Resident Manual of Trauma to the Face, Head, and Neck
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Orbital Blowout Fractures in Sport
Br J Sp Med 1994; 28(4) Br J Sports Med: first published as 10.1136/bjsm.28.4.272 on 1 December 1994. Downloaded from Orbital blowout fractures in sport N. P. Jones FRCS FCOphth University Department of Ophthalmology, Manchester Royal Eye Hospital, Manchester, UK One-third of orbital blowout fractures are sustained with confirmed pure orbital blowout fractures. during sport. Soccer is most commonly involved. Though Particular attention was paid to blowout fractures visual acuity recovery is usually complete, permanent loss sustained during sport: the sport involved; the of binocular visual field is almost universal. Typically mechanism of injury; the necessary treatment; and high-energy blows by opponent's finger, fist, elbow, knee residual visual problem. or boot are responsible. Injuries to the eye itself may also be sustained and should be looked for. Ocular protection may be feasible in some sports, but the main preventive Results measure to be addressed is the reduction in aggressive play or deliberate injury. During the retrospective study period a total of 62 pure orbital blowout fractures was identified in 62 Keywords: Blowout fracture, sports injury patients. Various forms of assault accounted for 33 (53%) of these patients. Twenty-three fractures (37%) were sustained as a result of sporting activity. The The phenomenon of isolated orbital wall fracture was aetiology of all fractures is shown in Table 1. first recognized in the 19th century1 but the term Of those fractures sustained at sport, Table 2 shows 'blowout' was attributed in 1957 by Converse and the sport involved, the most common being soccer Smith2. -

Diagnoses to Include in the Problem List Whenever Applicable
Diagnoses to include in the problem list whenever applicable Tips: 1. Always say acute or open when applicable 2. Always relate to the original trauma 3. Always include acid-base abnormalities, AKI due to ATN, sodium/osmolality abnormalities 4. Address in the plan of your note 5. Do NOT say possible, potential, likely… Coders can only use a real diagnosis. Make a real diagnosis. Neurological/Psych: Head: 1. Skull fracture of vault – open vs closed 2. Basilar skull fracture 3. Facial fractures 4. Nerve injury____________ 5. LOC – include duration (max duration needed is >24 hrs) and whether they returned to neurological baseline 6. Concussion with or without return to baseline consciousness 7. DAI/severe concussion with or without return to baseline consciousness 8. Type of traumatic brain injury (hemorrhages and contusions) – include size a. Tiny = <0.6 cm b. Small/moderate = 0.6-1 cm c. Large/extensive = >1 cm 9. Cerebral contusion/hemorrhage 10. Cerebral edema 11. Brainstem compression 12. Anoxic brain injury 13. Seizures 14. Brain death Spine: 1. Cervical spine fracture with (complete or incomplete) or without cord injury 2. Thoracic spine fracture with (complete or incomplete) or without cord injury 3. Lumbar spine fracture with (complete or incomplete) or without cord injury 4. Cord syndromes: central, anterior, or Brown-Sequard 5. Paraplegia or quadriplegia (any deficit in the upper extremity is consistent with quadriplegia) Cardiovascular: 1. Acute systolic heart failure 40 2. Acute diastolic heart failure 3. Chronic systolic heart failure 4. Chronic diastolic heart failure 5. Combined heart failure 6. Cardiac injury or vascular injuries 7. -

Lacrimal Obstruction
Yung_edit_final_Layout 1 01/09/2009 15:19 Page 81 Lacrimal Obstruction Proximal Lacrimal Obstruction – A Review Carl Philpott1 and Matthew W Yung2 1. Rhinology and Anterior Skull Base Fellow, St Paul’s Sinus Centre, St Paul’s Hospital, Vancouver; 2. Department of Otolaryngology, Ipswich Hospital NHS Trust Abstract While less common than distal lacrimal obstruction, proximal obstruction causes many cases of epiphora. This article examines the aetiology of proximal lacrimal obstruction and considers current management strategies with reference to recent literature. The Lester Jones tube is the favoured method of dealing with most cases of severe proximal obstruction; other methods have been tried with less success. Keywords Proximal lacrimal obstruction, epiphora, canalicular blockage, Lester Jones tube Disclosure: The authors have no conflicts of interest to declare. Received: 31 March 2009 Accepted: 14 April 2009 DOI: 10.17925/EOR.2009.03.01.81 Correspondence: Matthew W Yung, The Ipswich Hospital, Heath Road, Ipswich, Suffolk, IP4 5PD, UK. E: [email protected] Obstruction of the lacrimal apparatus commonly causes sufferers to dominant fashion.3 Where absence of the punctum and papilla present with symptoms of epiphora, for which they are commonly (congenital punctal agenesis) occurs, it is likely that more distal parts referred to ophthalmology departments. In those units where of the lacrimal apparatus are obliterated. collaboration with otorhinolaryngology occurs, the distal site of obstruction is usually dealt with. -

