Robbins Medal Speech
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

TESTIMONY Peter J. Hotez MD, Phd President, Sabin Vaccine Institute
TESTIMONY Peter J. Hotez MD, PhD President, Sabin Vaccine Institute “The Growing Threat of Cholera and Other Diseases in the Middle East” Subcommittee on Africa, Global Health, Global Human Rights, and International Organizations Committee on Foreign Affairs United States House of Representatives March 2, 2016 Mr. Chairman and Members of the Subcommittee, thank you for the opportunity to speak with you today. I am Peter Hotez, a biomedical scientist and pediatrician. I am the dean of the National School of Tropical Medicine at Baylor College of Medicine and also the Texas Children’s Hospital Endowed Chair in Tropical Pediatrics based at the Texas Medical Center in Houston. I am also past president of the American Society of Tropical Medicine and Hygiene, and currently serve as President of the Sabin Vaccine Institute, a non-profit which develops vaccines for neglected tropical diseases (NTDs) through a product development partnership (PDP) model. This year I am also serving as US Science Envoy for the State Department and White House Office of Science and Technology Policy focusing on the urgency to develop vaccines for diseases that are emerging in the Middle East and North Africa due to the breakdowns in health systems in the ISIS occupied conflict zones in Syria, Iraq, Libya, and also Yemen. In my submitted written testimony I highlighted some of the successes in US global health policy, many of which can be attributed to the hard work of this Subcommittee working hand in glove with two presidential administrations since 2000. I cite evidence from the Global Burden of Disease Study (GBD) that brings together hundreds of scientists - I am also a part of this - who are measuring the impact of large scale global health programs. -

Sabin in the News Recent Scientific Articles Sabin Vaccine Institute
Home About Us News & Resources Support Sabin Sabin in the News October 2011 The Sabin Report | Volume 13 Issue 2 New York Times article featuring Dr. Peter Hotez's new study on increased Sabin Vaccine Institute Establishes a Houston prevalence of NTDs in Europe. Office Drs. Ciro de Quadros and In September 2011, the Zulfiqar Bhutta highlight Sabin Vaccine Institute the dire need for a dengue established offices in vaccine in an opinion Houston, Texas in the piece for GlobalPost. heart of the city's Texas Medical Center (TMC). The In an interview on Voice of new facilities will house the America Dr. Peter Hotez Sabin Vaccine Institute & focused on NTDs in Sub- Texas Children's Hospital Saharan Africa. Center for Vaccine Development, which will be An article by Dr. Neeraj operated in partnership Mistry was featured in a with Baylor College of special supplemental Medicine Department of section of the USA today, Pediatrics. Sabin Dr. Hotez and team at Sabin's new Houston facility titled "Neglected Diseases President, Dr. Peter J. in Developing Nations". Hotez will direct the new center. In an op-ed for the Houston Chronicle, Dr. The new space includes offices and laboratories through which the Peter Hotez writes about Sabin Vaccine Institute Product Development Partnership (PDP) will the establishment of the advance and strengthen its collaborative work in the field of vaccine new School of Tropical biotechnology. The change is the result of a year-long plan to expand Medicine at Baylor College the scope and depth of the Sabin PDP's partnership and to enhance of Medicine. -

View Introduction and Presentation from Dr
1 We are here tonight to honor and celebrate the outstanding accomplishments and contributions in the field of vaccines of our colleague, our mentor, our friend, Mathu Santosham. Mathu’s professional titles attest to his accomplishments at the highest levels. He is professor of Pediatrics and International Health at Johns Hopkins University and is the Founder and Director of the Center for American Indian Health. 2 He is a widely recognized and celebrated international expert in the area of vaccines against rotavirus, pneumococcus and Haemophilus influenzae type b----the area of work and contribution for which he is being awarded this year’s Sabin Gold Medal Award. But he has also made equally impactful contributions in the area of oral rehydration therapy for diarrheal disease, neonatal survival strategies and more broadly in the area of reducing health disparities for this country’s first nations American Indian people. Millions of deaths around the world have been prevented because of his medical and scientific contributions. Ostensibly this is what we are here to celebrate. 3 Mathu has been celebrated with numerous awards from the Indian Health Service, the Thrasher Research Fund, and the pneumococcal scientific community through the Robert Austrian Award along with awards from his own institution to recognize him from among the many outstanding alumnae of the school. 4 His work and sage advice valued by many around the world, including shown here ABC’s Chief Health and Medical Editor, Dr. Rich Besser. 5 Here with Martin Sheen at the Native Vision Camp in 2012. 6 Here working with Robert Redford on American Indian health disparity issues. -

