The Burden of Serious Fungal Infections in Cameroon
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Congo DRC, Kamwiziku. Mycoses 2021
Received: 8 April 2021 | Revised: 1 June 2021 | Accepted: 10 June 2021 DOI: 10.1111/myc.13339 REVIEW ARTICLE Serious fungal diseases in Democratic Republic of Congo – Incidence and prevalence estimates Guyguy K. Kamwiziku1 | Jean- Claude C. Makangara1 | Emma Orefuwa2 | David W. Denning2,3 1Department of Microbiology, Kinshasa University Hospital, University of Abstract Kinshasa, Kinshasa, Democratic Republic A literature review was conducted to assess the burden of serious fungal infections of Congo 2Global Action Fund for Fungal Infections, in the Democratic Republic of the Congo (DRC) (population 95,326,000). English and Geneva, Switzerland French publications were listed and analysed using PubMed/Medline, Google Scholar 3 Manchester Fungal Infection Group, The and the African Journals database. Publication dates spanning 1943– 2020 were in- University of Manchester, Manchester Academic Health Science Centre, cluded in the scope of the review. From the analysis of published articles, we estimate Manchester, UK a total of about 5,177,000 people (5.4%) suffer from serious fungal infections in the Correspondence DRC annually. The incidence of cryptococcal meningitis, Pneumocystis jirovecii pneu- Guyguy K. Kamwiziku, Department monia in adults and invasive aspergillosis in AIDS patients was estimated at 6168, of Microbiology, Kinshasa University Hospital, University of Kinshasa, Congo. 2800 and 380 cases per year. Oral and oesophageal candidiasis represent 50,470 Email: [email protected] and 28,800 HIV- infected patients respectively. Chronic pulmonary aspergillosis post- tuberculosis incidence and prevalence was estimated to be 54,700. Fungal asthma (allergic bronchopulmonary aspergillosis and severe asthma with fungal sensitiza- tion) probably has a prevalence of 88,800 and 117,200. -

Pediatric Invasive Gastrointestinal Fungal Infections: Causative Agents and Diagnostic Modalities
Microbiology Research Journal International 19(2): 1-11, 2017; Article no.MRJI.32231 Previously known as British Microbiology Research Journal ISSN: 2231-0886, NLM ID: 101608140 SCIENCEDOMAIN international www.sciencedomain.org Pediatric Invasive Gastrointestinal Fungal Infections: Causative Agents and Diagnostic Modalities Mortada H. F. El-Shabrawi 1, Lamiaa A. Madkour 2* , Naglaa Kamal 1 and Kerstin Voigt 3 1Department of Pediatrics, Faculty of Medicine, Cairo University, Egypt. 2Department of Microbiology and Immunology, Faculty of Medicine, Cairo University, Egypt. 3Department of Microbiology and Molecular Biology, University of Jena, Germany. Authors’ contributions This work was carried out in collaboration between all authors. Author MHFES specified the topic of the research. Author LAM designed the study, managed the literature research and wrote the first draft of the manuscript. Authors NK and KV wrote the subsequent drafts. Author MHFES revised the manuscript. All authors read and approved the final manuscript. Article Information DOI: 10.9734/MRJI/2017/32231 Editor(s): (1) Raúl Rodríguez-Herrera, Autonomous University of Coahuila, México. Reviewers: (1) Hasibe Vural, Necmettin Erbakan Üniversity, Turkey. (2) Berdicevsky Israela, Technion Faculty of Medicine, Haifa, Israel. (3) Vassiliki Pitiriga, University of Athens, Greece. Complete Peer review History: http://www.sciencedomain.org/review-history/18327 Received 16 th February 2017 th Review Article Accepted 18 March 2017 Published 24 th March 2017 ABSTRACT Invasive gastrointestinal fungal infections are posing a serious threat to the ever-expanding population of immunocompromised children, as well as some healthy children at risk. In this narrative review, we collate and explore the etiologies and diagnostic modalities of these overlooked infections. -

