Toxicity Prediction Using Multi-Disciplinary Data Integration and Novel Computational Approaches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
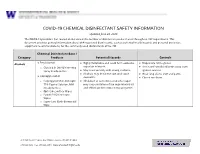
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -
AMIFOSTINE for INJECTION Incidence of Grade 2 Or Higher Xerostomia (RTOG Criteria)
TABLE 4 AMIFOSTINE FOR INJECTION Incidence of Grade 2 or Higher Xerostomia (RTOG criteria) Amifostine for RT p-value only Injection +RT LBL-7062PD Acute DESCRIPTION 51% (75/148) 78% (120/153) p<0.0001 ( 90 days from Amifostine for Injection is an organic thiophosphate cytoprotective agent known chemically ɖ start of radiation) as 2-[(3-aminopropyl)amino]ethanethiol dihydrogen phosphate (ester) and has the following structural formula: Latea 35% (36/103) 57% (63/111) p=0.0016 (9-12 months H2N(CH2)3NH(CH2)2S-PO3H2 post radiation) Amifostine is a white crystalline powder which is freely soluble in water. Its empirical aBased on the number of patients for whom actual data were available. formula is C5H15N2O3PS and it has a molecular weight of 214.22. Amifostine for Injection is the trihydrate form of amifostine and is supplied as a sterile At one year following radiation, whole saliva collection following radiation showed that lyophilized powder requiring reconstitution for intravenous infusion. Each single-use 10 mL more patients given Amifostine for Injection produced >0.1 gm of saliva (72% vs. 49%). vial contains 500 mg of amifostine on the anhydrous basis. In addition, the median saliva production at one year was higher in those patients who CLINICAL PHARMACOLOGY received amifostine (0.26 gm vs. 0.1 gm). Stimulated saliva collections did not show Amifostine is a prodrug that is dephosphorylated by alkaline phosphatase in tissues to a a difference between treatment arms. These improvements in saliva production were pharmacologically active free thiol metabolite. This metabolite is believed to be responsible supported by the patients’ subjective responses to a questionnaire regarding oral dryness. -

DE H 2281 001 PAR.Pdf
Bundesinstitut für Arzneimittel und Medizinprodukte Decentralised Procedure RMS Public Assessment Report Latanoprost Malcosa 0,005% Xalaprost 0,005% Laxatan 0,005% Pharmecol 0.005% DE/H/1999/001/DC DE/H/2281/001/DC DE/H/2282/001/DC DE/H/2382/001/DC Applicant: Malcosa Ltd. Reference Member State DE Date of this report: 06.12.2010 The BfArM is a Federal Institute within the portfolio of the Federal Ministry of Health. 1/30 CONTENTS ADMINISTRATIVE INFORMATION .............................................................................................. 3 I. RECOMMENDATION ................................................................................................................ 4 II. EXECUTIVE SUMMARY....................................................................................................... 4 II.1 Problem statement..................................................................................................................... 4 II.2 About the product ..................................................................................................................... 4 II.3 General comments on the submitted dossier .......................................................................... 5 II.4 General comments on compliance with GMP, GLP, GCP and agreed ethical principles..6 III. SCIENTIFIC OVERVIEW AND DISCUSSION ................................................................... 6 III.1 Quality aspects...................................................................................................................... -

Eosin Y Catalysed Photoredox Synthesis: a Review
RSC Advances REVIEW View Article Online View Journal | View Issue Eosin Y catalysed photoredox synthesis: a review a b Cite this: RSC Adv.,2017,7,31377 Vishal Srivastava and Praveen P. Singh * In recent years, photoredox catalysis using eosin Y has come to the fore front in organic chemistry as a powerful strategy for the activation of small molecules. In a general sense, these approaches rely on the ability of organic dyes to convert visible light into chemical energy by engaging in single-electron Received 14th May 2017 transfer with organic substrates, thereby generating reactive intermediates. In this perspective, we Accepted 13th June 2017 highlight the unique ability of photoredox catalysis to expedite the development of completely new DOI: 10.1039/c7ra05444k reaction mechanisms, with particular emphasis placed on multicatalytic strategies that enable the rsc.li/rsc-advances construction of challenging carbon–carbon and carbon–heteroatom bonds. 1. Introduction However, the transition metal based photocatalysts disadvantageously exhibit high cost, low sustainability and Visible light photoredox catalysis has recently received much potential toxicity. Recently, a superior alternative to transition Creative Commons Attribution 3.0 Unported Licence. attention in organic synthesis owing to ready availability, metal photoredox catalysts, especially metal-free organic dyes sustainability, non-toxicity and ease of handling of visible particularly eosin Y has been used as economically and 1–13 light but the general interest in the eld started much ecologically superior surrogates for Ru(II)andIr(II)complexes earlier.14 Unlike thermal reactions, photoredox processes occur in visible-light promoted organic transformations involving 18–21 under mild conditions and do not require radical initiators or SET (single electron transfer). -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

