IMPACT on the GROUND: WHO’S Action in Countries, Territories and Areas
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nationwide March to Commemorate 27Th Anniversary of Khojaly
A nationwide march has been held in Baku to commemorate the 27th anniversary of Khojaly genocide, one of the bloodiest crimes in the history of mankind. President of the Republic of Azerbaijan Ilham Aliyev, first lady Mehriban Aliyeva and family members attended the march. TheThe nationwide nationwide march, march, which which began began from from the the Azadlyg Azadlyg Square Square in inKhatai Khatai district, district, involves involves ten ten thousands thousands of of people.people. They They gathered gathered to to pay pay tribute tribute to to victims victims of of Khojaly Khojaly tragedy tragedy and and draw draw the the world world community`s community`s attention attention to to this this crime against humanity, which was committed by the Armenian fascists. WithWith President President Ilham Ilham Aliyev Aliyev and and first first lady lady Mehriban Mehriban Aliyeva Aliyeva in in the the front front row, row, the the marchers marchers started started moving moving in in thethe directiondirection ofof thethe KhojalyKhojaly memorialmemorial inin KhataiKhatai district.district. Thousands of young people gathered along the avenues and streets that the marchers are moving. They hold portraitsportraits of innocent of innocent victims victims of the of bloodythe bloody event event – slaughtered – slaughtered children, children, women women and andelders elders – photos – photos depicting depicting abominableabominable scenesscenes ofof slaughter,slaughter, placardsplacards demandingdemanding toto bringbring toto accountaccount andand -

Health Corps Station, One of About 400 Similar Health to Help Alleviate This Great Shortage, Iran Centres Found Throughout Rural Iran
P42 ARCHIV IDRC-074e MOUSSE - 22580 a a ER7.1;. _ An, -- ( Proceedings of a workshop held at Shiraz, Iran, 6-13 March 1976 Editors: H.A.Ronaghy, Y. Mousseau-Gershman, and Alexandre Dorozynski © 1976 International Development Research Centre Postal Address: Box 8500, Ottawa, Canada K1G 3H9 Head Office: 60 Queen Street, Ottawa Ronaghy, H.A. Mousseau-Gershman, Y. Dorozynski, A. Village health workers: proceedings of a workshop held at Shiraz, Iran, 6-13 March 1976. Ottawa, IDRC, 1976. 48p. /IDRC pub CRDI/. Compilation of seminar papers on /health service/s in /rural area/s of /Iran/, /Nepal/, the /Philippines/, /Thailand/ and /Papua/ /New Guinea/, with emphasis on the /training/ of /auxiliary health worker/s includes /list of participants/, /statistical data/. UDC: 614.2 ISBN: 0-88936-106-1 Microfiche Edition $1 Layout and design: S. Clerget-Vaucouleurs IDRC-074e Proceedings of a workshop held at Shiraz, Iran, 6-13 March 1976 Editors: H.A. Ronaghy, Y. Mousseau-Gershman, and Alexandre Dorozynski p3928 The views expressed in this publication are those of the individual authors and do not necessarily represent the views of IDRC. Contents Foreword Y. Mousseau-Gershman 5 iran Village health workers in Iran Hossain A. Ronaghy 6 Middle level health workers training project in Iran Hossain A. Ronaghy 11 Evaluation of Iranian village health workers efficacy Bahram Zeighami and Elaine Zeighami 14 Health or development? Training of frontline health workers, particularly in Lorestan, Iran M. Taghi Farvar 21 nepal Health care in Nepal Moin Shah 25 !IL t_Jtppines Health care in the Philippines within a total framework Victor N. -

Cruising Guide to the Philippines
Cruising Guide to the Philippines For Yachtsmen By Conant M. Webb Draft of 06/16/09 Webb - Cruising Guide to the Phillippines Page 2 INTRODUCTION The Philippines is the second largest archipelago in the world after Indonesia, with around 7,000 islands. Relatively few yachts cruise here, but there seem to be more every year. In most areas it is still rare to run across another yacht. There are pristine coral reefs, turquoise bays and snug anchorages, as well as more metropolitan delights. The Filipino people are very friendly and sometimes embarrassingly hospitable. Their culture is a unique mixture of indigenous, Spanish, Asian and American. Philippine charts are inexpensive and reasonably good. English