Cervical Spine Injury Risk Factors in Children with Blunt Trauma Julie C
Cervical Spine Injury Risk Factors in Children With Blunt Trauma Julie C. Leonard, MD, MPH,a Lorin R. Browne, DO,b Fahd A. Ahmad, MD, MSCI,c Hamilton Schwartz, MD, MEd,d Michael Wallendorf, PhD,e Jeffrey R. Leonard, MD,f E. Brooke Lerner, PhD,b Nathan Kuppermann, MD, MPHg BACKGROUND: Adult prediction rules for cervical spine injury (CSI) exist; however, pediatric rules abstract do not. Our objectives were to determine test accuracies of retrospectively identified CSI risk factors in a prospective pediatric cohort and compare them to a de novo risk model. METHODS: We conducted a 4-center, prospective observational study of children 0 to 17 years old who experienced blunt trauma and underwent emergency medical services scene response, trauma evaluation, and/or cervical imaging. Emergency department providers recorded CSI risk factors. CSIs were classified by reviewing imaging, consultations, and/or telephone follow-up. We calculated bivariable relative risks, multivariable odds ratios, and test characteristics for the retrospective risk model and a de novo model. RESULTS: Of 4091 enrolled children, 74 (1.8%) had CSIs. Fourteen factors had bivariable associations with CSIs: diving, axial load, clotheslining, loss of consciousness, neck pain, inability to move neck, altered mental status, signs of basilar skull fracture, torso injury, thoracic injury, intubation, respiratory distress, decreased oxygen saturation, and neurologic deficits. The retrospective model (high-risk motor vehicle crash, diving, predisposing condition, neck pain, decreased neck mobility (report or exam), altered mental status, neurologic deficits, or torso injury) was 90.5% (95% confidence interval: 83.9%–97.2%) sensitive and 45.6% (44.0%–47.1%) specific for CSIs. -

Ciliary Zonule Sclera (Suspensory Choroid Ligament)
ACTIVITIES Complete Diagrams PNS 18 and 19 Complete PNS 23 Worksheet 3 #1 only Complete PNS 24 Practice Quiz THE SPECIAL SENSES Introduction Vision RECEPTORS Structures designed to respond to stimuli Variable complexity GENERAL PROPERTIES OF RECEPTORS Transducers Receptor potential Generator potential GENERAL PROPERTIES OF RECEPTORS Stimulus causing receptor potentials Generator potential in afferent neuron Nerve impulse SENSATION AND PERCEPTION Stimulatory input Conscious level = perception Awareness = sensation GENERAL PROPERTIES OF RECEPTORS Information conveyed by receptors . Modality . Location . Intensity . Duration ADAPTATION Reduction in rate of impulse transmission when stimulus is prolonged CLASSIFICATION OF RECEPTORS Stimulus Modality . Chemoreceptors . Thermoreceptors . Nociceptors . Mechanoreceptors . Photoreceptors CLASSIFICATION OF RECEPTORS Origin of stimuli . Exteroceptors . Interoceptors . Proprioceptors SPECIAL SENSES Vision Hearing Olfaction Gustation VISION INTRODUCTION 70% of all sensory receptors are in the eye Nearly half of the cerebral cortex is involved in processing visual information Optic nerve is one of body’s largest nerve tracts VISION INTRODUCTION The eye is a photoreceptor organ Refraction Conversion (transduction) of light into AP’s Information is interpreted in cerebral cortex Eyebrow Eyelid Eyelashes Site where conjunctiva merges with cornea Palpebral fissure Lateral commissure Eyelid Medial commissure (a) Surface anatomy of the right eye Figure 15.1a Orbicularis oculi muscle -