Appendix on Tariff Elimination Schedule for Mercosur
Trade part of the EU-Mercosur Association Agreement Without Prejudice Disclaimer: In view of the Commission's transparency policy, the Commission is publishing the texts of the Trade Part of the Agreement following the agreement in principle announced on 28 June 2019. The texts are published for information purposes only and may undergo further modifications including as a result of the process of legal revision. However, in view of the growing public interest in the negotiations, the texts are published at this stage of the negotiations for information purposes. These texts are without prejudice to the final outcome of the agreement between the EU and Mercosur. The texts will be final upon signature. The agreement will become binding on the Parties under international law only after completion by each Party of its internal legal procedures necessary for the entry into force of the Agreement (or its provisional application). AR applied BR applied PY applied UY applied Mercosur Final NCM Description Comments tariff tariff tariff tariff Offer 01012100 Pure-bred horses 0 0 0 0 0 01012900 Lives horses, except pure-bred breeding 2 2 2 2 0 01013000 Asses, pure-bred breeding 4 4 4 4 4 01019000 Asses, except pure-bred breeding 4 4 4 4 4 01022110 Purebred breeding cattle, pregnant or lactating 0 0 0 0 0 01022190 Other pure-bred cattle, for breeding 0 0 0 0 0 01022911 Other bovine animals for breeding,pregnant or lactating 2 2 2 2 0 01022919 Other bovine animals for breeding 2 2 2 2 4 01022990 Other live catlle 2 2 2 2 0 01023110 Pure-bred breeding buffalo, pregnant or lactating 0 0 0 0 0 01023190 Other pure-bred breeding buffalo 0 0 0 0 0 01023911 Other buffalo for breeding, ex. -

The Study Programme for the Quality Management of Essential Medicines - Good Manufacturing Practical (GMP) and Inspection
The Study Programme for the Quality Management of Essential Medicines - Good Manufacturing Practical (GMP) and Inspection - Country Reports Japan International Corporation of Welfare Services (JICWELS) Contents 1. Cambodia 1 2. Indonesia 70 3. Malaysia 91 4. Philippines 116 5. Sri Lanka 141 6. Thailand 161 The Study Programme for the Quality Management of Essential Medicines - Good Manufacturing Practical (GMP) and Inspection - Cambodia -1- KINGDOM OF CAMBODIA Nation Religion King Ministry of Health Department of Drugs and Food Country Report The Study Program on Quality Management of Essential Medicines Good Manufacturing Practice (GMP) and Inspection November 4, 2012 – November 30, 2012 Sponsored by : The Government of Japan Japan International Cooperation Agency (JICA) Department of Drugs and Food Ministry of Health, Cambodia. -2- I- COUNTRY PROFILE -3- A-Geography Cambodia is an agricultural country located in South East Asia which bordering the Gulf of Thailand, between Thailand, Vietnam, and Laos. Its approximate geographical coordinates are 13°N 105°E. Its 2,572 km border is split among Vietnam (1,228 km), Thailand (803 km) and Laos (541 km), as well as 443 km of coastline. Cambodia covers 181,035 square kilometers in the southwestern part of the Indochina, Cambodia lies completely within the tropics; its southernmost points are only slightly more than 10° above the equator. The country is bounded on the north by Thailand and by Laos, on the east and southeast by Vietnam, and on the west by the Gulf of Thailand and by Thailand. It consists of the Tonle Sap Basin and the Mekong Lowlands. To the southeast of this great basin is the Mekong Delta, which extends through Vietnam to the South China Sea. -

