312.1.Full.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Verily Forms Strategic Alliances with Novartis, Otsuka, Pfizer and Sanofi
Verily Forms Strategic Alliances with Novartis, Otsuka, Pfizer and Sanofi to Transform Clinical Research Leading biopharmaceutical organizations join Project Baseline initiative to engage more patients and clinicians in research and speed evidence generation South San Francisco, CA -- May 21, 2019 -- Verily, an Alphabet company, today announced strategic alliances with Novartis (NYSE: NVS), Otsuka (NYSE: OTSKY), Pfizer Inc. (NYSE: PFE) and Sanofi (EURONEXT: SAN, NASDAQ: SNY) to develop digitally innovative, patient-centered clinical research programs using Project Baseline’s evidence generation platform and tools. The Baseline Platform is designed to engage more patients and clinicians in research, increase the speed and ease of conducting studies and collect more comprehensive, higher quality data, including outside the four walls of a clinic. Across the United States, the number of people participating in clinical research -- including clinical trials and observational studies -- is less than 10% of the population.1 In addition to low participation, challenges in research include data fragmentation, inefficient operations and limited value for patients. Alongside academic research institutions, patient-advocacy groups and health systems, Verily and its industry partners aim to implement a more patient-centric, technology-enabled approach to research, and increase the number and diversity of clinical research participants. They will also explore novel approaches to generating real-world evidence using the Baseline Platform to collect, organize and activate health information from electronic health records, sensors and other digital sources. Over the coming years, Novartis, Otsuka, Pfizer and Sanofi each plan to launch clinical studies leveraging the platform across diverse therapeutic areas, such as cardiovascular disease, oncology, mental health, dermatology and diabetes. -

SEB Fund 1 AR 31122019 Final Post BM
Annual Report SEB Fund 1 Status: 31 December 2019 R.C.S K 49 Notice The sole legally binding basis for the purchase of units of the Fund described in this report is the latest valid Sales Prospectus with its terms of contract. Table of Contents Page Additional Information to the Investors in Germany 2 Organisation 3 General Information 5 Management Report 9 Schedule of Investments: SEB Fund 1 - SEB Asset Selection Fund 10 SEB Fund 1 - SEB Europe Index Fund 14 SEB Fund 1 - SEB Global Fund 24 SEB Fund 1 - SEB Global Chance / Risk Fund 33 SEB Fund 1 - SEB Norway Focus Fund 39 SEB Fund 1 - SEB Sustainability Fund Europe 41 SEB Fund 1 - SEB Sustainability Nordic Fund 46 SEB Fund 1 - SEB US All Cap 48 Combined Statement of Operations 50 Combined Statement of Changes in Net Assets 54 Combined Statement of Net Assets 58 Statistical Information 62 Notes to the Financial Statements 74 Audit Report 81 Risk Disclosure (unaudited) 84 Remuneration Disclosure (unaudited) 86 1 Additional Information to the Investors in Germany As at 31 December 2019 Units in circulation: The following Sub-Funds are publicly approved for distribution in Germany: • SEB Fund 1 - SEB Asset Selection Fund • SEB Fund 1 - SEB Global Fund • SEB Fund 1 - SEB Global Chance / Risk Fund • SEB Fund 1 - SEB Sustainability Fund Europe • SEB Fund 1 - SEB Sustainability Nordic Fund The following Sub-Funds are not distributed in Germany: • SEB Fund 1 - SEB Europe Index Fund • SEB Fund 1 - SEB Norway Focus Fund • SEB Fund 1 - SEB US All Cap The information disclosed above is as at 31 December 2019 and this may change after the year end. -

CA Signed Novartis 315 Settlement Agreement Signed California
