New Perspective in Diagnostics of Mitochondrial Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NDUFAF1 Antibody
Efficient Professional Protein and Antibody Platforms NDUFAF1 Antibody Basic information: Catalog No.: UPA63763 Source: Rabbit Size: 50ul/100ul Clonality: monoclonal Concentration: 1mg/ml Isotype: Rabbit IgG Purification: Protein A purified. Useful Information: WB:1:1000 ICC:1:50-1:200 Applications: IHC:1:50-1:200 FC:1:50-1:100 Reactivity: Human Specificity: This antibody recognizes NDUFAF1 protein. Immunogen: Synthetic peptide within C terminal human NDUFAF1. This gene encodes a complex I assembly factor protein. Complex I (NADH-ubiquinone oxidoreductase) catalyzes the transfer of electrons from NADH to ubiquinone (coenzyme Q) in the first step of the mitochondrial respiratory chain, resulting in the translocation of protons across the inner mitochondrial membrane. The encoded protein is required for assembly of complex I, and mutations in this gene are a cause of mitochondrial complex I deficiency. Alternatively spliced transcript variants have been observed for Description: this gene, and a pseudogene of this gene is located on the long arm of chromosome 19. Part of the mitochondrial complex I assembly (MCIA) com- plex. The complex comprises at least TMEM126B, NDUFAF1, ECSIT, and ACAD9. Interacts with ECSIT. Interacts with ACAD9. At early stages of com- plex I assembly, it is found in intermediate subcomplexes that contain dif- ferent subunits including NDUFB6, NDUFA6, NDUFA9, NDUFS3, NDUFS7, ND1, ND2 and ND3 Uniprot: Q9Y375 Human BiowMW: 38 kDa Buffer: 1*TBS (pH7.4), 1%BSA, 50%Glycerol. Preservative: 0.05% Sodium Azide. Storage: Store at 4°C short term and -20°C long term. Avoid freeze-thaw cycles. Note: For research use only, not for use in diagnostic procedure. -

Molecular Mechanism of ACAD9 in Mitochondrial Respiratory Complex 1 Assembly
bioRxiv preprint doi: https://doi.org/10.1101/2021.01.07.425795; this version posted January 9, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Molecular mechanism of ACAD9 in mitochondrial respiratory complex 1 assembly Chuanwu Xia1, Baoying Lou1, Zhuji Fu1, Al-Walid Mohsen2, Jerry Vockley2, and Jung-Ja P. Kim1 1Department of Biochemistry, Medical College of Wisconsin, Milwaukee, Wisconsin, 53226, USA 2Department of Pediatrics, University of Pittsburgh School of Medicine, University of Pittsburgh, Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA 15224, USA Abstract ACAD9 belongs to the acyl-CoA dehydrogenase family, which catalyzes the α-β dehydrogenation of fatty acyl-CoA thioesters. Thus, it is involved in fatty acid β-oxidation (FAO). However, it is now known that the primary function of ACAD9 is as an essential chaperone for mitochondrial respiratory complex 1 assembly. ACAD9 interacts with ECSIT and NDUFAF1, forming the mitochondrial complex 1 assembly (MCIA) complex. Although the role of MCIA in the complex 1 assembly pathway is well studied, little is known about the molecular mechanism of the interactions among these three assembly factors. Our current studies reveal that when ECSIT interacts with ACAD9, the flavoenzyme loses the FAD cofactor and consequently loses its FAO activity, demonstrating that the two roles of ACAD9 are not compatible. ACAD9 binds to the carboxy-terminal half (C-ECSIT), and NDUFAF1 binds to the amino-terminal half of ECSIT. Although the binary complex of ACAD9 with ECSIT or with C-ECSIT is unstable and aggregates easily, the ternary complex of ACAD9-ECSIT-NDUFAF1 (i.e., the MCIA complex) is soluble and extremely stable. -