is widely (although not universally) spoken. The cost of living is very reasonable. This book is intended to meet the particular needs of the cruising yachtsman with a boat in the 10-20 meter range. It supplements (but is not intended to replace) conventional navigational materials, a discussion of which can be found below on page 16. I have tried to make this book accurate, but responsibility for the safety of your vessel and its crew must remain yours alone. CONVENTIONS IN THIS BOOK Coordinates are given for various features to help you find them on a chart, not for uncritical use with GPS. In most cases the position is approximate, and is only given to the nearest whole minute. Where coordinates are expressed more exactly, in decimal minutes or minutes and seconds, the relevant chart is mentioned or WGS 84 is the datum used. See the References section (page 157) for specific details of the chart edition used. -

African Traditional Medicine Day Rganization Regional Office for Africa O Rganization of the World H Ealth a Serial Publication
august 2010 · special issue 14 · a serial publication of the World health organization regional office for africa · issn 2077 6136 tHe AfricAn monitor Healt 31 August 31 Day Medicine Traditional African special H issue r EG i O n AL O ffic E f O r Africa The African Health Monitor is a magazine of the World Health Organization Regional Office for Africa (WHO- AFRO) published four times a year (January, April, July and October). It is a multilingual publication with peer- reviewed articles in English, French and Portuguese. REGIONAL OFFICE FOR Africa The aim of the African Health Monitor is to promote and facilitate evidence-based policy and decisions to strengthening programmes for health promotion, protection, and restoration in the African Region. In order to achieve its aim, the Monitor serves as a medium for publication of articles that monitor the health n A situation and trends, and track progress toward the health-related Millennium Development Goals and other internationally agreed-upon goals. It will publish and disseminate relevant and scientifically rigorous public HealtH health information. It will also disseminate information on public health interventions carried out in the Member States with the cooperation of AFRO technical programmes. Afric e Prospective authors should follow the Monitor stylesheet, which can be obtained by sending an email H t monitor message to the Editorial Office at [email protected] or by using this intranet link http://intranet.afro.who.int/ guidelines/ahm.pdf african traditional Paul Lusamba-Dikassa (Editor-in-Chief) for the African Health Monitor Special Issue on Traditional Medicine medicine day, 31 august EditorialUche Amazigo Board ExpErt adviSorY panel special issue Rufaro Chatora Dr Kofi Busia, WAHO, Burkina Faso Alimata J. -

Dietary Sodium and Potassium Intake and Their Association with Blood Pressure in a Non-Hypertensive Iranian Adult Population: Isfahan Salt Study
View metadata, citation and similar papers at core.ac.uk brought to you by CORE Nutrition & Dietetics 2016 DOI: 10.1111/1747-0080.12304provided by shahrekord university of medical scinces Australia Dietitians f of o Association A A D ORIGINAL RESEARCH Dietary sodium and potassium intake and their association with blood pressure in a non-hypertensive Iranian adult population: Isfahan salt study Noushin MOHAMMADIFARD,1,2 Arsalan KHALEDIFAR,3,4 Alireza KHOSRAVI,2,4 Fatemeh NOURI,1 Ali POURMOGHADAS,4 Awat FEIZI,5,6 Ahmad ESMAILLZADEH7,8,9 and Nizal SARRAFZADEGAN1 1Isfahan Cardiovascular Research Centre, 2Hypertension Research Centre, Cardiovascular Research Institute, Isfahan University of Medical Sciences, Isfahan and 3Department of Cardiology, School of Medicine, Hajar Hospital, Modeling in Health Research Centre, Shahrekord University of Medical Sciences, Shahrekord, 4Interventional Cardiology Research Centre, 5Epidemiology and Biostatistics Department, 6Cardiac Rehabilitation Research Centre, Cardiovascular Research Institute, 7Food Security Research Centre, 8Department of Community Nutrition, Isfahan University of Medical Sciences, Isfahan, and 9Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran Abstract Aim: The association of sodium (Na) and potassium (K) intake with blood pressure (BP) is an ongoing debate, espe- cially in central Iran. We aimed to examine the mean Na and K intake, major sources of Na and the relationship between BP and dietary and urinary Na and K. Methods: This cross-sectional study was performed in central Iran in 2013–2014. A total of 796 non-hypertensive adults aged >18 years were randomly recruited. The semi-quantitative food frequency questionnaire was used to assess dietary Na and K intake. -