STATE SETTLEMENT AGREEMENT I. PARTIES This Settlement Agreement (the "Agreement") is entered into between the State of California ("the State") and Novartis Pharmaceuticals Corporation ("Novartis"), collectively, "the Parties." II. PREAMBLE As a preamble to this Agreement, the Parties agree to the following: A. At all relevant times, Novartis, (a subsidiary of Novartis International AG, which is headquartered in Basel, Switzerland) was a corporation with its principal place of business in East Hanover, New Jersey, distributed, marketed and/or sold pharmaceutical products in the United States, including drugs sold under the trade names of Lotrel, Valturna, Starlix, Tekamlo, Diovan, Diovan HCT, Tekturna, Tekturna HCT, Exforge, and Exforge HCT (the "Covered Drugs"). B. On January 5, 2011 , Oswald Bilotta, (the "Relater") filed a sealed qui tam action, which was subsequently amended on October 19, 2012, as of right on April 3, 2013 (pursuant to an unopposed motion dated March 21 , 2013), and on July 10, 2013 (pursuant to a stipulation dated July 8, 2013) (the "Civil Action") in the United States District Court for the Southern District of New York captioned United States of America et al. , ex rel. Oswald Bilotta et al. v. Novartis Pharmaceuticals Corporation Civil Action No. 1 l-cv-00071 , alleging, inter alia, that Novartis violated the False Claims Act ("FCA") and the Anti-Kickback Statute, 42 U.S.C. §I320a-7b(b) (the "AKS"), by paying doctors remuneration to prescribe the drugs Lotrel, Valturna, Starlix, Tekturna, Tekturna HCT, Diovan, Diovan HCT, Exforge, and Exforge HCT through the mechanism ofspeaker program honoraria and related misconduct. Novartis-315 Page 1 of 19 On April 26, 2013, the United States intervened in the Civil Action against Novartis by filing a Notice of Election to Intervene and Complaint-in-Intervention, in which it is asserted that claims against Novartis under the FCA and common law. -
Event Calendar
Published on Novartis (https://www.novartis.com) Home > Printer-friendly PDF > Event Calendar Event Calendar View recent presentations and learn more about upcoming events. Disclaimer: Disclaimer: The information in the presentations on these pages was factually accurate on the date of publication. These presentations remain on the Novartis website for historical purposes only. Novartis assumes no responsibility to update the information to reflect subsequent developments. Readers should not rely upon the information in these pages as current or accurate after their publication dates. Tab: Upcoming Events Third quarter results 2021 Oct 26, 2021 Basel, Switzerland Recent Events [1] ESG Investor Day Sep 30, 2021 Watch the webcast [2] Download the podcast (MP3 66 MB) [3] Access our interactive slide deck (PDF 9.6 MB) [4] Read the media release [5] Novartis ESG Investor Day 2021 6 key takeaways [6] Bernstein Strategic Decisions Conference Sep 23, 2021 Baader Investment Conference Sep 21, 2021 Bank of America Merrill Lynch Global Healthcare Virtual Conference Sep 15, 2021 Morgan Stanley Global Healthcare Conference Sep 13, 2021 Citi's GEMS Virtual Conference 2021 Sep 8, 2021 Second quarter results 2021 Jul 21, 2021 Basel, Switzerland Media release English (PDF 0.4 MB) [7] Deutsch (PDF 0.4 MB) [8] Français (PDF 0.4 MB) [9] Interim financial report (PDF 0.5 MB) [10] Watch the webcast [11] Read the presentation transcript [12] Download the podcast (MP3 45 MB) [13] Download the interactive presentation (PDF 4.5 MB) [14] Novartis ESG Update - July -

Annual Report 2014
ANNUAL REPORT 2014 Dress €99 Blazer €19.99 H&M SPRING 2015 MODERN ESSENTIALS SELECTED BY DAVID BECKHAM SPRING 2015 Shirt €19.99 H&M SPRING 2014 Sweater € 19.95 — H&M ANNUAL REPORT 2014 — Contents H&M IN WORDS AND PICTURES This is H&M 8 CEO letter 10 2014 in brief 12 Our brands 16 Sustainable development 36 Our employees 42 Expansion 46 History 54 H&M IN FIGURES Administration report, including proposed distribution of earnings 60 Group income statement 66 Consolidated statement of comprehensive income 66 Group balance sheet 67 Group changes in equity 68 Group cash flow statement 69 Parent company income statement 70 Parent company statement of comprehensive income 70 Parent company balance sheet 71 Parent company changes in equity 72 Parent company cash flow statement 73 Notes to the financial statements 74 Signing of the annual report 90 Auditor’s report 91 Corporate governance report, including information about the board of directors 92 Auditor’s statement on the corporate governance report 104 Five year summary 106 The H&M share 107 Financial information and contact details 108 H&M’s annual accounts and consolidated accounts for the financial year 2013/14 comprise pages 60–90. — THIS IS H&M — Fashion and quality at the best price H&M is a leading global fashion company with strong values and a clear business concept. H&M has a passion for fashion, a belief in people and a desire to always exceed customers’ expectations – and to do so in a sustainable way. H&M’s busi- ness concept is to offer fashion and quality at the best price. -

