UCLA Previously Published Works
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MUC4/MUC16/Muc20high Signature As a Marker of Poor Prognostic for Pancreatic, Colon and Stomach Cancers
Jonckheere and Van Seuningen J Transl Med (2018) 16:259 https://doi.org/10.1186/s12967-018-1632-2 Journal of Translational Medicine RESEARCH Open Access Integrative analysis of the cancer genome atlas and cancer cell lines encyclopedia large‑scale genomic databases: MUC4/MUC16/ MUC20 signature is associated with poor survival in human carcinomas Nicolas Jonckheere* and Isabelle Van Seuningen* Abstract Background: MUC4 is a membrane-bound mucin that promotes carcinogenetic progression and is often proposed as a promising biomarker for various carcinomas. In this manuscript, we analyzed large scale genomic datasets in order to evaluate MUC4 expression, identify genes that are correlated with MUC4 and propose new signatures as a prognostic marker of epithelial cancers. Methods: Using cBioportal or SurvExpress tools, we studied MUC4 expression in large-scale genomic public datasets of human cancer (the cancer genome atlas, TCGA) and cancer cell line encyclopedia (CCLE). Results: We identifed 187 co-expressed genes for which the expression is correlated with MUC4 expression. Gene ontology analysis showed they are notably involved in cell adhesion, cell–cell junctions, glycosylation and cell signal- ing. In addition, we showed that MUC4 expression is correlated with MUC16 and MUC20, two other membrane-bound mucins. We showed that MUC4 expression is associated with a poorer overall survival in TCGA cancers with diferent localizations including pancreatic cancer, bladder cancer, colon cancer, lung adenocarcinoma, lung squamous adeno- carcinoma, skin cancer and stomach cancer. We showed that the combination of MUC4, MUC16 and MUC20 signature is associated with statistically signifcant reduced overall survival and increased hazard ratio in pancreatic, colon and stomach cancer. -

Targeting PH Domain Proteins for Cancer Therapy
The Texas Medical Center Library DigitalCommons@TMC The University of Texas MD Anderson Cancer Center UTHealth Graduate School of The University of Texas MD Anderson Cancer Biomedical Sciences Dissertations and Theses Center UTHealth Graduate School of (Open Access) Biomedical Sciences 12-2018 Targeting PH domain proteins for cancer therapy Zhi Tan Follow this and additional works at: https://digitalcommons.library.tmc.edu/utgsbs_dissertations Part of the Bioinformatics Commons, Medicinal Chemistry and Pharmaceutics Commons, Neoplasms Commons, and the Pharmacology Commons Recommended Citation Tan, Zhi, "Targeting PH domain proteins for cancer therapy" (2018). The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access). 910. https://digitalcommons.library.tmc.edu/utgsbs_dissertations/910 This Dissertation (PhD) is brought to you for free and open access by the The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences at DigitalCommons@TMC. It has been accepted for inclusion in The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access) by an authorized administrator of DigitalCommons@TMC. For more information, please contact [email protected]. TARGETING PH DOMAIN PROTEINS FOR CANCER THERAPY by Zhi Tan Approval page APPROVED: _____________________________________________ Advisory Professor, Shuxing Zhang, Ph.D. _____________________________________________ -

Genetic Overlap Between Alzheimer&Rsquo
Molecular Psychiatry (2015) 20, 1588–1595 © 2015 Macmillan Publishers Limited All rights reserved 1359-4184/15 www.nature.com/mp ORIGINAL ARTICLE Genetic overlap between Alzheimer’s disease and Parkinson’s disease at the MAPT locus RS Desikan1, AJ Schork2, Y Wang3,4, A Witoelar4, M Sharma5,6, LK McEvoy1, D Holland3, JB Brewer1,3, C-H Chen1,7, WK Thompson7, D Harold8, J Williams8, MJ Owen8,MCO’Donovan8, MA Pericak-Vance9, R Mayeux10, JL Haines11, LA Farrer12, GD Schellenberg13, P Heutink14, AB Singleton15, A Brice16, NW Wood17, J Hardy18, M Martinez19, SH Choi20, A DeStefano20,21, MA Ikram22, JC Bis23, A Smith24, AL Fitzpatrick25, L Launer26, C van Duijn22, S Seshadri21,27, ID Ulstein28, D Aarsland29,30,31, T Fladby32,33, S Djurovic4, BT Hyman34, J Snaedal35, H Stefansson36, K Stefansson36,37, T Gasser5, OA Andreassen4,7, AM Dale1,2,3,7for the ADNI38ADGC, GERAD, CHARGE and IPDGC Investigators39 We investigated the genetic overlap between Alzheimer’s disease (AD) and Parkinson’s disease (PD). Using summary statistics (P-values) from large recent genome-wide association studies (GWAS) (total n = 89 904 individuals), we sought to identify single nucleotide polymorphisms (SNPs) associating with both AD and PD. We found and replicated association of both AD and PD with the A allele of rs393152 within the extended MAPT region on chromosome 17 (meta analysis P-value across five independent AD cohorts = 1.65 × 10− 7). In independent datasets, we found a dose-dependent effect of the A allele of rs393152 on intra-cerebral MAPT transcript levels and volume loss within the entorhinal cortex and hippocampus. -