Clinical Features and Treatment of Pediatric Orbit Fractures
ORIGINAL INVESTIGATION Clinical Features and Treatment of Pediatric Orbit Fractures Eric M. Hink, M.D.*, Leslie A. Wei, M.D.*, and Vikram D. Durairaj, M.D., F.A.C.S.*† Departments of *Ophthalmology, and †Otolaryngology and Head and Neck Surgery, University of Colorado Denver, Aurora, Colorado, U.S.A. of craniofacial skeletal development.1 Orbit fractures may be Purpose: To describe a series of orbital fractures and associated with ophthalmic, neurologic, and craniofacial inju- associated ophthalmic and craniofacial injuries in the pediatric ries that may require intervention. The result is that pediatric population. facial trauma is often managed by a diverse group of specialists, Methods: A retrospective case series of 312 pediatric and each service may have their own bias as to the ideal man- patients over a 9-year period (2002–2011) with orbit fractures agement plan.4 In addition, children’s skeletal morphology and diagnosed by CT. physiology are quite different from adults, and the benefits of Results: Five hundred ninety-one fractures in 312 patients surgery must be weighed against the possibility of detrimental were evaluated. There were 192 boys (62%) and 120 girls (38%) changes to facial skeletal growth and development. The purpose with an average age of 7.3 years (range 4 months to 16 years). of this study was to describe a series of pediatric orbital frac- Orbit fractures associated with other craniofacial fractures were tures; associated ophthalmic, neurologic, and craniofacial inju- more common (62%) than isolated orbit fractures (internal ries; and fracture management and outcomes. fractures and fractures involving the orbital rim but without extension beyond the orbit) (38%). -

Eyelid Conjunctival Tumors
EYELID &CONJUNCTIVAL TUMORS PHOTOGRAPHIC ATLAS Dr. Olivier Galatoire Dr. Christine Levy-Gabriel Dr. Mathieu Zmuda EYELID & CONJUNCTIVAL TUMORS 4 EYELID & CONJUNCTIVAL TUMORS Dear readers, All rights of translation, adaptation, or reproduction by any means are reserved in all countries. The reproduction or representation, in whole or in part and by any means, of any of the pages published in the present book without the prior written consent of the publisher, is prohibited and illegal and would constitute an infringement. Only reproductions strictly reserved for the private use of the copier and not intended for collective use, and short analyses and quotations justified by the illustrative or scientific nature of the work in which they are incorporated, are authorized (Law of March 11, 1957 art. 40 and 41 and Criminal Code art. 425). EYELID & CONJUNCTIVAL TUMORS EYELID & CONJUNCTIVAL TUMORS 5 6 EYELID & CONJUNCTIVAL TUMORS Foreword Dr. Serge Morax I am honored to introduce this Photographic Atlas of palpebral and conjunctival tumors,which is the culmination of the close collaboration between Drs. Olivier Galatoire and Mathieu Zmuda of the A. de Rothschild Ophthalmological Foundation and Dr. Christine Levy-Gabriel of the Curie Institute. The subject is now of unquestionable importance and evidently of great interest to Ophthalmologists, whether they are orbital- palpebral specialists or not. Indeed, errors or delays in the diagnosis of tumor pathologies are relatively common and the consequences can be serious in the case of malignant tumors, especially carcinomas. Swift diagnosis and anatomopathological confirmation will lead to a treatment, discussed in multidisciplinary team meetings, ranging from surgery to radiotherapy. -

