SUTTER HEALTH PLUS FORMULARY Drug List for HMO Members – Effective September 1, 2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antibiotic Treatment in Inflammatory Bowel Disease: Rifaximin, a New Possible Approach
European Review for Medical and Pharmacological Sciences 1999; 3: 27-30 Review – Antibiotic treatment in inflammatory bowel disease: rifaximin, a new possible approach P. GIONCHETTI, F. RIZZELLO, A. VENTURI, F. UGOLINI*, M. ROSSI**, P. BRIGIDI**, R. JOHANSSON, A. FERRIERI***, G. POGGIOLI*, M. CAMPIERI Clinica Medica I, Nuove Patologie, Bologna University (Italy) *Istituto di Clinica Chirurgica II, Bologna University (Italy) **Dipartimento di Scienze Farmaceutiche, Bologna University (Italy) ***Direzione Medica Alfa Wassermann, Bologna (Italy) Abstract. – The etiology of inflammatory ported the presence of a breakdown of toler- disease is still unknown, but a body of evidence ance to the normal commensal intestinal flora from clinical and experimental observation indi- in active IBD2-3. Reduction of microflora by cates a role for intestinal microflora in the pathogenesis of this disease. Reduction of mi- antibiotics, bowel rest and fecal diversion de- croflora using antibiotics, bowel rest and fecal creases inflammatory activity in Crohn’s dis- diversion decreases activity in Crohn’s disease ease and to a lesser extent in ulcerative colitis and in ulcerative colitis. Several trials have been (UC). The pathogenetic role of intestinal mi- carried out on the use of antibiotic treatment in croflora is further suggested by the observa- patients with active ulcerative colitis with con- tion that experimental colitis, in germ-free or trasting results. A number of trials have been antibiotic treated animals, is less severe com- carried out using Rifaximin, a non-absorbable broad-spectrum antibiotic, confirming the ab- pared to that inducible in normal animals or sence of systemic bioavalaibility of the drug at times is not inducible at all. -

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

Lifestyle Drugs” for Men and Women
Development of “Lifestyle Drugs” for Men and Women Armin Schultz CRS - Clinical Research Services Mannheim GmbH AGAH Annual Meeting 2012, Leipzig, March 01 - 02 Lifestyle drugs Smart drugs, Quality-of-life drugs, Vanity drugs etc. Lifestyle? Lifestyle-Drugs? Active development? Discovery by chance? AGAH Annual Meeting 2012, Leipzig, March 01 - 02 Lifestyle A lifestyle is a characteristic bundle of behaviors that makes sense to both others and oneself in a given time and place, including social relations, consumption, entertainment, and dress. The behaviors and practices within lifestyles are a mixture of habits, conventional ways of doing things, and reasoned actions „Ein Lebensstil ist [...] der regelmäßig wiederkehrende Gesamtzusammenhang der Verhaltensweisen, Interaktionen, Meinungen, Wissensbestände und bewertenden Einstellungen eines Menschen“ (Hradil 2005: 46) Different definitions in social sciences, philosophy, psychology or medicine AGAH Annual Meeting 2012, Leipzig, March 01 - 02 Lifestyle Many “subdivisions” LOHAS: “Lifestyles of Health and Sustainability“ LOVOS: “Lifestyles of Voluntary Simplicity“ SLOHAS: “Slow Lifestyles of Happiness and Sustainability” PARKOS: “Partizipative Konsumenten“ ……. ……. ……. AGAH Annual Meeting 2012, Leipzig, March 01 - 02 Lifestyle drugs Lifestyle drug is an imprecise term commonly applied to medications which treat non-life threatening and non-painful conditions such as baldness, impotence, wrinkles, or acne, without any medical relevance at all or only minor medical relevance relative to others. Desire for increase of personal well-being and quality of life It is sometimes intended as a pejorative, bearing the implication that the scarce medical research resources allocated to develop such drugs were spent frivolously when they could have been better spent researching cures for more serious medical conditions. -

FDA Warns About an Increased Risk of Serious Pancreatitis with Irritable Bowel Drug Viberzi (Eluxadoline) in Patients Without a Gallbladder