Mouse Arhgap27 Knockout Project (CRISPR/Cas9)
https://www.alphaknockout.com Mouse Arhgap27 Knockout Project (CRISPR/Cas9) Objective: To create a Arhgap27 knockout Mouse model (C57BL/6J) by CRISPR/Cas-mediated genome engineering. Strategy summary: The Arhgap27 gene (NCBI Reference Sequence: NM_001205236.1 ; Ensembl: ENSMUSG00000034255 ) is located on Mouse chromosome 11. 16 exons are identified, with the ATG start codon in exon 1 and the TGA stop codon in exon 16 (Transcript: ENSMUST00000107024). Exon 4~10 will be selected as target site. Cas9 and gRNA will be co-injected into fertilized eggs for KO Mouse production. The pups will be genotyped by PCR followed by sequencing analysis. Note: Exon 4 starts from about 48.25% of the coding region. Exon 4~10 covers 24.32% of the coding region. The size of effective KO region: ~2282 bp. The KO region does not have any other known gene. Page 1 of 9 https://www.alphaknockout.com Overview of the Targeting Strategy Wildtype allele 5' gRNA region gRNA region 3' 1 4 5 6 7 8 9 10 11 16 Legends Exon of mouse Arhgap27 Knockout region Page 2 of 9 https://www.alphaknockout.com Overview of the Dot Plot (up) Window size: 15 bp Forward Reverse Complement Sequence 12 Note: The 178 bp section upstream of Exon 4 is aligned with itself to determine if there are tandem repeats. No significant tandem repeat is found in the dot plot matrix. So this region is suitable for PCR screening or sequencing analysis. Overview of the Dot Plot (down) Window size: 15 bp Forward Reverse Complement Sequence 12 Note: The 124 bp section downstream of Exon 10 is aligned with itself to determine if there are tandem repeats. -

The Genetic Case for Cardiorespiratory Fitness As a Clinical Vital Sign and the Routine
medRxiv preprint doi: https://doi.org/10.1101/2020.12.08.20243337; this version posted December 9, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . UKB cardiorespiratory fitness and physical activity 1 The genetic case for cardiorespiratory fitness as a clinical vital sign and the routine 2 prescription of physical activity in healthcare 3 4 Ken B. Hanscombe1, 4, Elodie Persyn1, Matthew Traylor2, Kylie P. Glanville4, Mark Hamer 3, Jonathan R. I. Coleman4, 5 Cathryn M. Lewis1, 4 6 7 1Department of Medical & Molecular Genetics, King's College London, London, United Kingdom, 2Queen Mary 8 University of London, London, United Kingdom, 3Institute of Sport Exercise & Health, Division of Surgery and 9 Interventional Science, University College London, London, United Kingdom, 4Social, Genetic and Developmental 10 Psychiatry Centre, King's College London, London, United Kingdom 11 12 Ken B. Hanscombe [email protected] (corresponding author) 13 Elodie Persyn [email protected] 14 Matthew Traylor [email protected] 15 Kylie P. Glanville [email protected] 16 Mark Hamer [email protected] 17 Jonathan R. I. Coleman [email protected] 18 Cathryn M. Lewis [email protected] 19 20 21 Abstract 22 23 Background: Cardiorespiratory fitness (CRF) and physical activity (PA) are well-established predictors of morbidity and 24 all-cause mortality. However, CRF is not routinely measured and PA not routinely prescribed as part of standard 25 healthcare. -

Supplementary Appendix Table of Contents
Supplementary Appendix This appendix has been provided by the authors to give readers additional information about their work. Table of Contents Supplementary Note ........................................................................................................................... 1 Author contributions ............................................................................................................................... 1 Additional authors from study groups .............................................................................................. 2 Task Force COVID-19 Humanitas ......................................................................................................................................... 2 TASK FORCE COVID-19 HUMANITAS GAVAZZENI & CASTELLI ............................................................................. 3 COVICAT Study Group ............................................................................................................................................................... 4 Pa COVID-19 Study Group ....................................................................................................................................................... 5 Covid-19 Aachen Study (COVAS) .......................................................................................................................................... 5 Norwegian SARS-CoV-2 Study group ................................................................................................................................. -