Pulmonary Basidiobolomycosis: an Unusual Presentation in a Cancer Patient: a Case Report and Mini Review of Cases in India
Int.J.Curr.Microbiol.App.Sci (2015) 4(5): 798-805 ISSN: 2319-7706 Volume 4 Number 5 (2015) pp. 798-805 http://www.ijcmas.com Case Study Pulmonary Basidiobolomycosis: An unusual presentation in a cancer patient: A case report and mini review of cases in India Deba Dulal Biswal1, Manisa Sahu2* and Pallavi Bhaleker3 1Department of Medical Oncology, S L Raheja Hospital (A Fortis Associate) Mahim (W), Mumbai-400016, India 2Department of Microbiology, S L Raheja Hospital (A Fortis Associate) Mahim(W), Mumbai-400016, India *Corresponding author A B S T R A C T K e y w o r d s Basidiobolomycosis is an uncommon disease caused by Basidiobolus Basidiobolo- ranarum. The clinical presentation varies from localized subcutaneous mycosis, infection to widespread dissemination involving different viscera s, notably Basidio-bolus the gastrointestinal tract. Pulmonary involvement is rarer; we report a case ranarum, of pulmonary Basidiobolomycosis in a lung cancer patient. lung cancer Introduction Basidiobolo mycosis is caused by the fungus cases are from Southern part.( Sujatha S et Basidiobolus ranarum, which is a al., 2003; Chandrasekhar HR et al., 1998; zygomycetes belonging to order Prasad PV et al., 2002; Krishnan et al., Entomophthorales. (Gugnani, H. C et al., 1998) Rare dissemination with visceral 1999) This filamentous fungus is usually involvement by Basidiobolus are quoted by associated with subcutaneous zygomycosis various authors such as gastrointestinal tract, of trunk and limbs in immune competent uterus, urinary bladder and retro peritoneum. individuals (Ribes JA et al., 2000) It is an (Bigliazzi C et al., 2004; Khan ZU et al., environmental saprophyte isolated mostly 2001; Nazir Z et al., 1997; Choonhakarn C from decaying vegetation, foodstuffs, fruits, et al., 2004) Pulmonary involvement are and soil. -

A Case of Disseminated Histoplasmosis Detected in Peripheral Blood Smear Staining Revealing AIDS at Terminal Phase in a Female Patient from Cameroon
Hindawi Publishing Corporation Case Reports in Medicine Volume 2012, Article ID 215207, 3 pages doi:10.1155/2012/215207 Case Report A Case of Disseminated Histoplasmosis Detected in Peripheral Blood Smear Staining Revealing AIDS at Terminal Phase in a Female Patient from Cameroon Christine Mandengue Ebenye Cliniques Universitaires des Montagnes, Bangangt´e, Cameroon Correspondence should be addressed to Christine Mandengue Ebenye, [email protected] Received 28 August 2012; Revised 2 November 2012; Accepted 5 November 2012 Academic Editor: Ingo W. Husstedt Copyright © 2012 Christine Mandengue Ebenye. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Histoplasmosis is endemic in the American continent and also in Sub-Saharan Africa, coexisting with the African histoplasmosis. Immunosuppressed patients, especially those with advanced HIV infection develop a severe disseminated histoplasmosis with fatal prognosis. The definitive diagnosis of disseminated histoplasmosis is based on the detection of Histoplasma capsulatum from patient’ tissues samples or body fluids. Among the diagnostic tests peripheral blood smear staining is not commonly used. Nonetheless a few publications reveal that Histoplasma capsulatum has been discovered by chance using this method in HIV infected patients with chronic fever and hence revealed AIDS at the terminal phase. We report a new case detected in a Cameroonian woman without any previous history of HIV infection. Peripheral blood smear staining should be commonly used for the diagnosis of disseminated histoplasmosis in the Sub-Saharan Africa, where facilities for mycology laboratories are unavailable. 1. Introduction 1987 [2]. -

Opportunistic Invasive Fungal Infections: Diagnosis & Clinical
Review Article Indian J Med Res 139, February 2014, pp 195-204 Opportunistic invasive fungal infections: diagnosis & clinical management Parisa Badiee & Zahra Hashemizadeh Prof. Alborzi Clinical Microbiology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran Received May 14, 2013 Invasive fungal infections are a significant health problem in immunocompromised patients. The clinical manifestations vary and can range from colonization in allergic bronchopulmonary disease to active infection in local aetiologic agents. Many factors influence the virulence and pathogenic capacity of the microorganisms, such as enzymes including extracellular phospholipases, lipases and proteinases, dimorphic growth in some Candida species, melanin production, mannitol secretion, superoxide dismutase, rapid growth and affinity to the blood stream, heat tolerance and toxin production. Infection is confirmed when histopathologic examinationwith special stains demonstrates fungal tissue involvement or when the aetiologic agent is isolated from sterile clinical specimens by culture. Both acquired and congenital immunodeficiency may be associated with increased susceptibility to systemic infections. Fungal infection is difficult to treat because antifungal therapy forCandida infections is still controversial and based on clinical grounds, and for molds, the clinician must assume that the species isolated from the culture medium is the pathogen. Timely initiation of antifungal treatment is a critical component affecting the outcome. Disseminated infection requires the use of systemic agents with or without surgical debridement, and in some cases immunotherapy is also advisable. Preclinical and clinical studies have shown an association between drug dose and treatment outcome. Drug dose monitoring is necessary to ensure that therapeutic levels are achieved for optimal clinical efficacy. The objectives of this review are to discuss opportunistic fungal infections, diagnostic methods and the management of these infections. -