FDA warns about an increased risk of serious pancreatitis with irritable bowel drug Viberzi (eluxadoline) in patients without a gallbladder Safety Announcement [03-15-2017] The U.S. Food and Drug Administration (FDA) is warning that Viberzi (eluxadoline), a medicine used to treat irritable bowel syndrome with diarrhea (IBS-D), should not be used in patients who do not have a gallbladder. An FDA review found these patients have an increased risk of developing serious pancreatitis that could result in hospitalization or death. Pancreatitis may be caused by spasm of a certain digestive system muscle in the small intestine. As a result, we are working with the Viberzi manufacturer, Allergan, to address these safety concerns. Patients should talk to your health care professional about how to control your symptoms of irritable bowel syndrome with diarrhea (IBS-D), particularly if you do not have a gallbladder. The gallbladder is an organ that stores bile, one of the body’s digestive juices that helps in the digestion of fat. Stop taking Viberzi right away and get emergency medical care if you develop new or worsening stomach-area or abdomen pain, or pain in the upper right side of your stomach-area or abdomen that may move to your back or shoulder. This pain may occur with nausea and vomiting. These may be symptoms of pancreatitis, an inflammation of the pancreas, an organ important in digestion; or spasm of the sphincter of Oddi, a muscular valve in the small intestine that controls the flow of digestive juices to the gut. Health care professionals should not prescribe Viberzi in patients who do not have a gallbladder and should consider alternative treatment options in these patients. -
Prevention and Management of Intravesical BCG-Related Lower Urinary Tract Symptoms with Prophylactic Pentosan Polysulphate In
Prevention and Management of Intravesical BCG-related Lower Urinary Tract Symptoms with Prophylactic Pentosan Polysulphate in Patients with Non-Muscle-Invasive Bladder Cancer: A Randomized Controlled Trial Samer Shamout, Simon Tanguay, Maurice Anidjar, Lysanne Campeau CQI Research Grant 2017 INTRODUCTION METHODS / INTERVENTIONS PATIENT IMPACT Study Design • Bacillus Calmette-Guerin (BCG) remains the most effective • Phase 2, double-blind, randomized, placebo-controlled, parallel-group • Improve patient experience by identifying predictor markers prophylactic treatment of intermediate and high-risk non- study rendering patients at higher risk of developing BCG-related muscle invasive bladder cancer. • Multicentre trial involving two partner sites: (Jewish General Hospital, LUTS. McGill University Health Centre) • 30 to 60% of bladder cancer patients experienced systemic • This will guide patient counselling before treatment to inform Outcomes them about associated risks and benefits of the BCG and local adverse events of variable severity following Primary outcomes (change from baseline to end of treatment): treatment. intravesical BCG therapy • Mean change in number of urgency episodes/24hr (3-day bladder diary) • Only 16 to 29% of patients completed all the three-year BCG • Mean change in ICIQ-LUTSqol score • We will determine the role of prophylactic PPS to prevent these treatment regimen. • Mean change in OAB-V8 score LUTS from occurring, particularly if patients are considered at Secondary outcomes (change from baseline to end of treatment): higher risk, and therefore improve patient experience. • Guidelines recommend medications, such as oxybutynin • Mean change in VAS score only phenazopyridine, and propantheline bromide for short term • Mean change in urinary inflammatory markers (TRAIL, IFN, IL-2, IL-10) • The improvement measurements are validated in the symptomatic relief. -

Ophthalmic Adverse Effects of Nasal Decongestants on an Experimental
A RQUIVOS B RASILEIROS DE ORIGINAL ARTICLE Ophthalmic adverse effects of nasal decongestants on an experimental rat model Efeitos oftálmicos adversos de descongestionantes nasais em modelo experimental com ratos Ayse Ipek Akyuz Unsal1, Yesim Basal2, Serap Birincioglu3, Tolga Kocaturk1, Harun Cakmak1, Alparslan Unsal4, Gizem Cakiroz5, Nüket Eliyatkın6, Ozden Yukselen7, Buket Demirci5 1. Department of Ophthalmology, Medical Faculty, Adnan Menderes University, Aydin, Turkey. 2. Department of Otorhinolaringology, Medical Faculty, Adnan Menderes University, Aydin, Turkey. 3. Department of Pathology, Veterinary Faculty, Adnan Menderes University, Aydin, Turkey. 4. Department of Radiology, Medical Faculty, Adnan Menderes University, Aydin, Turkey. 