Membrane and Protein Interactions of the Pleckstrin Homology Domain Superfamily
Membranes 2015, 5, 646-663; doi:10.3390/membranes5040646 OPEN ACCESS membranes ISSN 2077-0375 www.mdpi.com/journal/membranes Article Membrane and Protein Interactions of the Pleckstrin Homology Domain Superfamily Marc Lenoir 1, Irina Kufareva 2, Ruben Abagyan 2, and Michael Overduin 3,* 1 School of Cancer Sciences, Faculty of Medical and Dental Sciences, University of Birmingham, Birmingham B15 2TT, UK; E-Mail: [email protected] 2 Skaggs School of Pharmacy and Pharmaceutical Sciences, University of California, San Diego, 9500 Gilman Drive, La Jolla, CA 92093, USA; E-Mails: [email protected] (I.K.); [email protected] (R.A.) 3 Department of Biochemistry, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, AB T6G 2H7, Canada * Author to whom correspondence should be addressed: E-Mail: [email protected]; Tel.: +1-780-492-3357; Fax: +1-780-492-0886. Academic Editor: Shiro Suetsugu Received: 15 September 2015 / Accepted: 16 October 2015 / Published: 23 October 2015 Abstract: The human genome encodes about 285 proteins that contain at least one annotated pleckstrin homology (PH) domain. As the first phosphoinositide binding module domain to be discovered, the PH domain recruits diverse protein architectures to cellular membranes. PH domains constitute one of the largest protein superfamilies, and have diverged to regulate many different signaling proteins and modules such as Dbl homology (DH) and Tec homology (TH) domains. The ligands of approximately 70 PH domains have been validated by binding assays and complexed structures, allowing meaningful extrapolation across the entire superfamily. Here the Membrane Optimal Docking Area (MODA) program is used at a genome-wide level to identify all membrane docking PH structures and map their lipid-binding determinants. -

The Pdx1 Bound Swi/Snf Chromatin Remodeling Complex Regulates Pancreatic Progenitor Cell Proliferation and Mature Islet Β Cell
Page 1 of 125 Diabetes The Pdx1 bound Swi/Snf chromatin remodeling complex regulates pancreatic progenitor cell proliferation and mature islet β cell function Jason M. Spaeth1,2, Jin-Hua Liu1, Daniel Peters3, Min Guo1, Anna B. Osipovich1, Fardin Mohammadi3, Nilotpal Roy4, Anil Bhushan4, Mark A. Magnuson1, Matthias Hebrok4, Christopher V. E. Wright3, Roland Stein1,5 1 Department of Molecular Physiology and Biophysics, Vanderbilt University, Nashville, TN 2 Present address: Department of Pediatrics, Indiana University School of Medicine, Indianapolis, IN 3 Department of Cell and Developmental Biology, Vanderbilt University, Nashville, TN 4 Diabetes Center, Department of Medicine, UCSF, San Francisco, California 5 Corresponding author: [email protected]; (615)322-7026 1 Diabetes Publish Ahead of Print, published online June 14, 2019 Diabetes Page 2 of 125 Abstract Transcription factors positively and/or negatively impact gene expression by recruiting coregulatory factors, which interact through protein-protein binding. Here we demonstrate that mouse pancreas size and islet β cell function are controlled by the ATP-dependent Swi/Snf chromatin remodeling coregulatory complex that physically associates with Pdx1, a diabetes- linked transcription factor essential to pancreatic morphogenesis and adult islet-cell function and maintenance. Early embryonic deletion of just the Swi/Snf Brg1 ATPase subunit reduced multipotent pancreatic progenitor cell proliferation and resulted in pancreas hypoplasia. In contrast, removal of both Swi/Snf ATPase subunits, Brg1 and Brm, was necessary to compromise adult islet β cell activity, which included whole animal glucose intolerance, hyperglycemia and impaired insulin secretion. Notably, lineage-tracing analysis revealed Swi/Snf-deficient β cells lost the ability to produce the mRNAs for insulin and other key metabolic genes without effecting the expression of many essential islet-enriched transcription factors. -

Title: a Yeast Phenomic Model for the Influence of Warburg Metabolism on Genetic
bioRxiv preprint doi: https://doi.org/10.1101/517490; this version posted January 15, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. 1 Title Page: 2 3 Title: A yeast phenomic model for the influence of Warburg metabolism on genetic 4 buffering of doxorubicin 5 6 Authors: Sean M. Santos1 and John L. Hartman IV1 7 1. University of Alabama at Birmingham, Department of Genetics, Birmingham, AL 8 Email: [email protected], [email protected] 9 Corresponding author: [email protected] 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 1 bioRxiv preprint doi: https://doi.org/10.1101/517490; this version posted January 15, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. 26 Abstract: 27 Background: 28 Saccharomyces cerevisiae represses respiration in the presence of adequate glucose, 29 mimicking the Warburg effect, termed aerobic glycolysis. We conducted yeast phenomic 30 experiments to characterize differential doxorubicin-gene interaction, in the context of 31 respiration vs. glycolysis. The resulting systems level biology about doxorubicin 32 cytotoxicity, including the influence of the Warburg effect, was integrated with cancer 33 pharmacogenomics data to identify potentially causal correlations between differential 34 gene expression and anti-cancer efficacy. -