Investor Presentation
Participants Company overview Pharmaceuticals Oncology Financial review Conclusion Appendix References Q1 2021 Results Investor presentation 1 Investor Relations │ Q1 2021 Results Participants Company overview Pharmaceuticals Oncology Financial review Conclusion Appendix References Disclaimer This presentation contains forward-looking statements within the meaning of the United States Private Securities Litigation Reform Act of 1995, that can generally be identified by words such as “potential,” “expected,” “will,” “planned,” “pipeline,” “outlook,” or similar expressions, or by express or implied discussions regarding potential new products, potential new indications for existing products, potential product launches, or regarding potential future revenues from any such products; or regarding the impact of the COVID-19 pandemic on certain therapeutic areas including dermatology, ophthalmology, our breast cancer portfolio, some newly launched brands and the Sandoz retail and anti-infectives business, and on drug development operations; or regarding potential future, pending or announced transactions; regarding potential future sales or earnings of the Group or any of its divisions; or by discussions of strategy, plans, expectations or intentions; or regarding the Group’s liquidity or cash flow positions and its ability to meet its ongoing financial obligations and operational needs; or regarding our collaboration with Molecular Partners to develop, manufacture and commercialize potential medicines for the prevention and treatment of COVID- 19 and our joining of the industry-wide efforts to meet global demand for COVID-19 vaccines and therapeutics by leveraging our manufacturing capacity and capabilities to support the production of the Pfizer-BioNTech vaccine and to manufacture the mRNA and bulk drug product for the vaccine candidate CVnCoV from CureVac. -

Amc Lapis Glob Top 20 Gen Revol
Data as of 31.08.2021 August 2021 AMC LAPIS GLOB TOP 20 GEN REVOL PRODUCT STRATEGY FACTS AND FIGURES ISIN CH1103333931 The AMC on "LAPIS GLOBAL TOP 20 GENOMIC Currency USD REVOLUTION" is an actively managed portfolio of equities, which is based on investment Maturity Date Open End advice and recommendation by Lapis Asset NAV Date 30.08.2021 Management AG. The Lapis Global Top 20 Genomic Revolution is composed of the worldwide best-known Valor 110333393 and leading top 20 companies (gene therapy, Dividend Reinvested bioinformatics, bio-inspired computing, molecular medicine, pharmaceutical innovation) based on the FX Overlay Disabled research approach of an internationally recognized Issue Date 19.05.2021 company. All stocks are equally weighted and the NAV 110.20 certificate is rebalanced on a quarterly basis (end of January, April, July and October). Mgmt Fee (total) 1.35% Rebalancing Quarterly AuM USD 6’790’721 Components 21 Certificates 61’790 Issuer Bank Julius Baer Last Rebalancing 02.07.2021 PERFORMANCE 1 month -0.81% 52 week high 123.40 3 months 2.04% 52 week low 100.00 1 year N/A All-time high 123.40 Since inception 10.20% All-time low 100.00 YTD N/A Max draw down -14.67% Data as of 31.08.2021 August 2021 PRICE CHART MONTHLY RETURNS 2015 120 2016 115 2017 110 2018 105 2019 2020 100 8.00 13.61 -9.45 -0.81 2021 19 May 8 Jun 29 Jun 19 Jul 9 Aug 30 Aug Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec UNDERWATER EQUITY CURVE PERFORMANCE ANNUAL 0% 10% -5% 8% 2017 - 2018 - 6% 2019 - -10% 2020 - 4% 2021 10.20% 2% -15% 0% 19 May 8 Jun 29 -
Creating the Technology to Connect the World