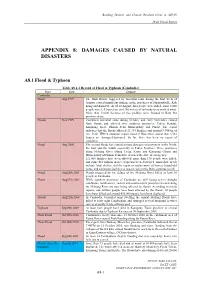
Appendix 8: Damages Caused by Natural Disasters
Building Disaster and Climate Resilient Cities in ASEAN Draft Finnal Report APPENDIX 8: DAMAGES CAUSED BY NATURAL DISASTERS A8.1 Flood & Typhoon Table A8.1.1 Record of Flood & Typhoon (Cambodia) Place Date Damage Cambodia Flood Aug 1999 The flash floods, triggered by torrential rains during the first week of August, caused significant damage in the provinces of Sihanoukville, Koh Kong and Kam Pot. As of 10 August, four people were killed, some 8,000 people were left homeless, and 200 meters of railroads were washed away. More than 12,000 hectares of rice paddies were flooded in Kam Pot province alone. Floods Nov 1999 Continued torrential rains during October and early November caused flash floods and affected five southern provinces: Takeo, Kandal, Kampong Speu, Phnom Penh Municipality and Pursat. The report indicates that the floods affected 21,334 families and around 9,900 ha of rice field. IFRC's situation report dated 9 November stated that 3,561 houses are damaged/destroyed. So far, there has been no report of casualties. Flood Aug 2000 The second floods has caused serious damages on provinces in the North, the East and the South, especially in Takeo Province. Three provinces along Mekong River (Stung Treng, Kratie and Kompong Cham) and Municipality of Phnom Penh have declared the state of emergency. 121,000 families have been affected, more than 170 people were killed, and some $10 million in rice crops has been destroyed. Immediate needs include food, shelter, and the repair or replacement of homes, household items, and sanitation facilities as water levels in the Delta continue to fall. -

Reproductive Knowledge, Attitudes and Behavior Among Adolescent Males in Tehran, Iran
Reproductive Knowledge, Attitudes and Behavior Among Adolescent Males in Tehran, Iran CONTEXT: Iran’s culture and religion prohibit sexual contact prior to marriage. Due to the sensitivity of the topic, little By Mohammad is known about the sexual activity of unmarried adolescent males or about their knowledge of, and attitudes toward, Reza Mohammadi, sexuality and reproductive health. Kazem Mohammad, Farideh K.A. METHODS: A population-based study of 1,385 males aged 15–18 in Tehran was conducted using a self-administered Farahani, questionnaire. Participants were questioned about their beliefs and knowledge regarding reproductive health, and Siamak Alikhani, asked whether they had engaged in sexual activity. Bivariate and multivariate analyses were performed to identify Mohammad Zare, factors associated with sexual knowledge, attitudes and behavior. Fahimeh R. Tehrani, Ali Ramezankhani RESULTS: Twenty-eight percent of the sample reported having engaged in sexual activity. Sexual experience was asso- and Farshid ciated with older age, access to satellite television, alcohol consumption and permissive attitudes toward sex. Sub- Alaeddini. stantial proportions of respondents held misconceptions regarding condoms, STIs and reproductive physiology. Atti- tudes toward premarital sex were more permissive among respondents who were older, were not in school, had work Mohammad Reza experience, had access to the Internet or satellite television, lived separately from their parents, or reported having Mohammadi is chair, used alcohol, cigarettes or drugs. child and adolescent psychiatry, Tehran CONCLUSION: The relatively high prevalence of sexual activity and the lack of knowledge regarding STIs and contra- University of Medical ceptives pose a significant threat to the sexual and reproductive health of adolescent males in Iran. -

Defeating Malaria Through Pharmaceutical Systems Strengthening Results from the Systems for Improved Access to Pharmaceuticals and Services (SIAPS) Program