Adrenaline Dacryolith: Detection by Ultrasound Examination of the Nasolacrimal Duct
Br J Ophthalmol: first published as 10.1136/bjo.72.12.935 on 1 December 1988. Downloaded from British Journal ofOphthalmology, 1988, 72, 935-937 Adrenaline dacryolith: detection by ultrasound examination of the nasolacrimal duct JOHN A BRADBURY,' IAN G RENNIE,' AND M ANDREW PARSONS2 From the Departments of'Ophthalmology and 2Pathology, University ofSheffield SUMMARY A 73-year-old woman on topical pilocarpine and adrenaline for chronic simple glaucoma for three years presented with a mass in the medial canthus of the right eye. Although dacryocystography showed a dilated and partially obstructed nasolacrimal system, ultrasound examination was able to demonstrate a mass in the nasolacrimal duct. At operation a black dacryolith was found, of the diameter predicted by ultrasound. Histological examination of the dacryolith suggested its derivation from breakdown products of adrenaline. Ultrasound examination of the nasolacrimal drain- her right conjunctival sac. In between these acute age system has been shown to be of value when the episodes the epiphora and a slight swelling at the copyright. system is dilated in cases such as a mucocoele or acute medial canthus persisted but were less troublesome. dacryocystitis. It is of limited value in functional Her right nasolacrimal duct had been irrigated during disorders, where the passage of fluid through the one of these acute episodes, which had caused some nasolacrimal system is slowed, producing a minimally resolution of her symptoms. dilated system.' No reports so far have illustrated the On examination a firm mass was palpable over the ability of ultrasound to demonstrate a mass in the right lacrimal fossa extending slightly above the nasolacrimal duct. -
Lid and Lash Conditions
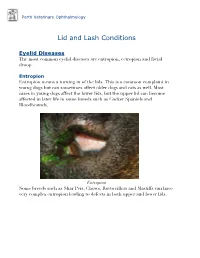
Perth Veterinary Ophthalmology Lid and Lash Conditions Eyelid Diseases The most common eyelid diseases are entropion, ectropion and facial droop. Entropion Entropion means a turning in of the lids. This is a common complaint in young dogs but can sometimes affect older dogs and cats as well. Most cases in young dogs affect the lower lids, but the upper lid can become affected in later life in some breeds such as Cocker Spaniels and Bloodhounds. Entropion Some breeds such as Shar Peis, Chows, Rottweillers and Mastiffs can have very complex entropion leading to defects in both upper and lower lids. A Shar Pei with severe upper and lower lid entropion Entropion is painful and can be potentially blinding. The rolling in of the lid leads to hair coming into contact with the cornea, leading to pain, ulceration and scarring (which can affect vision). In severe cases this can even lead to perforation of the eye. There are many causes of entropion. It can be primary or secondary to other problems affecting the lids (such as ectopic cilia, distichiasis etc. - see below). Some possible causes include the lid being too long, the lid being too tight, instability of the lateral canthus (outer cornea of the eyelids), misdirection of the lateral canthal tendon, brachycephalic anatomy (big eyes and short nose - e.g. Pekingese, Pugs, Shih Tsus, Persian cats etc.), diamond eye defects, loose or too much skin, facial droop etc. Often these cases are referred to a veterinary ophthalmologist for proper assessment and treatment to provide the best outcome. Entropion requires surgical correction. -

MBB: Head & Neck Anatomy
MBB: Head & Neck Anatomy Skull Osteology • This is a comprehensive guide of all the skull features you must know by the practical exam. • Many of these structures will be presented multiple times during upcoming labs. • This PowerPoint Handout is the resource you will use during lab when you have access to skulls. Mind, Brain & Behavior 2021 Osteology of the Skull Slide Title Slide Number Slide Title Slide Number Ethmoid Slide 3 Paranasal Sinuses Slide 19 Vomer, Nasal Bone, and Inferior Turbinate (Concha) Slide4 Paranasal Sinus Imaging Slide 20 Lacrimal and Palatine Bones Slide 5 Paranasal Sinus Imaging (Sagittal Section) Slide 21 Zygomatic Bone Slide 6 Skull Sutures Slide 22 Frontal Bone Slide 7 Foramen RevieW Slide 23 Mandible Slide 8 Skull Subdivisions Slide 24 Maxilla Slide 9 Sphenoid Bone Slide 10 Skull Subdivisions: Viscerocranium Slide 25 Temporal Bone Slide 11 Skull Subdivisions: Neurocranium Slide 26 Temporal Bone (Continued) Slide 12 Cranial Base: Cranial Fossae Slide 27 Temporal Bone (Middle Ear Cavity and Facial Canal) Slide 13 Skull Development: Intramembranous vs Endochondral Slide 28 Occipital Bone Slide 14 Ossification Structures/Spaces Formed by More Than One Bone Slide 15 Intramembranous Ossification: Fontanelles Slide 29 Structures/Apertures Formed by More Than One Bone Slide 16 Intramembranous Ossification: Craniosynostosis Slide 30 Nasal Septum Slide 17 Endochondral Ossification Slide 31 Infratemporal Fossa & Pterygopalatine Fossa Slide 18 Achondroplasia and Skull Growth Slide 32 Ethmoid • Cribriform plate/foramina -

