B0223.Pdf (1.275Mb)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lakshadweep Action Plan on Climate Change 2012 2012 333333333333333333333333
Lakshadweep Action Plan on Climate Change 2012 2012 333333333333333333333333 LAKSHADWEEP ACTION PLAN ON CLIMATE CHANGE (LAPCC) UNION TERRITORY OF LAKSHADWEEP i SUPPORTED BY UNDP Lakshadweep Action Plan on Climate Change 2012 LAKSHADWEEP ACTION PLAN ON CLIMATE CHANGE (LAPCC) Department of Environment and Forestry Union Territory of Lakshadweep Supported by UNDP ii Lakshadweep Action Plan on Climate Change 2012 Foreword 2012 Climate Change (LAPCC) iii Lakshadweep Action Plan on Lakshadweep Action Plan on Climate Change 2012 Acknowledgements 2012 Climate Change (LAPCC) iv Lakshadweep Action Plan on Lakshadweep Action Plan on Climate Change 2012 CONTENTS FOREWORD .......................................................................................................................................... III ACKNOWLEDGEMENTS .................................................................................................................... IV EXECUTIVE SUMMARY .................................................................................................................. XIII PART A: CLIMATE PROFILE .............................................................................................................. 1 1 LAKSHADWEEP - AN OVERVIEW ............................................................................................. 2 1.1 Development Issues and Priorities .............................................................................................................................. 3 1.2 Baseline Scenario of Lakshadweep ............................................................................................................................ -

Islands, Coral Reefs, Mangroves & Wetlands In
Report of the Task Force on ISLANDS, CORAL REEFS, MANGROVES & WETLANDS IN ENVIRONMENT & FORESTS For the Eleventh Five Year Plan 2007-2012 Government of India PLANNING COMMISSION New Delhi (March, 2007) Report of the Task Force on ISLANDS, CORAL REEFS, MANGROVES & WETLANDS IN ENVIRONMENT & FORESTS For the Eleventh Five Year Plan (2007-2012) CONTENTS Constitution order for Task Force on Islands, Corals, Mangroves and Wetlands 1-6 Chapter 1: Islands 5-24 1.1 Andaman & Nicobar Islands 5-17 1.2 Lakshwadeep Islands 18-24 Chapter 2: Coral reefs 25-50 Chapter 3: Mangroves 51-73 Chapter 4: Wetlands 73-87 Chapter 5: Recommendations 86-93 Chapter 6: References 92-103 M-13033/1/2006-E&F Planning Commission (Environment & Forests Unit) Yojana Bhavan, Sansad Marg, New Delhi, Dated 21st August, 2006 Subject: Constitution of the Task Force on Islands, Corals, Mangroves & Wetlands for the Environment & Forests Sector for the Eleventh Five-Year Plan (2007- 2012). It has been decided to set up a Task Force on Islands, corals, mangroves & wetlands for the Environment & Forests Sector for the Eleventh Five-Year Plan. The composition of the Task Force will be as under: 1. Shri J.R.B.Alfred, Director, ZSI Chairman 2. Shri Pankaj Shekhsaria, Kalpavriksh, Pune Member 3. Mr. Harry Andrews, Madras Crocodile Bank Trust , Tamil Nadu Member 4. Dr. V. Selvam, Programme Director, MSSRF, Chennai Member Terms of Reference of the Task Force will be as follows: • Review the current laws, policies, procedures and practices related to conservation and sustainable use of island, coral, mangrove and wetland ecosystems and recommend correctives. -
Agatti Island, UT of Lakshadweep
Socioeconomic Monitoring for Coastal Managers of South Asia: Field Trials and Baseline Surveys Agatti Island, UT of Lakshadweep Project completion Report: NA10NOS4630055 Project Supervisor : Vineeta Hoon Site Coordinators: Idrees Babu and Noushad Mohammed Agatti team: Amina.K, Abida.FM, Bushra M.I, Busthanudheen P.K, Hajarabeebi MC, Hassan K, Kadeeshoma C.P, Koyamon K.G, Namsir Babu.MS, Noorul Ameen T.K, Mohammed Abdul Raheem D A, Shahnas beegam.k, Shahnas.K.P, Sikandar Hussain, Zakeer Husain, C.K, March 2012 This volume contains the results of the Socioeconomic Assessment and monitoring project supported by IUCN/ NOAA Prepared by: 1. The Centre for Action Research on Environment Science and Society, Chennai 600 094 2. Lakshadweep Marine Research and Conservation Centre, Kavaratti island, U.T of Lakshadweep. Citation: Vineeta Hoon and Idrees Babu, 2012, Socioeconomic Monitoring and Assessment for Coral Reef Management at Agatti Island, UT of Lakshadweep, CARESS/ LMRCC, India Cover Photo: A reef fisherman selling his catch Photo credit: Idrees Babu 2 Table of Contents Executive Summary 7 Acknowledgements 8 Glossary of Native Terms 9 List of Acronyms 10 1. Introduction 11 1.1 Settlement History 11 1.2 Dependence on Marine Resources 13 1.3 Project Goals 15 1.4 Report Chapters 15 2. Methodology of Project Execution 17 2.1 SocMon Workshop 17 2.2 Data Collection 18 2.3 Data Validation 20 3. Site Description and Island Infrastructure 21 3.1 Site description 23 3.2. Community Infrastructure 25 4. Community Level Demographics 29 4.1 Socio cultural status 29 4.2 Land Ownership 29 4.3 Demographic characteristics 30 4.4 Household size 30 4.5. -