A Genetic Dissection of Mitochondrial Respiratory Chain Biogenesis
A GENETIC DISSECTION OF MITOCHONDRIAL RESPIRATORY CHAIN BIOGENESIS An Undergraduate Research Scholars Thesis by AARON GRIFFIN, SARAH THERIAULT, SHRISHIV TIMBALIA Submitted to Honors and Undergraduate Research Texas A&M University in partial fulfillment of the requirements for the designation as an UNDERGRADUATE RESEARCH SCHOLAR Approved by Research Advisor: Dr. Vishal Gohil May 2014 Major: Biochemistry, Genetics Biochemistry Biochemistry TABLE OF CONTENTS Page ABSTRACT .....................................................................................................................................1 CHAPTER I INTRODUCTION ...............................................................................................................3 II MATERIALS AND METHODS .........................................................................................7 Yeast strains, plasmids, and culture conditions .......................................................7 Yeast growth measurements ..................................................................................10 Yeast oxygen consumption and mitochondrial isolation .......................................11 SDS-PAGE and Western blotting ..........................................................................11 Sporulation, tetrad dissection, and genotyping ......................................................12 High-throughput phenotypic analysis of yeast strains ...........................................15 III RESULTS ..........................................................................................................................16 -
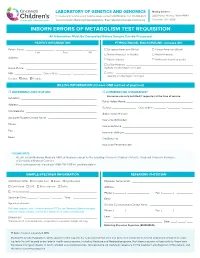
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______ -

Genes Investigated
BabyNEXTTM EXTENDED Investigated genes and associated diseases Gene Disease OMIM OMIM Condition RUSP gene Disease ABCC8 Familial hyperinsulinism 600509 256450 Metabolic disorder - ABCC8-related Inborn error of amino acid metabolism ABCD1 Adrenoleukodystrophy 300371 300100 Miscellaneous RUSP multisystem (C) * diseases ABCD4 Methylmalonic aciduria and 603214 614857 Metabolic disorder - homocystinuria, cblJ type Inborn error of amino acid metabolism ACAD8 Isobutyryl-CoA 604773 611283 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of (S) ** organic acid metabolism ACAD9 acyl-CoA dehydrogenase-9 611103 611126 Metabolic Disorder - (ACAD9) deficiency Inborn error of fatty acid metabolism ACADM Acyl-CoA dehydrogenase, 607008 201450 Metabolic Disorder - RUSP medium chain, deficiency of Inborn error of fatty (C) acid metabolism ACADS Acyl-CoA dehydrogenase, 606885 201470 Metabolic Disorder - RUSP short-chain, deficiency of Inborn error of fatty (S) acid metabolism ACADSB 2-methylbutyrylglycinuria 600301 610006 Metabolic Disorder - RUSP Inborn error of (S) organic acid metabolism ACADVL very long-chain acyl-CoA 609575 201475 Metabolic Disorder - RUSP dehydrogenase deficiency Inborn error of fatty (C) acid metabolism ACAT1 Alpha-methylacetoacetic 607809 203750 Metabolic Disorder - RUSP aciduria Inborn error of (C) organic acid metabolism ACSF3 Combined malonic and 614245 614265 Metabolic Disorder - methylmalonic aciduria Inborn error of organic acid metabolism 1 ADA Severe combined 608958 102700 Primary RUSP immunodeficiency due -

An Essential Role for ECSIT in Mitochondrial Complex I Assembly and Mitophagy in Macrophages
Article An Essential Role for ECSIT in Mitochondrial Complex I Assembly and Mitophagy in Macrophages Graphical Abstract Authors Fla´ via R.G. Carneiro, Alice Lepelley, John J. Seeley, Matthew S. Hayden, Sankar Ghosh Correspondence [email protected] In Brief Macrophages rely on fine-tuning their metabolism to fulfill their anti-bacterial functions. Carneiro et al. show that the complex I assembly factor ECSIT is an essential regulator of the balance between mitochondrial respiration and glycolysis and the maintenance of a healthy mitochondrial pool through mitophagy. Highlights d Loss of ECSIT in macrophages leads to a striking glycolytic shift d ECSIT is essential for complex I assembly and stability in macrophages d Role of ECSIT in mROS production and removal of damaged mitochondria by mitophagy Carneiro et al., 2018, Cell Reports 22, 2654–2666 March 6, 2018 ª 2018 The Author(s). https://doi.org/10.1016/j.celrep.2018.02.051 Cell Reports Article An Essential Role for ECSIT in Mitochondrial Complex I Assembly and Mitophagy in Macrophages Fla´ via R.G. Carneiro,1,3,4 Alice Lepelley,1,4 John J. Seeley,1 Matthew S. Hayden,1,2 and Sankar Ghosh1,5,* 1Department of Microbiology and Immunology, Vagelos College of Physicians and Surgeons, Columbia University, New York, NY 10032, USA 2Section of Dermatology, Department of Surgery, Dartmouth-Hitchcock Medical Center, Lebanon, NH 03756, USA 3FIOCRUZ, Center for Technological Development in Health (CDTS), Rio de Janeiro, Brazil 4These authors contributed equally 5Lead Contact *Correspondence: [email protected] https://doi.org/10.1016/j.celrep.2018.02.051 SUMMARY 2015). There, ECSIT-dependent mROS production promotes activation of the phagosomal nicotinamide adenine dinucleotide ECSIT is a mitochondrial complex I (CI)-associated phosphate (NADPH) oxidase system and ROS-dependent protein that has been shown to regulate the pro- killing of engulfed microbes (West et al., 2011). -