5. Department of Medical Pharmacology, Medical Faculty, Adnan Menderes University, Aydin, Turkey. 6. Department of Medical Pathology, Medical Faculty, Adnan Menderes University, Aydin, Turkey. 7. Department of Pathology, Aydin State Hospital, Aydin, Turkey. ABSTRACT | Purpose: To investigate the potential effects of cause ophthalmic problems such as dry eyes, corneal edema, chronic exposure to a nasal decongestant and its excipients cataracts, retinal nerve fiber layer, and vascular damage in on ocular tissues using an experimental rat model. Methods: rats. Although these results were obtained from experimental Sixty adult male Wistar rats were randomized into six groups. animals, ophthalmologists should keep in mind the potential The first two groups were control (serum physiologic) and ophthalmic adverse effects of this medicine and/or its excipients Otrivine® groups. The remaining four groups received the and exercise caution with drugs containing xylometazoline, Otrivine excipients xylometazoline, benzalkonium chloride, ethylene diamine tetra acetic acid, benzalkonium chloride and sorbitol, and ethylene diamine tetra acetic acid. Medications sorbitol for patients with underlying ocular problems. -
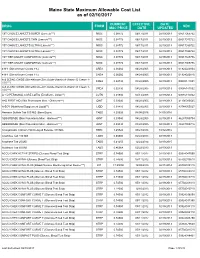
Maine State Maximum Allowable Cost List As of 02/10/2017
Maine State Maximum Allowable Cost List as of 02/10/2017 CURRENT EFFECTIVE DATE DRUG FORM NDC MAC PRICE DATE UPDATED 1ST CHOICE LANCETS SUPER (Lancets***) MISC 0.08772 06/17/2011 02/19/2013 08517065722 1ST CHOICE LANCETS THIN (Lancets***) MISC 0.08772 06/17/2011 02/19/2013 08517015722 1ST CHOICE LANCETS ULTRA (Lancets***) MISC 0.08772 06/17/2011 02/19/2013 08517030722 1ST CHOICE LANCETS ULTRA (Lancets***) MISC 0.08772 06/17/2011 02/19/2013 08517035722 1ST TIER UNILET COMFORTOU (Lancets***) MISC 0.08772 06/17/2011 02/19/2013 08517025736 1ST TIER UNILET COMFORTOU (Lancets***) MISC 0.08772 06/17/2011 02/19/2013 08517065736 4-N-1 (Dimethicone Cream 1%) CREA 0.06060 04/28/2005 02/19/2013 61924020804 4-N-1 (Dimethicone Cream 1%) CREA 0.06060 04/28/2005 02/19/2013 61924020816 A & D ZINC OXIDE (Dimethicone-Zinc Oxide-Vitamin A-Vitamin D Cream 1- CREA 0.02730 04/28/2005 02/19/2013 00085141001 10%***) A & D ZINC OXIDE (Dimethicone-Zinc Oxide-Vitamin A-Vitamin D Cream 1- CREA 0.02730 04/28/2005 02/19/2013 00085141002 10%***) A + D PERSONAL CARE LOTIO (Emollient - Lotion**) LOTN 0.01940 03/13/2008 02/19/2013 00085113002 A+D FIRST AID (Skin Protectants Misc - Ointment***) OINT 0.03040 04/28/2005 02/19/2013 41100080545 A-SOY (Nutritional Supplement Liquid**) LIQD 0.01410 04/28/2005 02/19/2013 83744055027 Abacavir Sulfate Tab 300 MG (Base Equiv) TABS 4.20626 04/08/2016 04/05/2016 ABSORBASE (Skin Protectants Misc - Ointment***) OINT 0.03040 04/28/2005 02/19/2013 46287050704 ABSORBASE (Skin Protectants Misc - Ointment***) OINT 0.03040 04/28/2005 02/19/2013 -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Pharmacokinetics, Pharmacodynamics and Drug
pharmaceutics Review Pharmacokinetics, Pharmacodynamics and Drug–Drug Interactions of New Anti-Migraine Drugs—Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Department of Clinical Pharmacy and Biopharmacy, Pozna´nUniversity of Medical Sciences, Sw.´ Marii Magdaleny 14 St., 61-861 Pozna´n,Poland; [email protected] Received: 28 October 2020; Accepted: 30 November 2020; Published: 3 December 2020 Abstract: In the last few years, there have been significant advances in migraine management and prevention. Lasmiditan, ubrogepant, rimegepant and monoclonal antibodies (erenumab, fremanezumab, galcanezumab, and eptinezumab) are new drugs that were launched on the US pharmaceutical market; some of them also in Europe. This publication reviews the available worldwide references on the safety of these anti-migraine drugs with a focus on the possible drug–drug (DDI) or drug–food interactions. As is known, bioavailability of a drug and, hence, its pharmacological efficacy depend on its pharmacokinetics and pharmacodynamics, which may be altered by drug interactions. This paper discusses the interactions of gepants and lasmiditan with, i.a., serotonergic drugs, CYP3A4 inhibitors, and inducers or breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitors. In the case of monoclonal antibodies, the issue of pharmacodynamic interactions related to the modulation of the immune system functions was addressed. It also focuses on the effect of monoclonal antibodies on expression of class Fc gamma receptors (FcγR). Keywords: migraine; lasmiditan; gepants; monoclonal antibodies; drug–drug interactions 1. Introduction Migraine is a chronic neurological disorder characterized by a repetitive, usually unilateral, pulsating headache with attacks typically lasting from 4 to 72 h. -