Technical Report on Design and Execution of Desalination Plants in Minicoy and Agatti, UT Lakshadweep
Technical Report on Design and Execution of Desalination Plants in Minicoy and Agatti, UT Lakshadweep Sea water desalination is attaining increasing attention of present day policy makers, especially with the growing demands that urbanization, population explosion, irregular rainfall and ground water contamination on the fragile natural resources. ‘Low Temperature Thermal Desalination’ (LTTD) is one process that uses the availability of a temperature gradient between two water bodies, such as the Ocean Thermal Gradient that describes temperature variation across the depth of the oceans, to obtain fresh water. The available thermal gradient between warmer surface water and colder deep seawater is utilized by flash evaporating the warm water at low temperatures and condensing the resultant vapour with cold water. Earth System Science Organization, Ministry of Earth Sciences, Government of India, Through National Institute of Ocean Technology (ESSO-NIOT), India, has successfully demonstrated the 100 m3/day capacity land based desalination plant in the remote islands of Agatti and Minicoy of UT Lakshadweep in 2011 following the initial success of similar capacity plant at Kavaratti island. Temperature (oC) 0 10 20 30 40 0 -50 -100 -150 -200 -250 Depth (m) Depth -300 -350 -400 -450 Fig. 1 Schematic Diagram of LTTD working principle (left) and the Ocean Thermal Gradient in coastal waters (NIO, Goa, 2000) The bathymetry around the islands allows availability of 350-380m water depth within 400- 1000m from the shore, for drawing water at 10-12oC. The temperature gradient of 16oC between the deep sea cold water at 12oC and the warm surface sea water at about 28oC is utilized in the LTTD process as shown Fig. -

Administration of the Union Territory of Lakshadweep
ADMINISTRATION OF THE UNION TERRITORY OF LAKSHADWEEP PRESENTATION OF SHRI J. K.DADOO, IAS ADMINISTRATOR 55TH NATIONAL DEVELOPMENT COUNCIL MEETING AT NEW DELHI ON 24TH JULY, 2010 Hon’ble Prime Minister, Deputy Chairman of Planning Commission, Members of National Development Council, Union Ministers, Chief Ministers and distinguished dignitaries: It is a matter of privilege for me to participate in the deliberations of the 55th National Development Council (NDC) convened by our Hon’ble Prime Minister to consider and approve the Mid-Term Appraisal of 11th Five Year Plan inter-alia with other high focus issues. I represent the U.T. of Lakshadweep which is a group of 36 Coral Islands with the total land area of just 32 Sq. kms. 10 Islands are inhabited and these Islands are at a distance of about 300 to 450 kms. from mainland, Kochi. From pin to plane, everything comes from the mainland and this makes these Islands the remotest and the most difficult to live in. Basic infrastructure is limited and yet nearly 70,000 people inhabit these 10 Islands. Shipping is the backbone and Mangalore is the food lifeline while Calicut is the fuel lifeline. All other provisions are supplied from Kochi. In the above circumstances, regular flights from Kochi, Mangalore and Calicut to Agatti, the only Airport are imperative. At least 4 to 5 all weather ships which can ensure smooth and regular transportation of goods and passengers in the 5 months of the monsoon are equally paramount. With rising aspirations of the people, a fast speed vessel which can complete the journey between mainland and the Islands in about 6 hours, and provide a Rajdhani train kind of link would be extremely beneficial for the Islands. -