Diagnostic Methods for Detection and Characterisation of Dimorphic Fungi Causing Invasive Disease in Africa: Development and Evaluation
Diagnostic methods for detection and characterisation of dimorphic fungi causing invasive disease in Africa: Development and evaluation TSIDISO GUGU MAPHANGA Diagnostic methods for detection and characterisation of dimorphic fungi causing invasive disease in Africa: Development and evaluation by TSIDISO GUGU MAPHANGA A thesis submitted in partial fulfilment of the requirements for the degree of PHILOSOPHIAE DOCTOR PhD (Medical Microbiology) in Department of Medical Microbiology Faculty of Health Sciences University of the Free State Bloemfontein, South Africa Promoter: A/Prof NP Govender March 2020 DECLARATION I, Tsidiso Gugu Maphanga, declare that the research thesis hereby submitted to the University of the Free State for the Doctoral Degree in Medical Microbiology and the work contained therein is my own original work and has not previously, in its entirety or in part, been submitted to any institution of higher education for degree purposes. I further declare that all sources cited are acknowledged by means of a list of references. Signed this day of 2020 Research is to see what everybody else has seen and to think what nobody else has thought Albert Szent-Györgi (US Biochemist) DEDICATION To my late brother, my mechanical engineer (Thabiso Benson Masilela): I will never forget all the plans we had, the motivations, love and laughter we shared. Life is never the same without you; I miss you daily. ACKNOWLEDGMENTS To God of Abraham, Isaac, Jacob, St Engenas and my God: Thank you for giving me strength, knowledge, wisdom and the ability to undertake this project. Your faithfulness reaches to the skies. A/Professor Nelesh P. Govender (supervisor): I would like to express my sincere gratitude for your patience, guidance, continuous support and useful comments received throughout this project. -
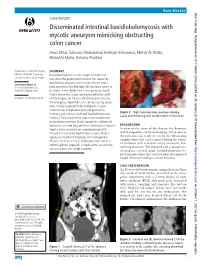
Disseminated Intestinal Basidiobolomycosis with Mycotic
Rare disease BMJ Case Rep: first published as 10.1136/bcr-2018-225054 on 29 January 2019. Downloaded from CASE REPORT Disseminated intestinal basidiobolomycosis with mycotic aneurysm mimicking obstructing colon cancer Arwa Omar Takrouni, Mohammad Heitham Schammut, Mishal Al-Otaibi, Manal Al-Mulla, Antonio Privitera Department of General Surgery, SUMMARY Ministry of Health, Dammam, Basidiobolomycosis is a rare fungal infection that Eastern Province, Saudi Arabia may affect the gastrointestinal tract. It is caused by Basidiobolus ranarum and less than 80 cases have Correspondence to Dr Arwa Omar Takrouni, been reported in the literature. The incidence seems to dr. arwa207@ gmail. com be higher in the Middle East and in particular Saudi Arabia where most cases are diagnosed in the south- Accepted 10 December 2018 western region. An 18-year-old woman presented to the emergency department with an obstructing caecal mass initially suspected to be malignant. Surgical resection was complicated by bowel perforation, Figure 2 Right hemicolectomy specimen showing histology and cultures confirmed basidiobolomycosis caecal wall thickening with necrotic debris in the lumen. infection. The postoperative course was complicated by an enterocutaneous fistula, fungal intra-abdominal abscesses, liver and lung abscesses, formation of mycotic BACKGROUND hepatic artery aneurysm and meningoencephalitis. In view of the rarity of the disease, the diagnosis The patient eventually expired due to sepsis despite and management can be challenging. The nature of aggressive treatment. Diagnosis and management the infection can result in several life-threatening complications that can be missed during the course of such rare cases are very challenging and require a of treatment such as hepatic artery aneurysm, liver multidisciplinary approach. -

