M.D. with Jens Hansen and J� Gary Shaw Introduction by John H. Davis (]) A SIGNET BOOK SIGNET Published by the Penguin Group Penguin Books USA Inc., 375 Hudson Street, New York, New York 10014, U.S.A. Penguin Books Ltd, 27 Wrights Lane, London WS STZ, England Penguin Books Australia Ltd, Ringwood, Victoria, Australia Penguin Books Canada Ltd, 10 Alcorn Avenue, Toronto, Ontario, Canada M4V 3B2 Penguin Books (N.Z.) Ltd, 182-190 Wairau Road, Auckland 10, New Zealand Penguin Books Ltd, Registered Offices: Harmondsworth, Middlesex, England Fust published by Signet, an imprint of New American Ubrary, a division of Penguin Books USA Inc. Fust Printing, April, 1992 10 9 8 7 6 5 4 3 Copyright C Dr. Charles A. Crenshaw, lens Hansen, and J. Gary Shaw, 1992 Introductioncopyright C John H. Davis, 1992 AU rights reserved (/)REGISTERED TRADEMARK-MARCA REOISTRADA Printed in the United States of America Without limitingthe rights under copyright reserved above, no part of this publication may be reproduced, stored in or introduced into a retrieval system, or transmitted, in any form, or by any means (electronic, mechanical, photocopying, recording, or otherwise), without the prior written permission of both the copyright owner and the above publisher of this book. BOOKS ARE AVAILABLE AT QUANTITY DISCOUNI'S WHEN USED TO PROMOTE PRODUCI'S OR SERVICES. FOR INFORMATION PLEASE WRITE TO PREMIUM MARKETING DIVISION, PENGUIN BOOKS USA INC., 375 HUDSON STREET, NEW YORK, NEW YORK 10014. · If you purchased this book without a cover you should be aware that this book is stolen property. -

Alton Ochsner, MD: Physician
Ochsner Profiles Alton Ochsner, MD: Physician Hector O. Ventura, MD Ochsner Heart and Vascular Institute, Department of Cardiology, Ochsner Clinic Foundation, New Orleans, LA he contributions of Alton Ochsner (1) to the principles and practice of medicine are internationally recognized. THis professional legacy has been recorded in numerous manuscripts and books during his long and fruitful medical career, and his personal legacy has been documented in multiple biographies. It is, therefore, both an honor and a daunting task to write on the life and career of Dr. Alton Ochsner for Ochsner Profiles. It is an honor because my name will be associated with others who have written about this renowned figure and a daunting task because I have to reach into Dr. Ochsner’s mind and heart through his interviews and through the minds and hearts of those who knew him on a personal level. I hope that my exploration of Alton Ochsner’s achievements and personality will lend tribute to one of the greatest figures in medicine. Life and Medical Career In 1881, Alton Ochsner’s parents, Edward Philip (EP) Alton Ochsner, MD Ochsner and Clara Leda Shontz, left Bear Valley, Wisconsin, for Kimball, South Dakota, a new community on the railroad line. for others’ shortcomings.” Alton Ochsner simply said, “I loved Kimball was named in honor of Edmund Kimball, father of the my mother” (2). railroad surveyor Frank Kimball. From 1881 and for the next 4 School lessons were easy for Dr. Ochsner. In the early grades decades the Ochsner family would be prominent in the business, he finished his assignments before anybody else, then he looked political, social, and religious life of Kimball, SD. -

The Haisted Mastectomy:Present
Refer to: Bland CS: The Halsted mastectomy: Present illness and, past history. West J Med 134:549-555, Jun 1981 Special Article The Haisted Mastectomy: Present Illness and Past History CORDELIA SHAW BLAND, Topanga, California The Halsted mastectomy put American surgeons of the late 19th century ahead of competing general practitioners at home and the preeminent German surgeons abroad. It thus served economic and nationalistic drives in the nascent specialty of surgery. Such socioemotional forces-and not scientific principles-may explain why Halsted's expansion of the mastectomy to include the pectoral muscles became lastingly institutionalized. 'I WENT TO THE hospital feeling peifectly healthy serves that loss of a breast is as devastating for and came out grotesquely mutilated-a mental some women as loss of the penis is for a man.2 and physical wreck." Nor has the operation's greater trauma been These are the words of a woman who under- justified by greater cure. Before the National went a radical mastectomy in 1971. Although Cancer Institute's (NCI) initiation of the first such anguish is customarily masked by the smil- controlled study in 1971, no comparative findings ing American version of the stiff upper lip (beau- existed. Surgeon C. D. Haagensen's substantial tifully modeled by former first and second ladies prospective study dating from 1935 had no con- Betty Ford and Happy Rockefeller), this woman trol group,3 and all retrospective studies have may well voice the innermost-even if transient- been essentially anecdotal, small-scale counts of feelings of millions of women subjected to a radi- apples mixed with oranges." cal mastectomy since it was introduced in 1882 by The NCI study, directed by surgeon Bernard American surgeon William S.