Impact of Tamsulosin, Tolterodine and Drug-Combination On
African Journal of Urology (2017) 23, 28–32 African Journal of Urology Official journal of the Pan African Urological Surgeon’s Association web page of the journal www.ees.elsevier.com/afju www.sciencedirect.com Original article Impact of Tamsulosin, Tolterodine and drug-combination on the outcomes of lower urinary tract symptoms secondary to post-ureteroscopy ureteral stent: A prospective randomized controlled clinical study a b,∗ a a O. Abdelkader , K. Mohyelden , M.H. Sherif , A.H. Metwaly , b c d a H. Aldaqadossi , A. Shelbaya , H. Khairy , A. Elnashar a Department of Urology, Suez Canal University, Ismailia, Egypt b Department of Urology, Fayoum University, Fayoum, Egypt c Student Hospital, Cairo University, Cairo, Egypt d Department of Urology, Cairo University, Cairo, Egypt Received 17 March 2016; received in revised form 23 June 2016; accepted 23 June 2016 Available online 18 November 2016 KEYWORDS Abstract Anticholinergics; Objectives: To compare the role of alpha-blocker (Tamsulosin) monotherapy, anticholinergic (Tolterodine) ␣-Adrenergic blockers; monotherapy or combination of both drugs versus analgesics in improving post-ureteroscopy (URS) lower Ureter stent; urinary tract symptoms related to double-J ureteral stent. Ureteroscopy Patients and methods: Between January 2009 and June 2013, 160 consecutive patients with ureteric stones were included in this study at 2 tertiary care centers’. Patients were randomized into 4 groups; group A (n = 40) received 0.4 mg Tamsulosin once a day, group B (n = 40) received 4 mg Tolterodine once a day, group C (n = 40) received Tamsulosin 0.4 mg and Tolterodine 4 mg once a day and group D (n = 40) as a control group, received placebo once a day. -

“The Silver Sheet” MEDICAL DEVICE QUALITY CONTROL
F-D-C REPORTS — FOUNDED 1939 $665 A YEAR ® www.TheSilverSheet.com“The Silver Sheet” MEDICAL DEVICE QUALITY CONTROL Vol. 13, No. 2 February 2009 THE NEWS THIS ISSUE • RECALLS SOARED TO THEIR HIGHEST POINT EVER IN 2008, with companies recalling a total of 845 devices. Many of the recalls were related to software problems and tainted heparin. “The goal is to try and decrease those recalls,” says Tim Ulatowski, director of CDRH’s Office of Compliance. “So we’re trying to push that number down through effective enforcement actions and industry training.” There is good news, however: The number of Class I recalls fell from 23 in 2007 to only 17 in 2008 – industry’s best Class I showing since 2003. Also, the recall manager for a Virginia hospital chain tells what companies should do to make their recall letters clearer and easier to comply with. “We get some recall letters and we truly don’t know what to do with them,” Bea Haupt says................................................Below • COMPLETE TABLE OF RECALLS FROM 2008 includes 17 Class I (2%), 726 Class II (86%) and 107 Class III (12%) medical device events ............................................................................................................12 • WARNING LETTERS: I-Flow cited for QS and MDR reg violations in relation to its infusion pumps.........66 • IN BRIEF: New GHTF guidance instructs firms on the control of products and services obtained from suppliers; former OSEL Director Larry Kessler is concerned that CDRH doesn’t always follow scientific principles and practices .......................................................................................................Back page Problems Related To Software, Heparin Help Push Recalls To All-Time High Also, FDA And Industry Experts Give Tips For Composing Recall Letters The number of recalled medical devices counting methods are typically negligible; the skyrocketed last year to its highest point ever, agency counted 831 total recalls in FY 2008 and spurred on by a large volume of Class II recalls 664 in FY 2007.