Genetic and Genomic Analysis of Hyperlipidemia, Obesity and Diabetes Using (C57BL/6J × TALLYHO/Jngj) F2 Mice
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Nutrition Publications and Other Works Nutrition 12-19-2010 Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P. Stewart Marshall University Hyoung Y. Kim University of Tennessee - Knoxville, [email protected] Arnold M. Saxton University of Tennessee - Knoxville, [email protected] Jung H. Kim Marshall University Follow this and additional works at: https://trace.tennessee.edu/utk_nutrpubs Part of the Animal Sciences Commons, and the Nutrition Commons Recommended Citation BMC Genomics 2010, 11:713 doi:10.1186/1471-2164-11-713 This Article is brought to you for free and open access by the Nutrition at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Nutrition Publications and Other Works by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. Stewart et al. BMC Genomics 2010, 11:713 http://www.biomedcentral.com/1471-2164/11/713 RESEARCH ARTICLE Open Access Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P Stewart1, Hyoung Yon Kim2, Arnold M Saxton3, Jung Han Kim1* Abstract Background: Type 2 diabetes (T2D) is the most common form of diabetes in humans and is closely associated with dyslipidemia and obesity that magnifies the mortality and morbidity related to T2D. The genetic contribution to human T2D and related metabolic disorders is evident, and mostly follows polygenic inheritance. The TALLYHO/ JngJ (TH) mice are a polygenic model for T2D characterized by obesity, hyperinsulinemia, impaired glucose uptake and tolerance, hyperlipidemia, and hyperglycemia. -

Low Abundance of the Matrix Arm of Complex I in Mitochondria Predicts Longevity in Mice
ARTICLE Received 24 Jan 2014 | Accepted 9 Apr 2014 | Published 12 May 2014 DOI: 10.1038/ncomms4837 OPEN Low abundance of the matrix arm of complex I in mitochondria predicts longevity in mice Satomi Miwa1, Howsun Jow2, Karen Baty3, Amy Johnson1, Rafal Czapiewski1, Gabriele Saretzki1, Achim Treumann3 & Thomas von Zglinicki1 Mitochondrial function is an important determinant of the ageing process; however, the mitochondrial properties that enable longevity are not well understood. Here we show that optimal assembly of mitochondrial complex I predicts longevity in mice. Using an unbiased high-coverage high-confidence approach, we demonstrate that electron transport chain proteins, especially the matrix arm subunits of complex I, are decreased in young long-living mice, which is associated with improved complex I assembly, higher complex I-linked state 3 oxygen consumption rates and decreased superoxide production, whereas the opposite is seen in old mice. Disruption of complex I assembly reduces oxidative metabolism with concomitant increase in mitochondrial superoxide production. This is rescued by knockdown of the mitochondrial chaperone, prohibitin. Disrupted complex I assembly causes premature senescence in primary cells. We propose that lower abundance of free catalytic complex I components supports complex I assembly, efficacy of substrate utilization and minimal ROS production, enabling enhanced longevity. 1 Institute for Ageing and Health, Newcastle University, Newcastle upon Tyne NE4 5PL, UK. 2 Centre for Integrated Systems Biology of Ageing and Nutrition, Newcastle University, Newcastle upon Tyne NE4 5PL, UK. 3 Newcastle University Protein and Proteome Analysis, Devonshire Building, Devonshire Terrace, Newcastle upon Tyne NE1 7RU, UK. Correspondence and requests for materials should be addressed to T.v.Z. -