Complex Ecological Pathways Underlie Perceptions of Conflict Between Green Turtles and Fishers in the Lakshadweep Islands
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/255910112 Complex ecological pathways underlie perceptions of conflict between green turtles and fishers in the Lakshadweep Islands Article in Biological Conservation · November 2013 DOI: 10.1016/j.biocon.2013.07.014 CITATIONS READS 4 105 4 authors, including: Nachiket Kelkar Teresa Alcoverro Ashoka Trust for Research in Ecology and t… Spanish National Research Council 27 PUBLICATIONS 107 CITATIONS 111 PUBLICATIONS 2,692 CITATIONS SEE PROFILE SEE PROFILE M. D. Madhusudan Nature Conservation Foundation 62 PUBLICATIONS 973 CITATIONS SEE PROFILE All in-text references underlined in blue are linked to publications on ResearchGate, Available from: Rohan Arthur letting you access and read them immediately. Retrieved on: 15 September 2016 Biological Conservation 167 (2013) 25–34 Contents lists available at ScienceDirect Biological Conservation journal homepage: www.elsevier.com/locate/biocon Complex ecological pathways underlie perceptions of conflict between green turtles and fishers in the Lakshadweep Islands a,b, a a,b a Rohan Arthur ⇑, Nachiket Kelkar , Teresa Alcoverro , M.D. Madhusudan a Nature Conservation Foundation, 3076/5, Gokulam Park, Mysore 570002, India b Centre d’Estudis Avançats de Blanes (CSIC), Accés a la Cala St. Francesc, 14, Spain article info abstract Article history: Managing human–wildlife conflict is often complicated by apparent mismatches between community Received 5 January 2013 perceptions and measures of directly incurred losses. Fishers in Agatti Island (Lakshadweep, India) asso- Received in revised form 2 July 2013 ciate recent increases in green turtle (Chelonia mydas) populations with declining fish catches, resulting in Accepted 12 July 2013 targeted killing of turtles. -

1 Government of India Lakshadweep Administration (DEPARTMENT OF
THE LAKSHADWEEP GAZETTE EXTRAORDINARY 1 VOL. LVI. No. 28 THURSDAY 15th OCTOBER, 2020 / 23rd ASVINA, 1942 (SAKA) Government of India Lakshadweep Administration (DEPARTMENT OF ENVIRONMENT AND FOREST) Kavaratti Island, Dated : 14-10-2020. NOTIFICATION F.No. 2/22/2020-E&F:- The Administrator, Union Territory of Lakshadweep Administration is pleased to publish the Lakshadweep Forest Code-2020 of the Department of Environment and Forest, Union Territory of Lakshadweep Administration and is declared as the Official Forest Code of the department with effect from the date of publication of this notification in the Official Gazette. This is issued with the approval of Hon’ble Administrator vide Diary No. 1752, dated 07-10-2020. Sd/- (DAMODHAR A.T., IFS) Secretary, Environment & Forest and Chief Wildlife Warden. LGP.Kvt. G-1389/10 -20/50 PRICE: 75 PAISE 2 THE LAKSHADWEEP GAZETTE EXTRAORDINARY CHAPTER – I ORGANISATION OF THE DEPARTMENT OF ENVIRONMENT AND FOREST 1 – GENERAL 1.1 Introduction Natural ecosystems are a dynamic ecosystem consisting of plants, animals & microorganisms safeguarding the ecological security of the nation. It provides various ecosystem services essential for the very survival of the human beings. The aim of the Department of Environment & Forest in UT of Lakshadweep is department and services ensure environmental stability and maintenance of ecological balance including atmospheric equilibrium which are vital for sustenance ofall life forms, human, animals and plants. This policy will be instrumental in strengthening ecological security, sustainable ecological management, and participatory management. This also ensures to safeguard the ecological and livelihood security of people, of the present and future generations, based on sustainable management of the ecosystem services thereby the stability of the fragile eco-systems. -