Nokia Annual Report on Form 20-F 2019 on Form Nokia Annual Report Creating the technology to connect the world Nokia Annual Report on Form 20-F 2019 As filed with the Securities and Exchange Commission on March 5, 2020 UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 20-F ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the fiscal year ended December 31, 2019 Commission file number 1-13202 Nokia Corporation (Exact name of Registrant as specified in its charter)) Republic of Finland (Jurisdiction of incorporation) Karaportti 3 FI-02610 Espoo, Finland (Address of principal executive offices) Esa Niinimäki, Deputy Chief Legal Officer, Corporate, Telephone: +358 (0) 10 44 88 000, Facsimile: +358 (0) 10 44 81 002, Karakaari 7, FI 02610 Espoo, Finland (Name, Telephone, E-mail and/or Facsimile number and Address of Company Contact Person) Securities registered pursuant to Section 12(b) of the Securities Exchange Act of 1934 (the “Exchange Act”): Title of each class Trading Symbol(s) Name of each exchange on which registered American Depositary Shares NOK New York Stock Exchange Shares New York Stock Exchange(1) (1) Not for trading, but only in connection with the registration of American Depositary Shares representing these shares, pursuant to the requirements of the Securities and Exchange Commission. Securities registered pursuant to Section 12(g) of the Exchange Act: None Securities for which there is a reporting obligation pursuant to Section 15(d) of the Exchange Act: None Indicate the number of outstanding shares of each of the registrant’s classes of capital or common stock as of the close of the period covered by the annual report. -

French Competition Law Newsletter, October 2020
October 2020 French Competition Law Newsletter — Highlights — The French Competition Authority fines three pharmaceutical companies for abuse of collective dominance — The French Cour de cassation upholds the Paris Court of Appeals’ judgment in the TDF abuse of dominance case — The Cour de cassation quashes the Paris Court of Appeals’ decision in the SFR/Orange case on the fixed telephony market for secondary homes for the second time The French Competition Authority fines three pharmaceutical companies for abuse of collective dominance On September 9, 2020, the French Competition of cancer. Bevacizumab was licensed to its Authority (“FCA”) fined Novartis, Roche and its parent company Roche for distribution outside subsidiary Genentech €444 million for abusing of the United States, and was granted a market their collective dominance on the market for authorization by the European Commission in AMD treatment. The FCA found that the parties 2005. In parallel, having found that Avastin could disparaged the off-label use of Roche’s Avastin also help treat age-related macular degeneration drug and spread an alarmist discourse before (“AMD”), Genentech developed and started the public authorities in order to preserve the selling ranibizumab, a specific molecule (sold dominant position and high price of Novartis’ under the name of Lucentis) that it considered Lucentis drug. more appropriate for treating AMD. Lucentis was licensed to Novartis for distribution outside of Background the United States, and was granted an EU market authorization in 2007. Novartis, already at that In the late 1990ies, US pharmaceutical company time, was one of Roche’s shareholders with a Genentech developed a revolutionary active 33,33% share of the voting rights. -

Executive Summary 1
Executive Summary 1 2 Novartis Pharmaceutical Production campus Executive Summary Cushman & Wakefield, Inc., as exclusive agent, is offering the Novartis Suffern Pharmaceutical Production Campus (the “Property”) for sale. This 585,000 SF multi-building complex is one of the nation’s top ten pharmaceutical manufacturing and packaging plants, with an annual solid dosage capacity in the billions. Owned and operated by Novartis, the Property has served as a vital U.S. production facility for the Company. Due to recent organizational changes and adjustments to the company’s product lines, Novartis will be vacating the facility by year end 2015. The offering provides a buyer with a rare opportunity to purchase an equipped, high-capacity pharmaceutical plant in the New York-New Jersey region. The location and size of the Campus also supports the potential redevelopment of the site