Peter Hotez, M.D., Ph.D. Biography
Peter Hotez, MD, PhD, FASTMH, FAAP Peter J. Hotez, M.D., Ph.D., is professor of pediatrics and Molecular Virology and Microbiology at Baylor College of Medicine where he is also chief of a new Section of Pediatric Tropical Medicine and founding Dean of the National School of Tropical Medicine. In addition Prof. Hotez is the Texas Children's Hospital Endowed Chair of Tropical Pediatrics, and president of the Sabin Vaccine Institute. He will lead the new Sabin vaccine development program at Texas Children's Hospital and Baylor College of Medicine. He moves to BCM and Texas Children's from The George Washington University, where he has served as a Distinguished Research Professor and the Walter G. Ross Professor and Chair of the Department of Microbiology, Immunology and Tropical Medicine. Dr. Hotez is an internationally-recognized clinician and investigator in neglected tropical diseases and vaccine development. Diseases he studies include hookworm, schistosomiasis, Chagas disease, leishmaniasis, and malaria, among others, impacting hundreds of millions of children and adults worldwide. He obtained his undergraduate degree in molecular biophysics from Yale University in 1980, followed by a Ph.D. degree in biochemical parasitology from Rockefeller University in 1986 and a medical degree from Cornell University in 1987. He completed pediatric residency training at Massachusetts General Hospital from 1987 to 1989 and postdoctoral fellowship training in infectious diseases and molecular parasitology at Yale from 1989 to 1991. Dr. Hotez joined the Yale faculty as an assistant professor of pediatrics in 1992. He became an associate professor in 1995 before moving to the George Washington University as professor and chair in 2000. -

Contributions of Native Americans to the Global Control of Infectious Diseases Mathuram Santosham A,∗, Raymond Reid A, Aruna Chandran A, Eugene V
Vaccine 25 (2007) 2366–2374 Contributions of Native Americans to the global control of infectious diseases Mathuram Santosham a,∗, Raymond Reid a, Aruna Chandran a, Eugene V. Millar a, James P. Watt a, Robert Weatherholtz a, Connie Donaldson a, Janne´ Croll a, Lawrence H. Moulton a, Claudette M. Thompson b, George R. Siber c, Katherine L. O’Brien a a Center for American Indian Health, Department of International Health, Johns Hopkins University, 621 N. Washington Street, Baltimore, MD 21205, United States b Department of Epidemiology, Harvard School of Public Health, 665 Huntington Avenue, Boston, MA 02115, United States c Wyeth Vaccines, 401 North Middletown Road, BH 21101, Pearl River, NY 10965, United States Available online 18 September 2006 Abstract For over a half of a century, Native American populations have participated in numerous studies regarding the epidemiology, prevention and treatment of infectious diseases. These studies have resulted in measures to prevent morbidity and mortality from many infectious diseases. The lessons learned from these studies and their resultant prevention or treatment interventions have been applied around the world, and have had a major impact in the reduction of global childhood morbidity and mortality. © 2006 Elsevier Ltd. All rights reserved. Keywords: Native Americans; Infectious diseases; Clinical trials; Pneumococcus; H. influenzae type b (Hib); Rotavirus; Trachoma; Tuberculosis; BCG Key messages from these studies has been applied in many populations around the world and has met with great success. This In the keynote address (The Robert Austrian Lecture) paper reviews the major achievements in Native Amer- for the 5th International Symposium on Pneumococci and ican health that have been made to date. -