Human Impacts on Lakshadweep Atolls, India
HUMAN IMPACTS ON LAKSHADWEEP ATOLLS, INDIA Abstract coconuts per year. There are about 6200 fishermen The Lakshadweep (Laccadive) islands are situated engaged in fishing using 900 boats. The total fish in the Arabian Sea about 225 to 450 km from the landings in these islands per year are about 15000 tonnes. southwest coast of India. These islands situated 1 to 2 The people are dependent on the mainland for all meters above mean sea level has a very thin lens of fresh essential supplies including fuel, vegetables, packaged water floating over the seawater. Almost all fresh water foods, and infrastructure. sources are contaminated due to seawater intrusion. The Lakshadweep islands are lying along a north-south drinking water wells contain excessive nitrate axis (except Androth Island) with lagoon on the west and concentration originating from septic tanks, other human open sea on the east. Estimated total coral reef area in wastes and fertilizers used in garden. All drinking water these islands is 276 km2 including the reef flat area of sources show positive bacterial (faecal coliform) count 136.5 km2 (Bahuguna and Nayak, 1998). Taxonomic exceeding the normal level. Increasing population studies of Lakshadweep corals are almost restricted to pressure (2600 people / km2) leading to the accumulation the pioneering works of Pillai (1989) and he showed the of more diseases in corals. The newly emerging disease presence of 104 species under 37 genera. The extensive Red Plague Syndrome is spreading very fast in these surveys made by the author during the year 2002 to 2003 islands. The anthropogenic impacts on coral reefs are and the results showing additional 9 species were present discussed in the paper in detail. -

E:\Published Issues\2015\Oct15\
NEWS AND NOTES A Comprehension on Coral Atolls of the Remote Lakshadweep, Arabian Sea, Indian Ocean – Tapas Kumar Mallik, Retd. Director, Geol. Surv. India, Kolkata (Email: tkmallik@ rediffmail.com) The Lakshadweep are least studied coral atoll group situated crater of a sunken volcano. The atoll surrounds a body of water in the northern part of the Laccadive-Chagos ridge at a distance called a lagoon. One or more channels connect the lagoon to the of 200-300 km from the west coast of India. The ridge is a open sea. continuation of the Aravalli Mountains and the islands are the Growth of coral will require clear shallow water with a remnants of submerged mountain cliffs. They lie between latitude particular temperature. Corals are formed by tiny lime secreting 80-140N and longitude 710-740E. The islands cover an area of only animal growing in millions in different shapes like branching 32 km2 and Kavaratti is the capital of the Lakshadweep group of trees, large domes, small irregular crusts, or tiny organ pipes. islands. The atolls have formed on the Lakshadweep-Chagos ridge. According to Menard (1986) plate tectonics is the key to under- There are 11 major islands and lagoons (Kavaratti, Kalpeni, Agatti, stand the creation, distribution and history of the islands. Chetlat, Bitra, Kiltan, Kadmat, Amini, Bangaram, Suheli, Other important features which play a major role are changes in Minicoy), 4 submerged reefs (Baliapani, Cheriapani, Perumalpar, sea level. Androth) and 5 banks (Bassas de Pedro, Sessostris, Coradivh, Islands in most of the atolls are situated on eastern leeward Aminipitti, Elikalpeni). -

COVID 19 Situation in Lakshadweep Islands
Vol. * XXXVI. No. 09 * KAVARATTI *WEDNESDAY * 23 JUNE 2021. Price Rs. 2. Hon'ble Administrator Collector and Chairman Shri Praful Patel District Disaster Manage- A COVID patient evacuating visited Lakshadweep and ment Authority Shri S. from Chetlat by Ambulance discussed various Asker Ali, IAS chairing a helicopter. developmental activities of meeting at Agatti Island. the territory. COVID 19 Situation in Hon'ble Administrator visited Lakshadweep Islands Lakshadweep 28th December, 2020, Collector said. Following the revised SOP, livelihood activities resumed in the islands. 945 tourists visited the islands in the five months since SOP was revised. Mechanized sailing vessels operated in the islands for 380 times. Consequently, construction activities A view from the COVID test at Kavaratti. started in the islands. Kavaratti : Due to the considering the genuine Flight operations were COVID 19 pandemic, requirement of the local also resumed. During this Lakshadweep islands population in terms of period, 35,170 people had highly restricted livelihood activities, came from mainland to Hon'ble Administrator Shri Praful Patel chairing a meeting conducted at movement of men and developmental islands majority of them Secretariat Conference Hall, Kavaratti. are local population and material from the mainland requirements of the local people in the to safeguard and protect considered, then 92,231 people travelled by to the islands and vice Administration and the islands also contributed its citizens from the Lakshadweep ships and HSC within versa from March prevailing MHA Guidelines significantly to the rise of pandemic. As a result of Administration has Lakshadweep islands, he to December 2020. during that time. As per COVID 19 cases in such continuous efforts, vaccinated 97.16% of its said. -