for an alternative industrial use. Executive Summary 3 4 Novartis Pharmaceutical Production campus The Campus contains three interconnected buildings including a 55,000 SF office/head building which features a 7,000 SF full-service cafeteria, multiple conference/meeting rooms, and analytical laboratories. The 425,000 SF production/manufacturing building is designed as a multi-product, high volume manufacturing operation with flexible and efficient product flow; the production building contains specialized areas including granulation suites, blending rooms, encapsulation suites, analytical laboratories, inspection areas and packaging lines. The layout of the Complex facilitates the transfer of packaged products to the warehouse/shipping area; the 74,000 SF receiving and warehouse building features 90’ ceiling heights and a fully automated racking system with over 11,500 pallet positions. -
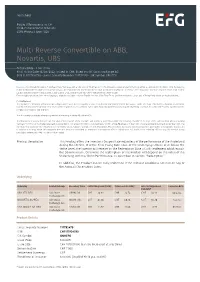
Multi Reverse Convertible on ABB, Novartis, UBS
Termsheet Public Offering only in: CH Yield-Enhancement Products SSPA Product Type: 1220 Multi Reverse Convertible on ABB, Novartis, UBS Autocallable - Low Strike Final Fixing Date 16/09/2022; issued in CHF; listed on SIX Swiss Exchange AG ISIN CH1117924790 - Swiss Security Number 111792479 - SIX Symbol GNHEFG Investors should read the section “Significant Risks” below as well as the section “Risk Factors” of the relevant Issuance and Offering Programme, as amended from time to time. By investing in this product (the "Product"), the Investor may put the capital that he invested in this Product at risk and, in addition, transaction costs may incur. Investors may lose some or all of their capital invested in the Product as well as transaction costs. Investors are exposed to the credit risk of the Issuer. Even though translations into other languages might be available, only the English version of the Final Terms and the relevant Issuance and Offering Programme are legally binding. For Switzerland: This Product is a derivative instrument according to Swiss law. It does not qualify as unit of a collective investment scheme pursuant to article 7 et seqq. of the Swiss Federal Act on Collective Investment Schemes ("CISA") and is therefore neither registered nor supervised by the Swiss Financial Market Supervisory Authority FINMA. Investors do not benefit from the specific investor protection provided under the CISA. This document constitutes advertising within the meaning of article 68 of the FinSA. This document is a termsheet prepared in view of the issuance of the Products and neither a prospectus within the meaning of article 35 et seqq. -

Buyback of Own Shares for the Purpose of a Capital Reduction Trading on a Second Trading Line on SIX Swiss Exchange
Buyback of own shares for the purpose of a capital reduction Trading on a second trading line on SIX Swiss Exchange ABB Ltd, Zurich On 25 March 2021, the Board of Directors of ABB Ltd, Affolternstrasse 44, 8050 Zurich ("ABB") decided to repurchase its registered shares for a maximum amount of USD 4.3 billion for the purpose of a capital reduc- tion. The Board of Directors of ABB intends to propose to future Annual General Meetings capital reductions through the cancellation of the registered shares repurchased on the second trading line. By way of illustration only, the repurchase volume of a maximum of USD 4.3 billion, based on the closing price of ABB’s registered shares on 6 April 2021 of CHF 29.25 and a USD/CHF exchange rate of 0.93, corre- sponds to up to 136.7 million registered shares or up to 6.3 % of the current share capital and voting rights of ABB. The share buyback program was exempted from the provisions on public takeover offers provided for in section 6.1 of the Circular no. 1 of the Swiss Takeover Board dated 27 June 2013 (status as of 1 January 2016) and refers to a maximum of 205,314,826 registered shares, equivalent to a maximum of 9.47 % of the share capi- tal currently registered in the commercial register (the share capital currently registered in the commercial regis- ter amounts to CHF 260,177,791.68, divided into 2,168,148,264 registered shares, each with a nominal value of CHF 0.12).