DEFEATING MALARIA THROUGH PHARMACEUTICAL SYSTEms STRENGTHENING Results from the Systems for Improved Access to Pharmaceuticals and Services (SIAPS) Program Seydou Doumbia, Aubrey Clark, and Andwele Mwansasu Acknowledgements The authors would like to thank the 70+ in-country staff, partners, and stakeholders who shared their insights through in-depth interviews, without which this report would not have been possible. Photos taken by Aubrey Clark (MSH/SIAPS) unless otherwise noted. ABOUT SIAPS | The Systems for Improved Access to Pharmaceuticals and Services (SIAPS) program works to ensure access to quality pharmaceutical products and effective pharmaceutical services through systems-strengthening approaches to achieve positive and lasting health outcomes. SIAPS is funded by the US Agency for International Development (USAID) and implemented by Management Sciences for Health. For more information, visit www.SIAPSprogram.org. The information provided in this document does not reflect or represent the position or views of the US Agency for International Development or the US Government. ACRONYMS ACT artemisinin-based combination therapy APTS Auditable Pharmacy Transactions and Services CRMS Continuous Results Monitoring System DNPL Direction Nationale de la Pharmacie et des Laboratoires DRC Democratic Republic of the Congo DTC drug and therapeutics committee EML essential medicines list EUV End Use Verification GFATM Global Fund to Fight AIDS, TB, and Malaria IPTp intermittent preventive treatment in pregnancy LMIS logistics management information -
Corruption and Integrity Programme
Anti-Corruption and Integrity Programme A Study on the Link between Corruption and the Causes of Migration and Forced Displacement Human CorruptionSecurity Published by: A Study on the Link between Corruption and the Causes of Migration and Forced Displacement March 29, 2017 Authors: Ortrun Merkle* Julia Reinold* Melissa Siegel* *Maastricht Graduate School of Governance The publication “A Study on the Link between Corruption and the Causes of Migration and Forced Displacement” was commissioned by the Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ) GmbH, Anti-Corruption and Integrity Programme, on behalf of the German Federal Ministry for Economic Cooperation and Development (BMZ). The contents of this publication do not represent the official position of neither BMZ nor GIZ. Table of Content 3 Table of Content List of Figures ..........................................................5 List of Tables...........................................................6 List of Boxes ...........................................................7 Acknowledgments .......................................................7 Abbreviations ...........................................................7 Executive Summary ......................................................9 1. Introduction ........................................................10 2. Mapping the Conceptual Terrain: Corruption and Migration .....................13 2.1. Corruption - what do we mean? 13 2.2. The concept of human security 16 2.3. Migration – the background 18 3. Methodology -

Words: Corner Beam-Column Joint; Hysteresis Loops; Seismic Design; Ductility; Stiffness; Equivalent Viscous Damping
Journal of Mechanical Engineering Vol 16(1), 213-226, 2019 Validation of Corner Beam-column Joint’s Hysteresis Loops between Experimental and Modelled using HYSTERES Program N.F. Hadi, M. Mohamad Faculty of Civil Engineering, Universiti Teknologi MARA 40450 Shah Alam, Selangor, Malaysia N.H. Hamid Institute of Infrastructure Engineering Sustainability and Management Universiti Teknologi MARA 40450 Shah Alam, Selangor, Malaysia ABSTRACT The beam - column joint is an important part of a multi-storey RC building as it caters for lateral and gravitational load during an earthquake event. The beam-column joints should have a medium to high ductility for transferring the earthquake load and gravity load to the foundation. By designing multi- storey RC buildings using Eurocode 8 can avoid any diagonal shear cracks in column which is a major problem in non-seismic design buildings using British Standard (BS8110). This paper presents the experimental hysteresis