THE LAKSHADWEEP TIMES Vol
THE LAKSHADWEEP TIMES Vol. * XXXV. No. 22 * KAVARATTI *FRIDAY * 23 OCTOBER 2020. Price Rs. 2. TOP STORIES Advisor to Hon’ble Administrator and Indigenously built stealth High Level Officials Visited Agatti Island corvette INS Kavaratti commissioned into Indian Navy Chief of Army Staff Gen MM Naravane commissioned the last of four indigenously built Advisor to Hon’ble Administrator and high level officials of Advisor to Hon’ble Administrator and high level officials hearing anti-submarine warfare UT Administration is being received by Deputy grievances from public at Agatti. (ASW) stealth corvettes Collector,Chairperson,VDP and others. ‘INS Kavaratti’ into the Agatti: Shri. P. During the visit at Households. He also needy requirements. E-Hospital, Oxygen plant Indian Navy in Krishnamurthy, Advisor to Agatti, the Advisor to inaugurated the Lobster While interacting with etc. He also directed to Visakhapatnam on concerned the increase Thursday. Hon’ble Administrator and Hon’ble Administrator and Holding and Fattening Deputy Collector, the contingent fund and Army Chief General high level officials of UT his team visited various Cages-Plot Farm Chairperson VDP, Manoj Mukund Administration visited places like Govt. Senior established at Agatti Administrative Officer speed up the annual Naravane said, “The Agatti Island on 17th Secondary School, Coir jointly by the Department RGSH and Manager procurement of OPD commissioning of INS October 2020. Production Centre, of Fisheries, UTL and DAYA, Advisor to Hon’ble medicines. Kavaratti marks yet Smt. A.M. Kadeeshabi, Western Side Jetty, ICAR-CMFRI sponsored Administrator has given While visiting Govt. another significant step Deputy Collector and Smt Agriculture plot, Rajiv by NFDB GOI by putting directions to concerned Senior Secondary School, in securing our country’s A. -
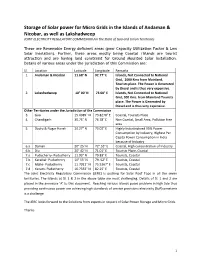
Storage of Solar Power for Micro Grids in the Islands of Andaman
Storage of Solar power for Micro Grids in the Islands of Andaman & Nicobar, as well as Lakshadweep JOINT ELECTRICITY REGULATORY COMMISSION For the State of Goa and Union Territories These are Renewable Energy deficient areas (poor Capacity Utilization Factor & Low Solar Insolation). Further, these areas mostly being Coastal /Islands are tourist attraction and are having land constraint for Ground Mounted Solar Installation. Details of various areas under the jurisdiction of this Commission are: Sl. Location Latitude Longitude Remarks 1. Andaman & Nicobar 11.68° N 92.77° E Islands, Not Connected to National Grid, 1000 Kms from Mainland, Tourists place. The Power is Generated by Diesel and is thus very expensive. 2. Lakashadweep 10° 00' N 73.00° E Islands, Not Connected to National Grid, 300 Kms. from Mainland Tourists place. The Power is Generated by Diesel and is thus very expensive. Other Territories under the Jurisdiction of the Commission 3. Goa 15.4989° N 73.8278° E Coastal, Tourists Place 4. Chandigarh 30.75° N 76.78° E Non Coastal, Small Area, Pollution free area 5. Dadra & Nagar Haveli 20.27° N 73.02° E Highly Industrialized 95% Power Consumption by Industry, Highest Per Capita Power Consumption in India because of Industry 6.a Daman 20° 25' N 72°.53° E Coastal, High concentration of Industry 6.b Diu 20° 42' N 71.01° E Tourists Place, Coastal 7.a Puducherry- Puducherry 11.93° N 79.83° E Tourists, Coastal 7.b Karaikal- Puducherry 10° 55' N 79. 52° E Tourists, Coastal 7.c Mahe- Puducherry 11.7011° N 75.5367° E Tourists, Coastal 7.d Yanam- Puducherry 16.7333° N 82.25° E Tourists, Coastal The Joint Electricity Regulatory Commission (JERC) is pushing for Solar Roof Tops in all the seven territories.