The Management of Congenital Malpositions of Eyelids, Eyes and Orbits
Eye (\988) 2, 207-219 The Management of Congenital Malpositions of Eyelids, Eyes and Orbits S. MORAX AND T. HURBLl Paris Summary Congenital malformations of the eye and its adnexa which are multiple and varied can affect the whole eyeball or any part of it, as well as the orbit, eyelids, lacrimal ducts, extra-ocular muscles and conjunctiva. A classification of these malformations is presented together with the general principles of treatment, age of operating and surgical tactics. The authors give some examples of the anatomo-clinical forms, eyelid malpositions such as entropion, ectropion, ptosis, levator eyelid retraction, medial canthus malposition, congenital eyelid colobomas, and congenital orbital abnormalities (Craniofacial stenosis, orbi tal plagiocephalies, hypertelorism, anophthalmos, microphthalmos and cryptophthalmos) . Congenital malformations of the eye and its as echography, CT-scan and NMR, enzymatic adnexa are multiple and varied. They can work-up or genetic studies (Table I). affect the whole eyeball or any part of it, as Surgical treatment when feasible will well as the orbit, eyelids, lacrimal ducts extra encounter numerous problems; age will play a ocular muscles and conjunctiva. role, choice of a surgical protocol directly From the anatomical point of view, the fol related to the existing complaints, and coop lowing can be considered. eration between several surgical teams Position abnormalities (malpositions) of (ophthalmologic, plastic, cranio-maxillo-fac one or more elements and formation abnor ial and neurosurgical), the ideal being to treat malities (malformations) of the same organs. Some of these abnormalities are limited to Table I The manag ement of cong enital rna/positions one organ and can be subjected to a relatively of eyelid s, eyes and orbits simple and well recognised surgical treat Ocular Findings: ment. -

Splanchnocranium
splanchnocranium - Consists of part of skull that is derived from branchial arches - The facial bones are the bones of the anterior and lower human skull Bones Ethmoid bone Inferior nasal concha Lacrimal bone Maxilla Nasal bone Palatine bone Vomer Zygomatic bone Mandible Ethmoid bone The ethmoid is a single bone, which makes a significant contribution to the middle third of the face. It is located between the lateral wall of the nose and the medial wall of the orbit and forms parts of the nasal septum, roof and lateral wall of the nose, and a considerable part of the medial wall of the orbital cavity. In addition, the ethmoid makes a small contribution to the floor of the anterior cranial fossa. The ethmoid bone can be divided into four parts, the perpendicular plate, the cribriform plate and two ethmoidal labyrinths. Important landmarks include: • Perpendicular plate • Cribriform plate • Crista galli. • Ala. • Ethmoid labyrinths • Medial (nasal) surface. • Orbital plate. • Superior nasal concha. • Middle nasal concha. • Anterior ethmoidal air cells. • Middle ethmoidal air cells. • Posterior ethmoidal air cells. Attachments The falx cerebri (slide) attaches to the posterior border of the crista galli. lamina cribrosa 1 crista galli 2 lamina perpendicularis 3 labyrinthi ethmoidales 4 cellulae ethmoidales anteriores et posteriores 5 lamina orbitalis 6 concha nasalis media 7 processus uncinatus 8 Inferior nasal concha Each inferior nasal concha consists of a curved plate of bone attached to the lateral wall of the nasal cavity. Each consists of inferior and superior borders, medial and lateral surfaces, and anterior and posterior ends. The superior border serves to attach the bone to the lateral wall of the nose, articulating with four different bones.