Epidemic Self-Poisoning with Seeds of Cerbera Manghas in Eastern Sri
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Method to Estimate Dry-Kiln Schedules and Species Groupings: Tropical and Temperate Hardwoods
United States Department of Agriculture Method to Estimate Forest Service Forest Dry-Kiln Schedules Products Laboratory Research and Species Groupings Paper FPL–RP–548 Tropical and Temperate Hardwoods William T. Simpson Abstract Contents Dry-kiln schedules have been developed for many wood Page species. However, one problem is that many, especially tropical species, have no recommended schedule. Another Introduction................................................................1 problem in drying tropical species is the lack of a way to Estimation of Kiln Schedules.........................................1 group them when it is impractical to fill a kiln with a single Background .............................................................1 species. This report investigates the possibility of estimating kiln schedules and grouping species for drying using basic Related Research...................................................1 specific gravity as the primary variable for prediction and grouping. In this study, kiln schedules were estimated by Current Kiln Schedules ..........................................1 establishing least squares relationships between schedule Method of Schedule Estimation...................................2 parameters and basic specific gravity. These relationships were then applied to estimate schedules for 3,237 species Estimation of Initial Conditions ..............................2 from Africa, Asia and Oceana, and Latin America. Nine drying groups were established, based on intervals of specific Estimation -

I. Isolation and Characterization of Bioactive Compounds From
I. ISOLATION AND CHARACTERIZATION OF BIOACTIVE COMPOUNDS FROM SURINAME AND MADAGASCAR FLORA. II. A SYNTHETIC APPROACH TO LUCILACTAENE Eba Adou Dissertation submitted to the faculty of the Virginia Polytechnic Institute and State University in partial fulfillment of the requirement for the degree of Doctor of Philosophy In Chemistry Dr. David G. I. Kingston, Chairman Dr. James Tanko Dr. Felicia Etzkorn Dr. Timothy E. Long Dr. Paul Deck November 28, 2005 Blacksburg, Virginia Keywords: Anticancer agents, Cytotoxicity assay, Indole alkaloids, Diterpenoids, Cardenolide glycosides, Physalins, Cucurbitacins, Cell cycle, Cell cycle inhibitor, p53 Tumor suppressor Gene, Lucilactaene Copyright 2005, Eba Adou ISOLATION AND CHARACTERIZATION OF BIOACTIVE COMPOUNDS FROM SURINAME AND MADAGASCAR FLORA AND A SYNTHETIC APPROACH TO LUCILACTAENE ABSTRACT Eba Adou As part of an International Cooperative Biodiversity Group (ICBG), extracts of plants from Suriname and Madagascar were bioassayed for cytotoxicity and antimalarial activity. Six cytotoxic extracts and one potential antimalarial were selected for fractionation, and yielded a number of bioactive compounds which were characterized by spectroscopy methods. Craspidospermum verticillatum (Apocynaceae) yielded four known indole alkoids. Casimirella sp (Icacinaceae) gave three new and five known diterpenoids. Pentopetia androsaemifolia (Apocynaceae) afforded one new and three known cardenolide glycosides. Physalis angulata (Solanaceae) yielded seven known physalins. Roupellina boivinnii (Apocynaceae) yielded four known and three new cardenolide glycosides, and three known cucurbitacins were isolated from Octolepis aff. dioica (Thymelaeaceae). In addition to these structural studies, a synthetic approach to lucilactaene, a cell cycle inhibitor was developed. ACKNOWLEDGMENTS I dedicate this to my family in Côte d’Ivoire (Ivory Coast) for giving me the opportunity to come to the U.S.A. -
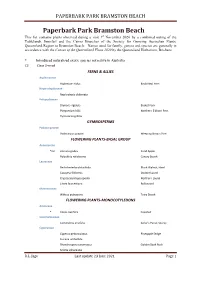
Paperbark Park Bramston Beach
PAPERBARK PARK BRAMSTON BEACH Paperbark Park Bramston Beach This list contains plants observed during a visit 1st November 2020 by a combined outing of the Tablelands, Innisfail and the Cairns Branches of the Society for Growing Australian Plants, Queensland Region to Bramston Beach. Names used for family, genera and species are generally in accordance with the Census of the Queensland Flora 2020 by the Queensland Herbarium, Brisbane. * Introduced naturalised exotic species not native to Australia C3 Class 3 weed FERNS & ALLIES Aspleniaceae Asplenium nidus Birds Nest Fern Nephrolepidaceae Nephrolepis obliterata Polypodiaceae Drynaria rigidula Basket Fern Platycerium hillii Northern Elkhorn Fern Pyrrosia longifolia GYMNOSPERMS Podocarpaceae Podocarpus grayae Weeping Brown Pine FLOWERING PLANTS-BASAL GROUP Annonaceae *C3 Annona glabra Pond Apple Polyalthia nitidissima Canary Beech Lauraceae Beilschmiedia obtusifolia Blush Walnut; Hard Cassytha filiformis Dodder Laurel Cryptocarya hypospodia Northern Laurel Litsea fawcettiana Bollywood Monimiaceae Wilkiea pubescens Tetra Beech FLOWERING PLANTS-MONOCOTYLEDONS Arecaceae * Cocos nucifera Coconut Commelinaceae Commelina ensifolia Sailor's Purse; Scurvy Cyperaceae Cyperus pedunculatus Pineapple Sedge Fuirena umbellata Rhynchospora corymbosa Golden Beak Rush Scleria sphacelata R.L. Jago Last update 23 June 2021 Page 1 PAPERBARK PARK BRAMSTON BEACH Flagellariaceae Flagellaria indica Supplejack Heliconiaceae * Heliconia psittacorum Heliconia Hemerocallidaceae Dianella caerulea var. vannata Blue -

A Case of Attempted Suicide by Cerbera Odollam Seed Ingestion
Hindawi Case Reports in Critical Care Volume 2020, Article ID 7367191, 5 pages https://doi.org/10.1155/2020/7367191 Case Report A Case of Attempted Suicide by Cerbera odollam Seed Ingestion Michelle Bernshteyn , Steven H. Adams, and Kunal Gada SUNY Upstate Medical University, 750 E Adams St., Syracuse, NY 13210, USA Correspondence should be addressed to Michelle Bernshteyn; [email protected] Received 3 March 2020; Revised 2 June 2020; Accepted 4 June 2020; Published 15 June 2020 Academic Editor: Ricardo Jorge Dinis-Oliveira Copyright © 2020 Michelle Bernshteyn et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We report a case of attempted suicide by Cerbera odollam seed ingestion by a transgender patient who was successfully treated at our hospital. While the C. odollam plant has multiple practical and ornamental functions, its seeds have traditionally been utilized for suicidal and homicidal purposes in many parts of the world. Physicians should be aware of the presentation, diagnosis, and treatment of C. odollam ingestion given the current ease of availability of these seeds in the United States and the increased reports of suicide attempts. 1. Introduction with a junctional rhythm and therefore received a total of 10 vials of Digibind (digoxin immune fab). She denied any head- Indigenous to India and Southeast Asia, Cerbera odollam, ache, visual disturbances, chest pain, palpitations, shortness “ ” also known as pong-pong, or suicide tree, yields highly car- of breath, abdominal tenderness, diarrhea, or constipation. -

Phytochemical Analysis, Antioxidant Assay and Antimicrobial Activity in Leaf Extracts of Cerbera Odollam Gaertn
Pharmacogn J. 2018; 10(2): 285-292 A Multifaceted Journal in the field of Natural Products and Pharmacognosy Original Article www.phcogj.com | www.journalonweb.com/pj | www.phcog.net Phytochemical Analysis, Antioxidant Assay and Antimicrobial Activity in Leaf Extracts of Cerbera odollam Gaertn Abinash Sahoo, Thankamani Marar* ABSTRACT Introduction: In the current study, methanol and aqueous extracts of leaf of Cerbera odollam Gaertn were screened for its antibacterial, antifungal, phytochemicals and antioxidant ac- tivities. Phytochemical constituents were investigated both qualitatively and quantitatively. Methods: The leaf extracts of Cerbera odollam Gaertn were prepared by drying and extracted using Soxhlet apparatus into methanol and aqueous media, which were subjected to phyto- chemical screening. Total phenols, tannins, flavanols, alkaloids and its antioxidant activity were determined using spectroscopic techniques. Antimicrobial activity were determined using well diffusion method. Results: Aqueous extract exhibits higher content of phenols, tannins, flavanols and alkaloids, whereas methanol extract exhibits higher content of anthocyanin and cardiac glycoside respectively. Aqueous extract exhibits higher inhibitory concentration (IC %) value for DPPH (2, 2-Diphenyl-1-picrylhydrazyl) and H2O2 radical scavenging assay and reduc- ing power (RP) assay. The methanol extracts exhibited higher inhibitory concentration (IC %) value in SO and NO radical scavenging assay, exhibiting antioxidant properties in five antioxi- dant models that were investigated. The methanol extract showed some antibacterial activity against Bacillus subtilis, Staphylococcus aureus, Salmonella typhi and Escherichia coli with inhibitory zone ranging from 2 mm to 3 mm, whereas the aqueous extract showed no activity. Abinash Sahoo, High antifungal activity was found against Saccharomyces cerevisiae and Candida albicans for methanol extract and moderate for aqueous extract with inhibitory zone ranging from 9mm Thankamani Marar* to 26 mm. -

JNMA (142) Final
CASE REPORT Journal of Nepal Medical Association, 2002:41:331-334 Yellow oleander poisoning : a case report 1 1 1 Mollah A H , Ahmed S , Haque N 1 1 2 3 Shamsuzzaman , Islam A K M N , Rashid A , Rahim M INTRODUCTION CASE SUMMARY Because of its beautiful flowers, people plant yellow A 7 years old school boy was admitted on 15th June oleander tree in their garden & compound as a 2001 with a history of ingestion of a fruit along with hobby without knowing it's poisonous action. The its seeds from a yellow oleander tree in the premises entire plant is toxic including smoke from the of his school as he thought it was a water chestnut burning foliage and even the water in which the (there is a structural similarity between water flower have been placed.1,2 Yellow oleander has chestnut & yellow oleander fruit). About 20 minutes been used for the purpose of suicide, homicide and following ingestion, he started vomiting & became as an abortifaecient3 and if anybody ingests any restless. Subsequently he became drowsy, lethargic part of it accidentally, this may apprehend a fatal & had froth from his mouth and passed loose stool outcome4,5 and even the fetus can be affected if the unconsciously. On examination, the child was found pregnant mother ingests it.6 Recently a 7 years old mildly dehydrated with cold & calmly extremities. boy was admitted into pediatric ward of Dhaka His pulse rate was 54/min, low volume & irregular. Medical College Hospital (DMCH) in a serious Blood pressure was 60/20 mm Hg. -

Chemical Constituents from the Seeds of Cerbera Manghas 1
Part I Chemical Constituents from the Seeds of Cerbera manghas 1 CHAPTER 1.1 INTRODUCTION 1.1.1 Introduction Cerbera manghas Linn., a mangrove plant belonging to the Apocynaceae family, is distributed widely in the coastal areas of Southeast Asia and countries surrounding the Indian Ocean. The Apocynaceae family contains about 155 genus and 1700 species. In Thailand only 42 genus and 125 species are found, from Cerbera genera only 2 species are found, C. manghas and C. odollam (The Forest Herbarium, Royal Forest Department, 1999). C. manghas was found in Prachuap Khiri Khan, Chonburi, Rayong, Phuket, Songkhla, Satun and Narathiwat while C. odollam was found in Bangkok, Ranong, Surat Thani, Phangga, Krabi, Satun and Narathiwat Cerbera manghas is a small tree, 4 - 6 m tall, stem soft, glabrous with milky juice, leaves alternate, closely set or whorled at the apices of branchlets, 10 -15 x 3 - 5 cm, ovate-oblong or oblaceolate, acuminate at apex, rounded at base, flowers large, bracteate, 3 - 4 cm long, arranged in terminal paniculate cyme, funnel shaped, white with yellow throat, turning purple or red on ageing, fruit large, 7 - 9 x 4 - 6 cm, globose, ovoid or ellipsoid, drupaceous with fibrous pericarp, seeds 1 -2 , each 2 - 2.5 cm across, broad, compressed, fibrous. 1 2 Figure 1 Cerbera manghas (Apocynaceae) 3 1.1.2 Review of literatures Plants in the Cerbera genus (Apocynaceae) are well known to be rich in a variety of compounds: cardenolide glycosides (Abe, et.al., 1977; Yamauchi, 1987); lignan (Abe, et.al., 1988; 1989); iridoid monoterpenes (Abe, et.al., 1977; Yamauchi, et.al.,1990) normonoterpene glycosides (Abe, et.al., 1988; 1996) and dinormonoterpeniod glycosides (Abe, et.al., 1996) etc. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

Insecticidal and Cytotoxic Agents of Thevetia Thevetioides Seed
Purchased by U. S. Dept. 01 AgrlcultlUe for Official Use Neriifolin and 2' -Acetylneriifolin: Insecticidal and Cytotoxic Agents of 1 Thevetia thevetioides Seeds ,2 J. L. McLAUGHLIN, B. FREEDMAN, R. G. POWELL, AND C. R. SMITH, JR. Northern Regional Research Center, Agric. Res., SEA, USDA, Peoria, IL 61604 Reprillted from the JOURNAL OF ECONOMIC ENTOMOLOGY Neriifolin and 2' -Acetylneriifolin: Insecticidal and Cytotoxic Agents of 1 Thevetia thevetioides Seeds ,2 J. L. McLAUGHLIN, B. FREEDMAN, R. G. POWELL, AND C. R. SMITH, JR. Northern Regional Research Center, Agric. Res., SEA, USDA, Peoria, IL 61604 ABSTRACT J. Ecan. Enlama!. 73: 398-402 (1980) A bioassay procedure utilizing the European com borer, Ostrinia nubilalis (Hiibner), has been used to guide the phytochemical fractionation of active extracts of the seeds of a yellow oleander, Thevetia thevetioides (HBK.) K. Schum. (Apocynaceae). The known cardiotonic glycosides, neriifolin and 2'-acetylneriifolin, were crystallized as the active insecticidal agents, giving LDso determinations of 30 ppm and 192 ppm, respectively, when incorporated into the com borer diet. These compounds also exhibited cytotoxic activities of 2.2x 10-2 and 3.3 x 10-2 fLg/ml, respectively, in the KB (human nasopharynx epidermoid carcinoma) in vitro system. The glucoside of f3-sitosterol also was isolated but it lacked insecticidal activity. Freedman et al. (1979) reported that ethanol extracts Materials and Methods of the seeds of a Mexican yellow oleander, Thevetia Plant Material thevetioides (HBK.) K. Schum. (Apocynaceae) were lethal (100% larval mortality) when incorporated into Seeds of T. thevetioides were collected in September the diet of the European com borer, Ostrinia nubilalis 1977 in Mexico for the USDA Medicinal Plant Re (Hiibner). -

Cerberiopsis Candelabrum Vieill
ADANSONIA,ser. 2, 11 (4) 1971. UNE APOCYNACÉE MONOCARPIQUE DE NOUVELLE-CALÉDONIE CERBERIOPSIS CANDELABRUM VIEILL. par J. M. VEILLON~ RBSUMÉ: Chez les Dicotylédones, les espèces arborescentes monocarpiques jusqu'à présent connues sont peu nombreuses et dans la quasi-totalité des cas, ce sont des espèces monocaules, leur croissance étant conditionnée par le fonctionnement d'un seul méristème apical dont la différenciation en inflorescence terminale entraîne la mort de la plante. P. SARLIN(1954) a signalé pour la première fois le caractère monocarpique chez l'Apocynacée arborescente : Cerberiopsis candelabrum Vieill.. espèce possédant un nombre élevé mais limité de méristèmes latéraux dont le fonctionnement a pour effet d'engendrer de nombreuses ramifications. Dans cette note, nous présentons quelques données nouvelles relatives 2 l'archi- tecture et à la monocarpie de cette espèce remarquable. SUMMARY:The few monocarpic arborescent dicotyledons already known are almost all monocaul species, their growth being conditioned by the activity of a single apical meristem whose differentiation into a terminal inflorescence leads to the death of the plant. Monocarpy in the tree Cevberiopsis candelabrum Vieill,, was first reported by SARLIN(1954). The species has a large but limited number of lateral meristems whose activity produces numerous branches. We present in this note some recent data concerning the architecture and the mono- carpy of this remarkable species. On sait que la flore néo-calédonienne est particulièrement riche en espèces ayant des formes architecturales ou des biologies très originales. Une des plus remarquables est Cerberiopsis candelabrum Vieill., Apocynacée arborescente dont le caractère monocarpique a été signalé pour la première fois par P. -

An Unusual Case of Cardiac Glycoside Toxicity
International Journal of Cardiology 170 (2014) 434–444 Contents lists available at ScienceDirect International Journal of Cardiology journal homepage: www.elsevier.com/locate/ijcard Letters to the Editor An unusual case of cardiac glycoside toxicity David Kassop a,⁎,1, Michael S. Donovan a,1, Brian M. Cohee b,1, Donovan L. Mabe c,1, Erich F. Wedam a,1, John E. Atwood a,1 a Cardiovascular Disease Service, Department of Medicine, Walter Reed National Military Medical Center, Bethesda, MD, United States b Pulmonary Disease and Critical Care Service, Department of Medicine, Walter Reed National Military Medical Center, Bethesda, MD, United States c Internal Medicine Service, Department of Medicine, Walter Reed National Military Medical Center, Bethesda, MD, United States article info Her heart rate was 30 beats per minute (bpm) and blood pressure 90/60 mm Hg. An electrocardiogram (ECG) demonstrated atrial Article history: flutter(AFl) with variable atrioventricular (AV) block and slow Received 10 September 2013 ventricular response, diffuse ST-segment depressions, shortened QT Accepted 2 November 2013 interval, and peaked T-waves (Fig. 1A). Laboratory studies were Available online 13 November 2013 significant for a serum potassium level of 7.5 mmol/L (normal: 3.5–5.1), Keywords: calcium of 10.9 mg/dL (normal 8.6–10.2), and creatinine of 2.6 mg/dL Cardiac glycoside toxicity (normal: 0.7–1.2). Cardiac enzymes were mildly elevated with a troponin Cerbera odollam T level of 0.07 ng/mL (normal: b0.03). Comprehensive serum and urine Pong-pong Poisoning toxicology screens were unremarkable. A digoxin concentration level was Dysrhythmia undetectable (b0.3 ng/mL). -

Oleander and Datura Poisoning: an Update Vijay V Pillay1, Anu Sasidharan2
INVITED ARTICLE Oleander and Datura Poisoning: An Update Vijay V Pillay1, Anu Sasidharan2 ABSTRACT India has a very high incidence of poisoning. While most cases are due to chemicals or drugs or envenomation by venomous creatures, a significant proportion also results from consumption or exposure to toxic plants or plant parts or products. The exact nature of plant poisoning varies from region to region, but certain plants are almost ubiquitous in distribution, and among these, Oleander and Datura are the prime examples. These plants are commonly encountered in almost all parts of India. While one is a wild shrub (Datura) that proliferates in the countryside and by roadsides, and the other (Oleander) is a garden plant that features in many homes. Incidents of poisoning from these plants are therefore not uncommon and may be the result of accidental exposure or deliberate, suicidal ingestion of the toxic parts. An attempt has been made to review the management principles with regard to toxicity of these plants and survey the literature in order to highlight current concepts in the treatment of poisoning resulting from both plants. Keywords: Cerbera, Datura, Nerium, Oleander, Plant poison, Thevetia. Indian Journal of Critical Care Medicine (2019): 10.5005/jp-journals-10071-23302 INTRODUCTION 1Department of Forensic Medicine and Toxicology, Poison Control India being a tropical country is host to a rich and varied Centre, Amrita School of Medicine, Amrita Vishwa Vidyapeetham, flora encompassing thousands of plants; and while most are Kochi, Kerala, India nonpoisonous, a significant few possess toxic properties of varying 2Department of Forensic Medicine and Toxicology, Forensic Pathology degree.