Detection of Histoplasma DNA from Tissue Blocks by a Specific
Journal of Fungi Article Detection of Histoplasma DNA from Tissue Blocks by a Specific and a Broad-Range Real-Time PCR: Tools to Elucidate the Epidemiology of Histoplasmosis Dunja Wilmes 1,*, Ilka McCormick-Smith 1, Charlotte Lempp 2 , Ursula Mayer 2 , Arik Bernard Schulze 3 , Dirk Theegarten 4, Sylvia Hartmann 5 and Volker Rickerts 1 1 Reference Laboratory for Cryptococcosis and Uncommon Invasive Fungal Infections, Division for Mycotic and Parasitic Agents and Mycobacteria, Robert Koch Institute, 13353 Berlin, Germany; [email protected] (I.M.-S.); [email protected] (V.R.) 2 Vet Med Labor GmbH, Division of IDEXX Laboratories, 71636 Ludwigsburg, Germany; [email protected] (C.L.); [email protected] (U.M.) 3 Department of Medicine A, Hematology, Oncology and Pulmonary Medicine, University Hospital Muenster, 48149 Muenster, Germany; [email protected] 4 Institute of Pathology, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany; [email protected] 5 Senckenberg Institute for Pathology, Johann Wolfgang Goethe University Frankfurt, 60323 Frankfurt am Main, Germany; [email protected] * Correspondence: [email protected]; Tel.: +49-30-187-542-862 Received: 10 November 2020; Accepted: 25 November 2020; Published: 27 November 2020 Abstract: Lack of sensitive diagnostic tests impairs the understanding of the epidemiology of histoplasmosis, a disease whose burden is estimated to be largely underrated. Broad-range PCRs have been applied to identify fungal agents from pathology blocks, but sensitivity is variable. In this study, we compared the results of a specific Histoplasma qPCR (H. qPCR) with the results of a broad-range qPCR (28S qPCR) on formalin-fixed, paraffin-embedded (FFPE) tissue specimens from patients with proven fungal infections (n = 67), histologically suggestive of histoplasmosis (n = 36) and other mycoses (n = 31). -

Gastrointestinal Basidiobolomycosis, a Rare and Under-Diagnosed Fungal Infection in Immunocompetent Hosts: a Review Article
IJMS Vol 40, No 2, March 2015 Review Article Gastrointestinal Basidiobolomycosis, a Rare and Under-diagnosed Fungal Infection in Immunocompetent Hosts: A Review Article Bita Geramizadeh1,2, MD; Mina Abstract 2 2 Heidari , MD; Golsa Shekarkhar , MD Gastrointestinal Basidiobolomycosis (GIB) is an unusual, rare, but emerging fungal infection in the stomach, small intestine, colon, and liver. It has been rarely reported in the English literature and most of the reported cases have been from US, Saudi Arabia, Kuwait, and Iran. In the last five years, 17 cases have been reported from one or two provinces in Iran, and it seems that it has been undiagnosed or probably unnoticed in other parts of the country. This article has Continuous In this review, we explored the English literature from 1964 Medical Education (CME) through 2013 via PubMed, Google, and Google scholar using the credit for Iranian physicians following search keywords: and paramedics. They may 1) Basidiobolomycosis earn CME credit by reading 2) Basidiobolus ranarum this article and answering the 3) Gastrointestinal Basidiobolomycosis questions on page 190. In this review, we attempted to collect all clinical, pathological, and radiological findings of the presenting patients; complemented with previous experiences regarding the treatment and prognosis of the GIB. Since 1964, only 71 cases have been reported, which will be fully described in terms of clinical presentations, methods of diagnosis and treatment as well as prognosis and follow up. Please cite this article as: Geramizadeh B, Heidari M, Shekarkhar G. Gastrointestinal Basidiobolomycosis, a Rare and Under-diagnosed Fungal Infection in Immunocompetent Hosts: A Review Article. Iran J Med Sci. -

Isolated Hepatic Basidiobolomycosis in a 2-Year-Old
Hepat Mon. 2015 August; 15(8): e30117. DOI: 10.5812/hepatmon.30117 Case Report Published online 2015 August 29. Isolated Hepatic Basidiobolomycosis in a 2-Year-Old Girl: The First Case Report 1,* 2 2 3 Bita Geramizadeh ; Anahita Sanai Dashti ; Mohammad Rahim Kadivar ; Shirin Kord 1Transplant Research Center, Pathology Department, Shiraz University of Medical Sciences, Shiraz, IR Iran 2Dr. Alborzi Microbiology Research Center, Department of Pediatrics, Shiraz University of Medical Sciences, Shiraz, IR Iran 3Department of Pathology, Shiraz University of Medical Sciences, Shiraz, IR Iran *Corresponding Author : Bita Geramizadeh, Transplant Research Center, Pathology Department, Shiraz University of Medical Sciences, Shiraz, IR Iran. Tel: +98-9173143438, E-mail: [email protected] Received: ; Revised: ; Accepted: May 20, 2015 June 28, 2015 July 13, 2015 Introduction: Gastrointestinal basidiobolomycosis is an emerging infection, with fewer than 80 cases reported in the English literature. Case Presentation: Also, a few cases of gastrointestinal basidiobolomycosis, accompanied by liver involvement as part of a disseminated disease, have been reported. Conclusions: This is the first case report of an isolated liver involvement of this fungal infection in a 2-year-old girl, who presented with a liver mass resembling a hepatic abscess. Keywords: Liver; Basidiobolomycosis; Immunocompetent 1. Introduction Zygomycosis includes 2 orders, one of which causes fun- delivery without any specific disorder. She had had a nor- gal infections in an immunocompromised host (Mucora- mal infancy until 2 months prior to her referral, when les) and the other in an immunocompetent host (Ento- she developed abdominal pain with no response to rou- mophthorales) (1). tine treatment. Basidiobolus ranarum belongs to the second group and Physical examination was normal, except for mild hepa- is a saprophyte found mostly in soil and decaying vege- tomegaly. -