Tonsillopharyngitis - Acute (1 of 10)
Tonsillopharyngitis - Acute (1 of 10) 1 Patient presents w/ sore throat 2 EVALUATION Yes EXPERT Are there signs of REFERRAL complication? No 3 4 EVALUATION Is Group A Beta-hemolytic Yes DIAGNOSIS Streptococcus (GABHS) • Rapid antigen detection test infection suspected? (RADT) • roat culture No TREATMENT EVALUATION No A Supportive management Is GABHS confi rmed? B Pharmacological therapy (Non-GABHS) Yes 5 TREATMENT A EVALUATE RESPONSEMIMS Supportive management TO THERAPY C Pharmacological therapy • Antibiotics Poor/No Good D Surgery, if recurrent or complicated response response REASSESS PATIENT COMPLETE THERAPY & REVIEW THE DIAGNOSIS© Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. B269 © MIMS Pediatrics 2020 Tonsillopharyngitis - Acute (2 of 10) 1 ACUTE TONSILLOPHARYNGITIS • Infl ammation of the tonsils & pharynx • Etiologies include bacterial (group A β-hemolytic streptococcus, Haemophilus infl uenzae, Fusobacterium sp, etc) & viral (infl uenza, adenovirus, coronavirus, rhinovirus, etc) pathogens • Sore throat is the most common presenting symptom in older children TONSILLOPHARYNGITIS 2 EVALUATION FOR COMPLICATIONS • Patients w/ sore throat may have deep neck infections including epiglottitis, peritonsillar or retropharyngeal abscess • Examine for signs of upper airway obstruction Signs & Symptoms of Sore roat w/ Complications • Trismus • Inability to swallow liquids • Increased salivation or drooling • Peritonsillar edema • Deviation of uvula -

Xx250 Spc 2015 Uk
SUMMARY OF PRODUCT CHARACTERISTICS 1 NAME OF THE MEDICINAL PRODUCT XENETIX 250 (250 mgI/ml) Solution for injection. 2 QUALITATIVE AND QUANTITATIVE COMPOSITION per ml 50 ml 100 ml 200 ml 500 ml Iobitridol (INN) 548.4 mg 27.42 g 54.84 g 109.68 g 274.2 g Iodine corresponding to 250 mg 12.5 g 25 g 50 g 125 g Excipient with known effect : Sodium (up to 3.5 mg per 100 mL). For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Solution for injection. Clear, colourless to pale yellow solution 4. CLINICAL PARTICULARS 4.1. Therapeutic indications For adults and children undergoing: . whole-body CT . venography . intra-arterial digital subtraction angiography . ERP/ERCP This medicinal product is for diagnostic use only. 4.2. Posology and method of administration The dosage may vary depending on the type of examination, the age, weight, cardiac output and general condition of the patient and the technique used. Usually the same iodine concentration and volume are used as with other iodinated X-ray contrast in current use. As with all contrast media, the lowest dose necessary to obtain adequate visualisation should be used. Adequate hydration should be assured before and after administration as for other contrast media. As a guideline, the recommended dosages are as follows: Indications Recommended dosage Whole-body CT The doses of contrast medium and the rates of administration depend on the organs under investigation, the diagnostic problem and, in particular, the different scan and image-reconstruction times of the scanners in use. -

List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -

Drugs for Glaucoma
Australian Prescriber Vol. 25 No. 6 2002 Drugs for glaucoma Ivan Goldberg, Eye Associates and Glaucoma Service, Sydney Eye Hospital and the Save Sight Institute, University of Sydney, Sydney SYNOPSIS is not uncommon and the pressure slowly rises. Withdrawing Older drugs for glaucoma reduce intra-ocular pressure, the drug for a few months often re-establishes its efficacy. but often have unpleasant adverse effects. They still The main problem with timolol or levobunolol is their potential have a role in therapy, but there are now newer for systemic adverse effects. These are the same as the adverse drugs which overcome some of the problems. The topical effects of oral beta blockers, the most important of which are carbonic anhydrase inhibitors decrease the secretion of bronchoconstriction, bradyarrhythmias, and an increase in aqueous humour, while lipid-receptor agonists increase falls in the elderly. uveoscleral outflow. Alpha agonists use both mechanisms 2 As betaxolol is relatively selective for beta1 receptors it should to reduce intra-ocular pressure. If a patient needs more pose less respiratory risk. Its pharmacokinetic properties than one drug to control their glaucoma, the new drugs (higher plasma binding and larger volume of distribution) also generally have an additive effect when used in combination make it less likely to provoke other systemic effects. regimens. Miotics Index words: beta blockers, carbonic anhydrase inhibitors, Miotics (pilocarpine and carbachol) are rapidly falling out of lipid-receptor agonists. favour. While their ocular hypotensive efficacy is undisputed, (Aust Prescr 2002;25:142–6) and their systemic safety margin wide (abdominal cramping or diarrhoea are rarely reported), their use is declining because Introduction of their local effects and the need to instill them up to four Glaucoma is the second commonest cause of visual disability times daily. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE