ELSO Bibliography Problems in the Extracorporeal Membrane Oxygenation (ECMO). Nippon Kyobu Geka Gakkai Zasshi 1978 March;26(3):2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CA Students Urge Assembly Members to Pass AB
May 26, 2021 The Honorable Members of the California State Assembly State Capitol Sacramento, CA 95814 RE: Thousands of CA Public School Students Strongly Urge Support for AB 101 Dear Members of the Assembly, We are a coalition of California high school and college students known as Teach Our History California. Made up of the youth organizations Diversify Our Narrative and GENup, we represent 10,000 youth leaders from across the State fighting for change. Our mission is to ensure that students across California high schools have meaningful opportunities to engage with the vast, diverse, and rich histories of people of color; and thus, we are in deep support of AB101 which will require high schools to provide ethnic studies starting in academic year 2025-26 and students to take at least one semester of an A-G approved ethnic studies course to graduate starting in 2029-30. Our original petition made in support of AB331, linked here, was signed by over 26,000 CA students and adult allies in support of passing Ethnic Studies. Please see appended to this letter our letter in support of AB331, which lists the names of all our original petition supporters. We know AB101 has the capacity to have an immense positive impact on student education, but also on student lives as a whole. For many students, our communities continue to be systematically excluded from narratives presented to us in our classrooms. By passing AB101, we can change the precedent of exclusion and allow millions of students to learn the histories of their peoples. -

Revision Tracheobronchoplasty: Case Report
4 Case Report Page 1 of 4 Revision tracheobronchoplasty: case report Ammara A. Watkins, Jennifer L. Wilson, Mihir Parikh, Adnan Majid, Sidhu P. Gangadharan Division of Thoracic Surgery and Interventional Pulmonology, Beth Israel Deaconess, Harvard Medical School, Boston, MA, USA Correspondence to: Sidhu P. Gangadharan, MD. Chief, Division of Thoracic Surgery and Interventional Pulmonology, Beth Israel Deaconess Medical Center, 185 Pilgrim Rd. W/DC 201 Boston, MA 02215, USA. Email: [email protected]. Abstract: Tracheobronchoplasty, or posterior splinting of the airway with mesh, is a durable solution for patients with severe tracheobronchomalacia (TBM). Recurrent symptoms of TBM following tracheobronchoplasty are uncommon; however, when they occur can have significant impact on quality of life. Appropriate management of recurrent TBM requires a systematic and multidisciplinary collaborative approach. We present a patient with postoperative symptom recurrence requiring revisional tracheobronchoplasty to highlight the complexity of the disease’s presentation, workup and treatment. Keywords: Reoperative; revision; tracheobronchoplasty; tracheobronchomalacia (TBM); case report Received: 06 October 2019; Accepted: 18 December 2019; Published: 25 November 2020. doi: 10.21037/ccts.2019.12.14 View this article at: http://dx.doi.org/10.21037/ccts.2019.12.14 Introduction her tracheobronchoplasty she reported recurrent wheezing, cough and shortness of breath. By four years following Tracheobronchomalacia is an increasingly recognized her operation, the progressive symptoms considerably abnormality of the central airway that can cause dyspnea, impacted her quality of life. She was unable to walk 2 cough, recurrent respiratory infections and respiratory blocks without shortness of breath and had been admitted insufficiency (1,2). The hallmark of the disease is expiratory at least six times in the past year due to respiratory distress. -

Detection and Diagnosis of Large Airway Collapse: a Systematic Review
Early View Review Detection and diagnosis of large airway collapse: a systematic review Alexandros Mitropoulos, Woo-Jung Song, Fatma Almaghlouth, Samuel Kemp, Michael Polkey, James Hull Please cite this article as: Mitropoulos A, Song W-J, Almaghlouth F, et al. Detection and diagnosis of large airway collapse: a systematic review. ERJ Open Res 2021; in press (https://doi.org/10.1183/23120541.00055-2021). This manuscript has recently been accepted for publication in the ERJ Open Research. It is published here in its accepted form prior to copyediting and typesetting by our production team. After these production processes are complete and the authors have approved the resulting proofs, the article will move to the latest issue of the ERJOR online. Copyright ©The authors 2021. This version is distributed under the terms of the Creative Commons Attribution Non-Commercial Licence 4.0. For commercial reproduction rights and permissions contact [email protected] DETECTION AND DIAGNOSIS OF LARGE AIRWAY COLLAPSE: A SYSTEMATIC REVIEW Mitropoulos Alexandros1, Song Woo-Jung3, Almaghlouth Fatma2, Kemp Samuel1,2, Polkey I Michael1,2, Hull H James1,2 1Department of Respiratory Medicine, Royal Brompton Hospital, London, UK. 2National Heart and Lung Institute, Imperial College, London, UK. 3Department of Allergy and Clinical Immunology, Asan Medical Centre, University of Ulsan College of Medicine, Seoul, Korea Corresponding author: Dr James H Hull FRCP PhD Department of Respiratory Medicine, Royal Brompton Hospital London, SW3 6HP E-mail: [email protected] -

Urzędu Patentowego
URZĄD PATENTOWY RZECZYPOSPOLITEJ POLSKIEJ BIULETYN Urzędu Patentowego Wynalazki i Wzory użytkowe ISSN - 2543 - 5779 • Cena 10,50 zł (w tym 5% VAT) • Warszawa 2017 4 UUrządrząd PPatentowyatentowy RPRP – nana ppodstawieodstawie art.art. 4343 ust.ust. 1,1, art.art. 100100 orazoraz art.art. 2332331 uustawystawy z ddniania 3300 cczerwcazerwca 22000000 rr.. PPraworawo wwłasnościłasności przemysłowejprzemysłowej (Dz.(Dz. U.U. z 20132013 r.r. poz.poz. 14101410 z późniejszymipóźniejszymi zzmianami)mianami) oorazraz rrozporządzeniaozporządzenia PPrezesarezesa RRadyady MMinistrówinistrów wwydanegoydanego nnaa ppodstawieodstawie aart.rt. 9933 oorazraz aart.rt. 110101 uust.st. 2 ppowołanejowołanej ustawyustawy – dokonujedokonuje ogłoszeniaogłoszenia w „„BiuletynieBiuletynie UUrzędurzędu PPatentowego”atentowego” o zzgłoszonychgłoszonych wwynalazkach,ynalazkach, wwzorachzorach uużytkowych.żytkowych. OOgłoszeniagłoszenia o zzgłoszeniachgłoszeniach wwynalazkówynalazków i wwzorówzorów uużytkowychżytkowych ppublikowaneublikowane w BiuletynieBiuletynie ppodaneodane ssąą w uukła-kła- ddziezie klasowymklasowym wedługwedług MiędzynarodowejMiędzynarodowej KlasyfiKlasyfi kacjikacji PatentowejPatentowej i zawierają:zawierają: – ssymbolymbol MiędzynarodowejMiędzynarodowej KKlasyfilasyfi kkacjiacji PPatentowej,atentowej, – nnumerumer zgłoszeniazgłoszenia wwynalazkuynalazku llubub wwzoruzoru uużytkowego,żytkowego, – ddatęatę zzgłoszeniagłoszenia wwynalazkuynalazku llubub wwzoruzoru uużytkowego,żytkowego, – datędatę i kkrajraj uuprzedniegoprzedniego ppierwszeństwaierwszeństwa -

Ebooksspringer Contrat 4903.07.Xls Title Editors/Authors Year Book ISBN13 Book E-ISBN13 the Abcs of Gene Cloning Wong, Dominic W
EbooksSpringer_contrat_4903.07.xls Title Editors/Authors Year Book ISBN13 Book e-ISBN13 The ABCs of Gene Cloning Wong, Dominic W.S. 2006 978-0-387-28663-1 978-0-387-28679-2 Abductive Reasoning Aliseda, Atocha 2006 978-1-4020-3906-5 978-1-4020-3907-2 Abeta Peptide and Alzheimer's Disease Barrow, Colin J; Small, David H. 2007 978-1-85233-961-6 978-1-84628-440-3 Abiotic Stress Tolerance in Plants Rai, Ashwani K.; Takabe, Teruhiro 2006 978-1-4020-4388-8 978-1-4020-4389-5 Abnormal Skeletal Phenotypes Castriota-Scanderbeg, Alessandro; 2005 978-3-540-67997-4 978-3-540-30361-9 Dallapiccola, Bruno Abord clinique des malades de l'alcool Huas, Dominique; Rueff, Bernard 2005 978-2-287-59769-5 978-2-287-28577-6 Abord clinique des urgences traumatiques au cabinet Carolet, Carole; Pire, Jean-Claude 2005 978-2-287-25170-2 978-2-287-28164-8 du généraliste Abord clinique du malade âgé Moulias, Robert 2007 978-2-287-22084-5 978-2-287-31016-4 Abord clinique en urologie Cortesse, Alain; LeDuc, Alain 2006 978-2-287-25253-2 978-2-287-48614-2 About Life Agutter, Paul S.; Wheatley, Denys N. 2007 978-1-4020-5417-4 978-1-4020-5418-1 Abstract Algebra Grillet, Pierre Antoine 2007 978-0-387-71567-4 978-0-387-71568-1 Abstract Computing Machines Kluge, W. 2005 978-3-540-21146-4 978-3-540-27359-2 Abstract Harmonic Analysis of Continuous Wavelet Führ, Hartmut 2005 978-3-540-24259-8 978-3-540-31552-0 Transforms Abstraction Refinement for Large Scale Model Hachtel, Gary D.; Somenzi, Fabio; Wang, 2006 978-0-387-34155-2 978-0-387-34600-7 Abstraction,Checking Refinement and Proof for Probabilistic McIver,Chao Annabelle; Morgan, Charles C. -

Surgery for Lung Cancer and Malignant Pleural Mesothelioma
Surgery for Lung Cancer and Malignant Pleural Mesothelioma Mir Alireza Hoda, MD PhD Associate Professor for Surgery Clinical Director Surgical Thoracic Oncology Program & Translational Thoracic Oncology Laboratory Division of Thoracic Surgery Department of Surgery Comprehensive Cancer Center Medical University of Vienna 5th ESO-ESMO Eastern Europe and Balkan Region Masterclass in Medical Oncology – Session LUNG CANCER AND MESOTHELIOMA Current affiliation West German Lung Center & West German Cancer Center Department of Thoracic Surgery and Thoracic Endoscopy (Director: Prof. Dr. Clemens Aigner) Disclosure . I have no, real or perceived, direct or indirect conflicts of interest that relate to this presentation. Summary provided in: ESMO Thoracic Tumors: Essentials for Clinicians Chapter 5 Hoda & Klepetko available at Oncology PRO or by...... [email protected] [email protected] Surgery for lung cancer AGENDA Overview Surgery for early stage NSCLC Surgery for locally advanced disease Surgery for oligometastatic disease Palliative treatment options Role of surgery in SCLC Summary Male Female Lung Cancer Mortality since 1930 Classical treatment protocol for Lung cancer Stage TNM IA T1N0M0 IB T2N0M0 IIA Surgery T1N1M0 IIB T2N1M0 T3N0M0 IIIA T1-3N2M0 T3N1M0 Chemo/Radio IIIB T1-3N3M0 T4anyNM0 Modern Treatment Algorithm for Lung cancer Stage IA IB IIA IIB Surgery Adjuvant Chemotherapy IIIA1-2 IIIA3 neoadjuvant Radiotherapy + Second-line treatment Responders Chemotherapy IIIA4 - B - Responders IV Non Surgery for early stage NSCLC Standard of care: Lobectomy + mediastinal lymph node dissection (MLND) Standard of care – new developments • Minimal invasive resesctions (incl.awake) • Sublobar resection (limited resections) • Parenchyma sparing options Minimal invasive surgery (MIS) Video assisted thoracic surgery (VATS) VATS: uniportal (Gonzalez-Rivas et al, 2013) VATS: 3-portal (Hansen et al, 2011) Robotic assisted thoracic surgery (RATS) Awake VATS for SPN RCT n=60 Epidural anaesthesia vs GA+DLI 0% mortality Pompeo et al, ATS 2004 Lobectomy: MIS vs. -

Inside Surgery
HOME << | >> NOVEMBER / DECEMBER News from the Roberta and Stephen R. Weiner Department of Surgery 2011 at Beth Israel Deaconess Medical Center Volume 1, No. 2 THIS NEWSLETTER IS INTERACTIVE The table of contents, web addresses, and e-mail addresses in this newsletter are interactive. INSIDE SURGERY IN THis issUE Research Scholarship Honors Douglas Hanto, MD, PhD 1 Scholarship Honors Douglas Hanto, MD, PhD ed Boylan’s first encounter with BIDMC was unequivocally 2 New Leadership Structure T positive — 24 years ago, his third 3 Richard Whyte, MD, Assumes child and only daughter, Carolina New Vice Chair Position (“Nina”), was born at the hospital. Quality Team Grows The Concord resident’s recent 4 In Memoriam experiences at the hospital have, “Looking Back” — Photos from unfortunately, been considerably Our Archives less so. Last year, Nina was 5 “The Question I Own” — diagnosed with advanced liver Wolfgang Junger, PhD cancer at BIDMC, and began a 6 Research Notes long and arduous journey that Save the Date continues to this day. 7 “Alumni Spotlight” — Transplant Following her diagnosis, Surgeon Amy Evenson, MD Nina’s only chance at beating her Douglas Hanto, MD, PhD, Chief of Transplantation 8 News Briefs cancer was the surgical removal of a large liver tumor, which Douglas 10 Urology’s Mission to Cape Verde Hanto, MD, PhD, Chief of the Division of Transplantation, performed in January 11 Sidhu Gangadharan, MD, 2011. Nina fared very well until, four months later, follow-up tests revealed that the Named Division Chief cancer had spread. After three months of chemotherapy this summer, Nina underwent New Faculty: Erik Folch, MD a second operation in late September to remove tumors in her lungs and abdomen. -
Adams Adkinson Aeschlimann Aisslinger Akkermann
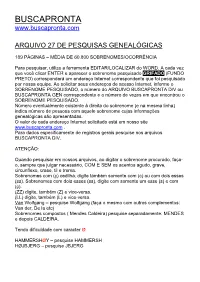
BUSCAPRONTA www.buscapronta.com ARQUIVO 27 DE PESQUISAS GENEALÓGICAS 189 PÁGINAS – MÉDIA DE 60.800 SOBRENOMES/OCORRÊNCIA Para pesquisar, utilize a ferramenta EDITAR/LOCALIZAR do WORD. A cada vez que você clicar ENTER e aparecer o sobrenome pesquisado GRIFADO (FUNDO PRETO) corresponderá um endereço Internet correspondente que foi pesquisado por nossa equipe. Ao solicitar seus endereços de acesso Internet, informe o SOBRENOME PESQUISADO, o número do ARQUIVO BUSCAPRONTA DIV ou BUSCAPRONTA GEN correspondente e o número de vezes em que encontrou o SOBRENOME PESQUISADO. Número eventualmente existente à direita do sobrenome (e na mesma linha) indica número de pessoas com aquele sobrenome cujas informações genealógicas são apresentadas. O valor de cada endereço Internet solicitado está em nosso site www.buscapronta.com . Para dados especificamente de registros gerais pesquise nos arquivos BUSCAPRONTA DIV. ATENÇÃO: Quando pesquisar em nossos arquivos, ao digitar o sobrenome procurado, faça- o, sempre que julgar necessário, COM E SEM os acentos agudo, grave, circunflexo, crase, til e trema. Sobrenomes com (ç) cedilha, digite também somente com (c) ou com dois esses (ss). Sobrenomes com dois esses (ss), digite com somente um esse (s) e com (ç). (ZZ) digite, também (Z) e vice-versa. (LL) digite, também (L) e vice-versa. Van Wolfgang – pesquise Wolfgang (faça o mesmo com outros complementos: Van der, De la etc) Sobrenomes compostos ( Mendes Caldeira) pesquise separadamente: MENDES e depois CALDEIRA. Tendo dificuldade com caracter Ø HAMMERSHØY – pesquise HAMMERSH HØJBJERG – pesquise JBJERG BUSCAPRONTA não reproduz dados genealógicos das pessoas, sendo necessário acessar os documentos Internet correspondentes para obter tais dados e informações. DESEJAMOS PLENO SUCESSO EM SUA PESQUISA. -

Rigid Laryngoscopy, Oesophagoscopy and Bronchoscopy in Adults
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY RIGID LARYNGOSCOPY, OESOPHAGOSCOPY & BRONCHOSCOPY IN ADULTS Johan Fagan, Mark De Groot Adult bronchoscopy, rigid oesophagoscopy teeth (Figure 3). Ask a dentist to make a and laryngoscopy for both diagnostic and customised guard for patients with therapeutic reasons are generally done abnormal teeth (Figure 4) or fashion one in under general anaesthesia. Panendoscopy the operating room from thermoplastic (all 3 procedures) is commonly performed sheeting (Figures 5a, b). to rule out synchronous primaries with squamous cell cancer of the upper aerodi- gestive tract. This chapter covers the tech- niques, pitfalls and safety measures of these 3 procedures. Morbidity of rigid endoscopy Sharing the airway with an anaesthetist requires close communication and a good understanding between surgeon and anaes- thetist. Figure 1: Protecting the lips with the fingers of the non-dominant hand It is surprising how often rigid endoscopy causes minor extralaryngeal and extra- oesophageal trauma. It is extremely easy to tear or perforate the delicate tissues that line the upper aerodigestive tract; this can lead to deep cervical sepsis, mediastinitis and death. Consequently it is important that a surgeon exercises extreme caution and knows when to abandon e.g. a difficult oesophagoscopy procedure. Mucosal injury occurs in up to 75% of cases and commonly involves the lips or Figure 2: Endoscopes exert excessive 1 angles of the mouth . To protect especially lateral pressure on the teeth to either side the lower lip one should advance the scope of a gap between the front teeth over the fingers of the non-dominant hand (Figure 1). -

The Prevalence of Tracheobronchomalacia in Patients
The Internet Journal of Pulmonary Medicine ISPUB.COM Volume 12 Number 1 The Prevalence of Tracheobronchomalacia in Patients with Asthma or Chronic Obstructive Pulmonary Disease R Patel, L Irugulapati, V Patel, A Esan, C Lapidus, J Weingarten, A Saleh, A Sung Citation R Patel, L Irugulapati, V Patel, A Esan, C Lapidus, J Weingarten, A Saleh, A Sung. The Prevalence of Tracheobronchomalacia in Patients with Asthma or Chronic Obstructive Pulmonary Disease. The Internet Journal of Pulmonary Medicine. 2009 Volume 12 Number 1. Abstract Background and Objective:Tracheobronchomalacia (TBM) is an under-diagnosed condition presenting with nonspecific symptoms. Patients are often diagnosed with “ difficult to treat” asthma or chronic obstructive pulmonary disease (COPD), especially in a community setting. Prevalence studies showing wide ranges have been based on selective populations. Computed tomography (CT) is a useful non-invasive test that can detect excessive collapse of the central airways. This study aims to determine the prevalence of TBM with compatible features incidentally noted on CT in patients hospitalized for asthma or COPD in a community setting. Methods:A retrospective analysis of CT scans of the chest in patients with a diagnosis of asthma or COPD from January 1, 2007 to December 31, 2007 was conducted. Images were assessed for excessive collapse of central airways between the thoracic inlet and carina. We defined a 50% reduction in the airway lumen diameter as criteria to diagnose TBM. Results:638 patients with a clinical diagnosis of asthma or COPD were admitted during the study period. Twenty-five patients (8.8%) met the criteria for TBM. The prevalence of TBM between the two groups was not statistically different. -

Robotic-Assisted Tracheobronchial Surgery
6178 Review Article on Airway Surgery Robotic-assisted tracheobronchial surgery Brian D. Cohen1, M. Blair Marshall2 1General Surgery Residency Program, MedStar Georgetown/Washington Hospital Center, Washington DC, USA; 2Division of Thoracic Surgery, Brigham and Women’s Hospital, Faculty, Harvard Medical School, Boston, MA, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: None; (III) Provision of study materials or patients: MB Marshall; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Brian D. Cohen, MD. General Surgery Residency Program, MedStar Georgetown/Washington Hospital Center, Washington DC, USA. Email: [email protected]; M. Blair Marshall, MD. Associate Chief for Quality and Safety, Division of Thoracic Surgery, Brigham and Women’s Hospital, Faculty, Harvard Medical School, Boston, MA, USA. Email: [email protected]. Abstract: Robotic technology is positioned to transform the approach to tracheobronchial surgery. With its magnified 3D view, intuitive controls, wristed-instruments, high-fidelity simulation platforms, and the steady implementation of new technical improvement, the robot is well-suited to manage the careful dissection and delicate handling of the airway in tracheobronchial surgery. This innovative technology has the potential to promote the widespread adoption of minimally invasive techniques for this complex thoracic surgery. Keywords: Robotic surgery; thoracic surgery; sleeve lobectomy; sleeve resection; bronchoplasty Submitted Nov 12, 2019. Accepted for publication Feb 19, 2020. doi: 10.21037/jtd.2020.03.05 View this article at: http://dx.doi.org/10.21037/jtd.2020.03.05 Introduction simultaneously being developed. -

Training Guidelines for Advanced Bronchoscopic Procedures Endorsed Version: February 2012
The Thoracic Society of Australia and New Zealand Ltd Training guidelines for advanced Bronchoscopic procedures Endorsed Version: February 2012 Contributing TSANZ Interventional Pulmonology SIG Members: Dr David Fielding Brisbane Dr Martin Phillips Perth Dr Peter Robinson Adelaide Dr Lou Irving Melbourne Dr Luke Garske Brisbane Dr Peter Hopkins Brisbane Abbreviations EBUS Endobronchial ultrasound TBNA Transbronchial needle aspiration Summary These guidelines for Thoracic Medicine advanced procedural training encourage fulfilment of a range of parameters, not just accumulating an empiric number of cases. These include: Empiric numbers as a starting point. The importance of a teacher-student relationship. The trainee has to achieve competence in the procedure as certified by an accredited trainer. As a guide it usually takes about 20 cases to have achieved the appropriate skill level, however that can vary as judged by the expert trainer. Attainment of modest procedural outcome measures during training and in ongoing clinical practice. Attendance at dedicated procedural conferences and fulfilment of modest presentation and/or publication goals. Completion of simulated training, preferably before commencing procedures in patients. Ultimately, when it becomes available, a “pass” on a universally accepted objective assessment tool. In the absence of this last parameter, we can at least insist that trainees undertake simulated training, and that such training itself has an objective assessment. In time such an assessment could become