Structural Bases of the Altered Catalytic Properties of a Pathogenic Variant of Apoptosis Inducing Factor
Structural bases of the altered catalytic properties of a pathogenic variant of apoptosis inducing factor Luca Sorrentinoa, b , Federica Cossua, b , Mario Milania, b, Alessandro Alivertib *, Eloise Mastrangeloa, b ** aBiophysics Institute, National Research Council c/o Department of Biosciences, Università degli Studi di Milano, Via Celoria 26, 20133 Milano, Italy; bDepartment of Biosciences, Università degli Studi di Milano, via Celoria 26, 20133 Milano, Italy. LS and FC contributed equally to this work. * To whom correspondence should be addressed: Phone: +39 0250314897. Fax: +39 0250314895. E-mail: [email protected] ** To whom correspondence should be addressed: Phone: +39 0250314898. Fax: +39 0250314895. E-mail: [email protected] 1 Abbreviations AIFCT, AIF forms in CT complex with NAD+; AIFOX, AIF forms harboring oxidized FAD; CHCHD4, coiled-coil-helix-coiled-coil-helix domain-containing protein 4; CT, charge transfer; DCIP, 2,6-dichlorophenolindophenol; FADH-, anionic dihydroquinone form of FAD; OXPHOS, oxidative phosphorylation. 2 Abstract The apoptosis-inducing factor (AIF) is a FAD-containing protein playing critical roles in caspase-independent apoptosis and mitochondrial respiratory chain biogenesis and maintenance. While its lethal role is well known, the details of its mitochondrial function remain elusive. So far, nineteen allelic variants of AIF have been associated to human diseases, mainly affecting the nervous system. A strict correlation is emerging between the degree of impairment of its ability to stabilize the charge- transfer (CT) complex between FAD and NAD+ and the severity of the resulting pathology. Recently, we demonstrated that the G307E replacement in murine AIF (equivalent to the pathogenic G308E in the human protein) dramatically decreases the rate of CT complex formation through the destabilization of the flavoprotein interaction with NAD(H). -

Mir-17-92 Fine-Tunes MYC Expression and Function to Ensure
ARTICLE Received 31 Mar 2015 | Accepted 22 Sep 2015 | Published 10 Nov 2015 DOI: 10.1038/ncomms9725 OPEN miR-17-92 fine-tunes MYC expression and function to ensure optimal B cell lymphoma growth Marija Mihailovich1, Michael Bremang1, Valeria Spadotto1, Daniele Musiani1, Elena Vitale1, Gabriele Varano2,w, Federico Zambelli3, Francesco M. Mancuso1,w, David A. Cairns1,w, Giulio Pavesi3, Stefano Casola2 & Tiziana Bonaldi1 The synergism between c-MYC and miR-17-19b, a truncated version of the miR-17-92 cluster, is well-documented during tumor initiation. However, little is known about miR-17-19b function in established cancers. Here we investigate the role of miR-17-19b in c-MYC-driven lymphomas by integrating SILAC-based quantitative proteomics, transcriptomics and 30 untranslated region (UTR) analysis upon miR-17-19b overexpression. We identify over one hundred miR-17-19b targets, of which 40% are co-regulated by c-MYC. Downregulation of a new miR-17/20 target, checkpoint kinase 2 (Chek2), increases the recruitment of HuR to c- MYC transcripts, resulting in the inhibition of c-MYC translation and thus interfering with in vivo tumor growth. Hence, in established lymphomas, miR-17-19b fine-tunes c-MYC activity through a tight control of its function and expression, ultimately ensuring cancer cell homeostasis. Our data highlight the plasticity of miRNA function, reflecting changes in the mRNA landscape and 30 UTR shortening at different stages of tumorigenesis. 1 Department of Experimental Oncology, European Institute of Oncology, Via Adamello 16, Milan 20139, Italy. 2 Units of Genetics of B cells and lymphomas, IFOM, FIRC Institute of Molecular Oncology Foundation, Milan 20139, Italy. -
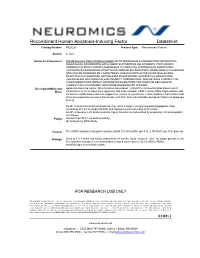
Recombinant Human Apoptosis-Inducing Factor Datasheet Catalog Number: PR27201 Product Type: Recombinant Protein
Recombinant Human Apoptosis-Inducing Factor Datasheet Catalog Number: PR27201 Product Type: Recombinant Protein Source: E. Coli Amino Acid Sequence: MGSSHHHHHH SSGLVPRGSH MGSEFLGLTP EQKQKKAALS ASEGEEVPQD KAPSHVPFLL IGGGTAAFAA ARSIRARDPG ARVLIVSEDP ELPYMRPPLS KELWFSDDPN VTKTLRFKQW NGKERSIYFQ PPSFYVSAQD LPHIENGGVA VLTGKKVVQL DVRDNMVKLN DGSQITYEKC LIATGGTPRS LSAIDRAGAE VKSRTTLFRK IGDFRSLEKI SREVKSITII GGGFLGSELA CALGRKARAL GTEVIQLFPE KGNMGKILPE YLSNWTMEKV RREGVKVMPN AIVQSVGVSS GKLLIKLKDG RKVETDHIVA AVGLEPNVEL AKTGGLEIDS DFGGFRVNAE LQARSNIWVA GDAACFYDIK LGRRRVEHHD HAVVSGRLAG ENMTGAAKPY WHQSMFWSDL GPDVGYEAIG LVDSSLPTVG VFAKATAQDN PKSATEQSGT GIRSESETES EASEITIPPS TPAVPQAPVQ GEDYGKGVIF YLRDKVVVGI VLWNIFNRMP IARKIIKDGE QHEDLNEVAK LFNIHED. Description/Molecular Apoptosis-Inducing Factor, Mitochondrion-Associated, 1 (AIFM1) is a mitochondrial protein which Mass: translocates to the nucleus once apoptosis has been initiated. AIFM1 causes DNA fragmentation and chromatin condensation and also triggers the release of cytochrome c and caspase-9 from mitochondria. Bcl-2 overexpression prevents the release of AIFM1 from mitochondria, but doesn’t block its apoptogenic activity. AIFM1 Human Recombinant produced in E.coli is a single, non-glycosylated polypeptide chain containing 537 amino acids (98-609) and having a molecular mass of 58.5 kDa. AIFM1 is fused to a 25 amino acid His-Tag at N-terminus and purified by proprietary chromatographic techniques. Purity: Greater than 95.0% as determined by: (a) Analysis by SDS-PAGE. Format: The AIFM1 solution (0.5mg/ml) contains 20mM Tris-HCl buffer (pH 8.0), 0.1M NaCl and 10% glycerol. Storage: Store at 4°C if entire vial will be used within 2-4 weeks. Store, frozen at -20°C for longer periods of time. For long term storage it is recommended to add a carrier protein (0.1% HSA or BSA). Avoid multiple freeze-thaw cycles. -