loops of monolithic corner beam-column joints of multi-storey building which had been designed using Eurocode 8 and tested under in-plane lateral cyclic loading. The experimental hysteresis loops of corner beam-column joint was compared with modelled using the HYSTERES program. The full-scale corner beam- column joint of a two story precast school building was designed, constructed, tested and modelled is presented herein. The seismic performance parameters such as lateral strength capacity, stiffness, ductility and equivalent viscous damping were compared between experimental and modelled hysteresis loops. The experimental hysteresis loops have similar shape with the modeling hysteresis loops with small percentage differences between them. Keywords: Corner beam-column joint; hysteresis loops; seismic design; ductility; stiffness; equivalent viscous damping ___________________ ISSN 1823-5514, eISSN2550-164X Received for review: 2017-07-10 © 2016 Faculty of Mechanical Engineering, Accepted for publication: 2018-05-18 Universiti Teknologi MARA (UiTM), Malaysia. -

Regime Stability in Azerbaijan
REGIME STABILITY IN AZERBAIJAN Despite predictions of a fourth wave of democratization and the assumption that socio-economic development would lead to democratization, Azerbaijan has consolidated a political system with authoritarian features. This article identifies both the domestic pillars of stability –the ability to spend, repress, and create patronage networks as a result of significant hydrocarbon revenues– and the international apathy that have produced this remarkable political stability. It concludes by arguing that the current strategies to create stability and legitimacy are likely to be unsustainable. Therefore, in the next few years it will be crucial for Azerbaijan to introduce reforms to gradually make the country more democratic, as well as encourage the population to make a living independently, so the economy can be diversified and sustained by taxes. Isabelle Langerak* Winter 2014 * Isabelle Langerak was a research intern at the Georgian Foundation for Strategic and International Studies (GFSIS) in Tbilisi when she wrote this article. She is currently a student at Durham University in the UK. 125 VOLUME 12 NUMBER 4 ISABELLE LANGERAK he history of modern Azerbaijan is closely associated with that of the Aliyev family. For the most part of the past four decades the Aliyevs have ruled Azerbaijan and shaped its politics. Heydar Aliyev ruled T Azerbaijan from 1969 until his forced retirement in 1987 as first sec- retary of the Azerbaijani Communist Party and again after retaking power in 1993, ruling Azerbaijan until his -
Waho-2017-Annual-Report.Pdf
WAHO/XIX.AHM/2018/REP-doc. WEST AFRICAN HEALTH ORGANISATION ORGANISATION OUEST AFRICAINE DE LA SANTE ORGANIZACAO OESTE AFRICANA DA SAUDE 2017 ANNUAL REPORT March 2018 GLOSSARY AGM: Annual General Meeting AMRH: African Medicines Regulation Harmonization AHM: Assembly of Health Ministers AREF: Africa Excellence Research Fund ARVs: Anti-Retro Viral Drugs WB: World Bank BMGF: Bill and Melinda Gates Foundation GMP: Good Manufacturing Practices GPH: Good Practices in Health BCC: Behaviour Change Communication ECOWAS: Economic Community of West African States UTH: University Teaching Hospital NACI: National Advisory Committee on Immunization CORDS: Connecting Organizations for Regional Disease Surveillance SMC: Seasonal Malaria Chemoprevention IDRC: International Development Research Center RCSDC: Regional Centre for Surveillance and Disease Control CTD: Common Technical Document DIHS2: District Health Information System 2 DDEC: Department of Disease and Epidemics Control DTC3: Diphtheria Tetanus Pertussis 3 DTCP: Diphtheria Tetanus Pertussis Poliomyelitis ECOWAS: Economic Community of West African States EQUIST: Equitable Strategies to save lives ERRRT: ECOWAS Regional Rapid Response Team FASFAF: Federation of French-speaking Africa Midwives Associations NITAG: National Immunization Technical Advisory Group HKI: Helen Keller International IATA: International Air Transport Association CBIs: Community-based Interventions IOTA: Tropical Ophthalmology Institute of Africa IPSAS: International Public Sector Accounting Standards IRSP: Regional Institute