Fungal Infections
FUNGAL INFECTIONS SUPERFICIAL MYCOSES DEEP MYCOSES MIXED MYCOSES • Subcutaneous mycoses : important infections • Mycologists and clinicians • Common tropical subcutaneous mycoses • Signs, symptoms, diagnostic methods, therapy • Identify the causative agent • Adequate treatment Clinical classification of Mycoses CUTANEOUS SUBCUTANEOUS OPPORTUNISTIC SYSTEMIC Superficial Chromoblastomycosis Aspergillosis Aspergillosis mycoses Sporotrichosis Candidosis Blastomycosis Tinea Mycetoma Cryptococcosis Candidosis Piedra (eumycotic) Geotrichosis Coccidioidomycosis Candidosis Phaeohyphomycosis Dermatophytosis Zygomycosis Histoplasmosis Fusariosis Cryptococcosis Trichosporonosis Geotrichosis Paracoccidioidomyc osis Zygomycosis Fusariosis Trichosporonosis Sporotrichosis • Deep / subcutaneous mycosis • Sporothrix schenckii • Saprophytic , I.P. : 8-30 days • Geographical distribution Clinical varieties (Sporotrichosis) Cutaneous • Lymphangitic or Pulmonary lymphocutaneous Renal Systemic • Fixed or endemic Bone • Mycetoma like Joint • Cellulitic Meninges Lymphangitic form (Sporotrichosis) • Commonest • Exposed sites • Dermal nodule pustule ulcer sporotrichotic chancre) (Sporotrichosis) (Sporotrichosis) • Draining lymphatic inflamed & swollen • Multiple nodules along lymphatics • New nodules - every few (Sporotrichosis) days • Thin purulent discharge • Chronic - regional lymph nodes swollen - break down • Primary lesion may heal spontaneously • General health - may not be affected (Sporotrichosis) (Sporotrichosis) Fixed/Endemic variety (Sporotrichosis) • -

Traveler Information
Traveler Information QUICK LINKS Fungal Disease—TRAVELER INFORMATION • Introduction • Geographic Distribution • Risk Factors • Symptoms • Prevention • Need for Medical Assistance Traveler Information FUNGAL DISEASE INTRODUCTION Fungi are found in soil and on vegetation, as well as on many indoor surfaces and human skin. More than 1.5 million different species of fungi exist, but only several hundred are known to cause human infection. In healthy persons, fungal disease is generally asymptomatic or self-limited. However, infection can lead to significant disease, particularly in persons who are immune compromised. In travelers, important fungal infections to be aware of include coccidioidomycosis, histoplasmosis, and paracoccidioidomycosis. These fungal diseases are acquired by the respiratory route and often affect the respiratory system. Infections occur after inhalation of spores found in dust, soil, bird/bat guano, or decaying vegetation following excavation, construction, landscaping, earthquakes, dirt bike riding, spelunking, and other activities. GEOGRAPHIC DISTRIBUTION Coccidioidomycosis, also known as valley fever, is a fungal infection caused by fungi that grow in the soil, mainly in the southwestern United States, parts of Mexico, and Central and South America. Coccidioidomycosis is a growing health concern and a common cause of pneumonia in endemic areas. At least 30-60% of people who live in an endemic region are exposed to the fungus at some point during their lives. In most people the infection will resolve spontaneously, but for those who develop severe infections or chronic pneumonia, medical treatment is necessary. Exposures of concern include arid regions and places where excavation is occurring. Histoplasmosis is an infection caused by a fungus that grows as a mold in soil and as yeast in animal and human hosts.