Sabin Vaccine Report
Volume VIII, Number 1 Sabin Vaccine Spring 2005 EPORT The newsletter of the Albert B. Sabin Vaccine InstituteR — dedicated to disease prevention www.sabin.org FDA Clears Human Hookworm Vaccine for Phase I Safety Trials Sabin/GW Researchers Receive Word on Investigational New Drug Status for Vaccine Clinical trials to test the safety of a gin safety trials is a major milestone for in individuals who suffer from hook- first-of-its-kind human hookworm vac- the human hookworm vaccine project,” worm infection.” cine will begin in the Washington, DC Hotez said. “It has taken an amazing Human hookworm infection is caused area in the coming weeks after the U.S. amount of our team’s effort to get us to by parasitic worms that fasten onto the Food and Drug Administration conferred the current stage of vaccine develop- inner layers of the small intestine using investigational new drug status on the ment. Of course, our ultimate goal is to their teeth-like projections and cause vaccine this past January. No current take this research to developing coun- blood loss at the attachment site. vaccine is available to prevent hook- tries where the vaccine will be tested Hookworm disease refers to the iron worm disease, which is one of the most Continued on page 4 common chronic infections of humans with an estimated 740 million cases in The village of Americaninhas, areas of rural poverty in the tropics in a rural part of Minas Gerais and subtropics. state in Brazil, is the focus of a The Human Hookworm Vaccine Ini- field study of hookworm dis- tiative (HHVI) is sponsored by the ease burden, being conducted Albert B. -
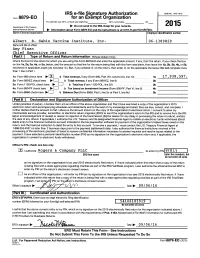
2015 Form 990 Or 990‐EZ
** PUBLIC DISCLOSURE COPY ** Return of Organization Exempt From Income Tax OMB No. 1545-0047 Form 990 Under section 501(c), 527, or 4947(a)(1) of the Internal Revenue Code (except private foundations) 2015 Department of the Treasury | Do not enter social security numbers on this form as it may be made public. Open to Public Internal Revenue Service | Information about Form 990 and its instructions is at www.irs.gov/form990. Inspection A For the 2015 calendar year, or tax year beginning and ending B Check if C Name of organization D Employer identification number applicable: Address change Albert B. Sabin Vaccine Institute, Inc. Name change Doing business as 06-1389829 Initial return Number and street (or P.O. box if mail is not delivered to street address) Room/suite E Telephone number Final return/ 2000 Pennsylvania Avenue, NW 7100 202-842-8610 termin- ated City or town, state or province, country, and ZIP or foreign postal code G Gross receipts $ 17,938,597. Amended return Washington, DC 20006 H(a) Is this a group return Applica- tion F Name and address of principal officer:Amy Finan for subordinates? ~~ Yes X No pending same as C above H(b) Are all subordinates included? Yes No I Tax-exempt status: X 501(c)(3) 501(c) ( )§ (insert no.) 4947(a)(1) or 527 If "No," attach a list. (see instructions) J Website: | www.sabin.org H(c) Group exemption number | K Form of organization: X Corporation Trust Association Other | L Year of formation: 1994 M State of legal domicile: MD Part I Summary 1 Briefly describe the organization's mission or most significant activities: An organization of scientists, researchers, and advocates for a world free of needless suffering. -

Bridging the Innovation Gap for Neglected Tropical Diseases in Mexico
Bol Med Hosp Infant Mex 2011;68(2):138-146 article Bridging the innovation gap for neglected tropical diseases in Mexico: capacity building for the development of a new generation of antipoverty vaccines Maria Elena Bottazzi,1 Eric Dumonteil,2 Jesus G. Valenzuela,3 Miguel Betancourt-Cravioto,4 Roberto Tapia-Conyer,5 and Peter J. Hotez1,6 ABSTRACT The neglected tropical diseases (NTDs) represent a group of chronic parasitic and related infections that promote poverty because of their impact on child development, pregnancy, and worker productivity. The estimated 20 million Mexicans who live below the poverty line suf- fer disproportionately from a high prevalence of neglected tropical diseases such as amebiasis, Chagas disease, dengue, leishmaniasis, soil-transmitted helminth infections, trachoma, and vivax malaria. However, because the NTDs occur predominantly among the poor, new industrial and financial models are required to establish innovative technologies to address these conditions in Mexico and elsewhere in Latin America. In response, the Slim Initiative for Antipoverty Vaccine Development was established to foster a public/private partnership between key academic, government, and industrial institutions in the U.S. and Mexico. Initial emphasis will be placed on developing new vaccines for Chagas disease and leishmaniasis, two of the highest burden NTDs in Mexico and Mesoamerica. Key words: public/private partnerships, vaccines, product development, technology transfer, vaccine manufacture. InTRODuCTIOn infectious diseases that -

A Century of Pneumococcal Vaccination Research in Humans
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector REVIEW 10.1111/j.1469-0691.2012.03943.x A century of pneumococcal vaccination research in humans J. D. Grabenstein1 and K. P. Klugman2,3 1) Merck Vaccines, West Point, PA USA, 2) Rollins School of Public Health and Division of Infectious Diseases, School of Medicine, Emory University, Atlanta, GA, USA and 3) Medical Research Council, National Institute for Communicable Diseases Respiratory and Meningeal Pathogens Research Unit, University of the Witwatersrand, Johannesburg, South Africa Abstract Sir Almroth Wright coordinated the first trial of a whole-cell pneumococcal vaccine in South Africa from 1911 to 1912. Wright started a chain of events that delivered pneumococcal vaccines of increasing clinical and public-health value, as medicine advanced from a vague understanding of the germ theory of disease to today’s rational vaccine design. Early whole-cell pneumococcal vaccines mimicked early typhoid vaccines, as early pneumococcal antisera mimicked the first diphtheria antitoxins. Pneumococcal typing systems developed by Franz Neufeld and others led to serotype-specific whole-cell vaccines. Pivotally, Alphonse Dochez and Oswald Avery isolated pneumo- coccal capsular polysaccharides in 1916–17. Serial refinements permitted Colin MacLeod and Michael Heidelberger to conduct a 1944– 45 clinical trial of quadrivalent pneumococcal polysaccharide vaccine (PPV), demonstrating a high degree of efficacy in soldiers against pneumococcal pneumonia. Two hexavalent PPVs were licensed in 1947, but were little used as clinicians preferred therapy with new antibiotics, rather than pneumococcal disease prevention. Robert Austrian’s recognition of high pneumococcal case-fatality rates, even with antibiotic therapy, led to additional trials in South Africa, the USA and Papua New Guinea, with 14-valent and 23-valent PPVs licensed in 1977 and 1983 for adults and older children. -