Mutations in Apoptosis-Inducing Factor Cause X-Linked Recessive Auditory
New loci J Med Genet: first published as 10.1136/jmedgenet-2014-102961 on 18 May 2015. Downloaded from ORIGINAL ARTICLE Mutations in apoptosis-inducing factor cause X-linked recessive auditory neuropathy spectrum disorder Liang Zong,1 Jing Guan,1 Megan Ealy,2,3 Qiujing Zhang,1 Dayong Wang,1 Hongyang Wang,1 Yali Zhao,1,4 Zhirong Shen,5 Colleen A Campbell,2 Fengchao Wang,5 Ju Yang,1 Wei Sun,6 Lan Lan,1 Dalian Ding,6 Linyi Xie,1 Yue Qi,1 Xin Lou,7 Xusheng Huang,8 Qiang Shi,8 Suhua Chang,9 Wenping Xiong,1 Zifang Yin,1 Ning Yu,1 Hui Zhao,1 Jun Wang,10 Jing Wang,9 Richard J Salvi,6 Christine Petit,11 Richard J H Smith,2 Qiuju Wang1 ▸ Additional material is ABSTRACT from 0.5% to 15% among hearing-impaired published online only. To view Background Auditory neuropathy spectrum disorder patients, with an incidence of about 13% in chil- please visit the journal online 2–4 (http://dx.doi.org/10.1136/ (ANSD) is a form of hearing loss in which auditory signal dren with severe-to-profound hearing loss. jmedgenet-2014-102961). transmission from the inner ear to the auditory nerve Consistent with physiological tests of auditory and brain stem is distorted, giving rise to speech function, ANSD can be caused by lesions of the perception difficulties beyond that expected for the IHC, IHC–auditory nerve synapse, auditory nerve fi – For numbered af liations see observed degree of hearing loss. For many cases of or auditory cortex.5 7 end of article.