Identification of Novel Regulatory Genes in Acetaminophen
IDENTIFICATION OF NOVEL REGULATORY GENES IN ACETAMINOPHEN INDUCED HEPATOCYTE TOXICITY BY A GENOME-WIDE CRISPR/CAS9 SCREEN A THESIS IN Cell Biology and Biophysics and Bioinformatics Presented to the Faculty of the University of Missouri-Kansas City in partial fulfillment of the requirements for the degree DOCTOR OF PHILOSOPHY By KATHERINE ANNE SHORTT B.S, Indiana University, Bloomington, 2011 M.S, University of Missouri, Kansas City, 2014 Kansas City, Missouri 2018 © 2018 Katherine Shortt All Rights Reserved IDENTIFICATION OF NOVEL REGULATORY GENES IN ACETAMINOPHEN INDUCED HEPATOCYTE TOXICITY BY A GENOME-WIDE CRISPR/CAS9 SCREEN Katherine Anne Shortt, Candidate for the Doctor of Philosophy degree, University of Missouri-Kansas City, 2018 ABSTRACT Acetaminophen (APAP) is a commonly used analgesic responsible for over 56,000 overdose-related emergency room visits annually. A long asymptomatic period and limited treatment options result in a high rate of liver failure, generally resulting in either organ transplant or mortality. The underlying molecular mechanisms of injury are not well understood and effective therapy is limited. Identification of previously unknown genetic risk factors would provide new mechanistic insights and new therapeutic targets for APAP induced hepatocyte toxicity or liver injury. This study used a genome-wide CRISPR/Cas9 screen to evaluate genes that are protective against or cause susceptibility to APAP-induced liver injury. HuH7 human hepatocellular carcinoma cells containing CRISPR/Cas9 gene knockouts were treated with 15mM APAP for 30 minutes to 4 days. A gene expression profile was developed based on the 1) top screening hits, 2) overlap with gene expression data of APAP overdosed human patients, and 3) biological interpretation including assessment of known and suspected iii APAP-associated genes and their therapeutic potential, predicted affected biological pathways, and functionally validated candidate genes. -
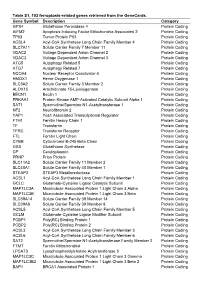
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -

The Manipulation of Host Transcription by the ANKH Effector of Legionella
University of Louisville ThinkIR: The University of Louisville's Institutional Repository Electronic Theses and Dissertations 12-2019 The manipulation of host transcription by the ANKH effector of legionella. Juanita E. Von Dwingelo Follow this and additional works at: https://ir.library.louisville.edu/etd Part of the Bacterial Infections and Mycoses Commons Recommended Citation Von Dwingelo, Juanita E., "The manipulation of host transcription by the ANKH effector of legionella." (2019). Electronic Theses and Dissertations. Paper 3310. https://doi.org/10.18297/etd/3310 This Doctoral Dissertation is brought to you for free and open access by ThinkIR: The University of Louisville's Institutional Repository. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of ThinkIR: The University of Louisville's Institutional Repository. This title appears here courtesy of the author, who has retained all other copyrights. For more information, please contact [email protected]. THE MANIPULATION OF HOST TRANSCRIPTION BY THE ANKH EFFECTOR OF LEGIONELLA By Juanita E Von Dwingelo B.Sc., Murray State University, 2010 M.S., Murray State University, 2012 M.S., University of Louisville, 2014 A Dissertation Submitted to the Faculty of the School of Medicine of the University of Louisville In Partial Fulfillment of the Requirements For the Degree of Doctor of Philosophy In Microbiology and Immunology Department of Microbiology and Immunology University of Louisville Louisville, Kentucky December 2019 Copyright 2019 by Juanita Von Dwingelo All rights reserved THE MANIPULATION OF HOST TRANSCRIPTION BY THE ANKH EFFECTOR OF LEGIONELLA By Juanita E. Von Dwingelo B.Sc., Murray State Univesity, 2010 M.S., Murray State University, 2012 M.S., University of Louisville, 2014 A Dissertation Approved on August 15, 2019 By the following Dissertation Committee: ______________________________________________ Dissertation Director, Dr.