Social and Economic Impact Review on Neglected Tropical Diseases
ECONOMIC POLICY / BRIEFING PAPER in conjunction with Social and Economic Impact Review on Neglected Tropical Diseases Jeremiah Norris Carol Adelman Yulya Spantchak Kacie Marano November 2012 Hudson Institute’s Center for Science in Public Policy in conjunction with The Global Network for Neglected Tropical Diseases an initiative of the Sabin Vaccine Institute Social and Economic Impact Review on Neglected Tropical Diseases November 2012 Contributors Jeremiah Norris Carol Adelman Senior Fellow and Director Senior Fellow and Director Center for Science in Public Policy Center for Global Prosperity Yulya Spantchak Kacie Marano Research Fellow and Deputy Director Project Manager and Research Associate Center for Science in Public Policy Center for Science in Public Policy Table of Contents I. Executive Summary……………………………………………………………………...i II. Introduction…………………………………………………………………………….1 III. Background……….…………………………………………………………………...2 IV. The Macroeconomic Impact of NTDs………………………………………………...4 V. Integration…………………………………………………………………………….16 VI. Key NTD Policy Issues……………………………………………………………...19 VII. The Role of the Corporate Sector in NTDs…………………………………………21 VIII. Conclusions and Recommendations……………………………………………….22 Appendix A………………………………………………………………………………25 I. Executive Summary The Hudson Institute’s Center for Science in Public Policy entered into a partnership with the Sabin Vaccine Institute’s Global Network for Neglected Tropical Diseases (GNNTD) to undertake a comprehensive research and policy analysis study on the economic impact of neglected -

Vaccinology in Latin America © 2018 Sabin Vaccine Institute
Vaccinology in Latin America © 2018 Sabin Vaccine Institute. All rights reserved. The material in this document may be freely used for educational or noncommercial purposes, provided that the material is accompanied by an acknowledgement. The Sabin Vaccine Institute is a leading advocate for expanding vaccine access and uptake globally, advancing vaccine research and development, and amplifying vaccine knowledge and innovation. Unlocking the potential of vaccines through partnership, Sabin has built a robust ecosystem of funders, innovators, implementers, practitioners, policy makers and public stakeholders to advance its vision of a future free from preventable diseases. As a non-profit with more than two decades of experience, Sabin is committed to finding solutions that last and extending the full benefits of vaccines to all people, regardless of who they are or where they live. At Sabin, we believe in the power of vaccines to change the world. For more information, visit www.sabin.org and follow us on Twitter, @SabinVaccine. Recommended citation: Andrus et al. Vaccinology in Latin America: A Resource for Immunization Managers. Washington, D.C.: Sabin Vaccine Institute; 2018. Design: Renée Saunders Translation: Silvia Colla Contents Preface ........................................................................................................................................................................................................................1 MODULE 1: EXISTING VACCINES AND VACCINES IN DEVELOPMENT .................................................................................. -

Sabin Vaccine Report
Volume IV, Number 1 Sabin Vaccine June 2001 EPORT The newsletter of the Albert B. Sabin Institute —dedicatedR to disease prevention www.sabin.org Walker’s Cay Colloquium Catalyzes Work on Cancer Vaccines and Immunotherapy 3rd Annual Sabin Institute-Sponsored Meeting Convened in March at Walker’s Cay, Abaco, Bahamas Thirty of the world’s leading cancer of the colloquium, said the meeting “was notherapy to learn from each other and vaccine scientists spent three days in a great success since it provided an ex- to discuss issues that are critical for the intense, unusually open discussions of cellent opportunity for top scientists in improvement of cancer treatments.” Jef- their newest research data and ideas at the field of tumor vaccines and immu- frey Schlom, head of the Laboratory of the Sabin Vaccine Institute’s Tumor Immunology and Biology Third Annual Walker’s Cay Col- at the National Cancer Institute loquium on Cancer Vaccines in also served as co-chair. The March. Their goal was to accel- Walker’s Cay Colloquium follows erate progress toward develop- a peer review format; emphasiz- ment of vaccines to treat and pre- ing an unusually open discussion vent various forms of cancer. of ideas and data so new they have Most of the renowned scientists not yet been published. It is reported learning new informa- multidisciplinary, involving ex- tion that will speed their own re- perts in oncology, immunology, search. Several said they formed microbiology, biochemistry, he- new, multi-institution collabora- matology and several other fields. tions at the meeting. It differs from most scientific Ralph A.