Deprescribing Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Efficacy of Treatments for Patients with Obsessive-Compulsive Disorder: a Systematic Review
REVIEW Efficacy of treatments for patients with obsessive-compulsive disorder: A systematic review Yun-Jung Choi, PhD, RN, PMHNP (Lecturer) Keywords Abstract Systematic review; obsessive-compulsive disorder; efficacy of medication. Purpose: This systematic review examines the efficacy of pharmacological therapy for obsessive-compulsive disorder (OCD), addressing two major issues: Correspondence which treatment is most effective in treating the patient’s symptoms and which Yun-Jung Choi, PhD, RN, PMHNP, Red Cross is beneficial for maintaining remission. College of Nursing, 98 Saemoonan-Gil, Data sources: Seven databases were used to acquire articles. The key words Jongno-Gu, Seoul 110-102, Korea; used to search for the relative topics published from 1996 to 2007 were Tel: +82-2-3700-3676; fax: +82-2-3700-3400; ‘‘obsessive-compulsive disorder’’ and ‘‘Yale-Brown obsession-compulsion E-mail: [email protected] scale.’’ Based on the inclusion and exclusion criteria, 25 studies were selected Received: August 2007; from 57 potentially relevant studies. accepted: March 2008 Conclusions: The effects of treatment with clomipramine and selective sero- tonin reuptake inhibitors (SSRIs: fluvoxamine, sertraline, fluoxetine, citalo- doi:10.1111/j.1745-7599.2009.00408.x pram, and escitalopram) proved to be similar, except for the lower adherence rate in case of clomipramine because of its side effects. An adequate drug trial involves administering an effective daily dose for a minimum of 8 weeks. An augmentation strategy proven effective for individuals refractory to monother- apy with SSRI treatment alone is the use of atypical antipsychotics (risperidone, olanzapine, and quetiapine). Implications for practice: Administration of fluvoxamine or sertraline to patients for an adequate duration is recommended as the first-line prescription for OCD, and augmentation therapy with risperidone, olanzapine, or quetiapine is recommended for refractory OCD. -

Cipramil® 20 Mg Film-Coated Tablets
NEW ZEALAND DATA SHEET 1 NAME OF THE MEDICINE Cipramil® 20 mg Film-coated Tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Cipramil 20 mg Film-coated tablets contain 24.98 mg citalopram hydrobromide, corresponding to 20 mg citalopram base. Excipients with known effect: lactose For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM Cipramil tablets are oval, white, film-coated tablets, 8 mm × 5.5 mm, marked “C” and “N” symmetrically around the score-line. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Treatment of depressive illness in the initial phase and as maintenance against potential relapse/ recurrence. 4.2 Dose and method of administration The dose may be taken in the morning or evening without regard for food. As the treatment result in general can be evaluated only after 2-3 weeks’ treatment, a possible dose increase in increments of 10 mg should take place with intervals of 2-3 weeks. Adults Cipramil should be administered as a single oral dose of 20 mg daily. Dependent on individual patient response and severity of depression the dose may be increased to a maximum of 40 mg daily. The maximum daily dose should not be exceeded as doses above 40mg/day are associated with an increased risk of QT prolongation. Elderly patients The starting dose is 10mg/day. The dose can be increased by 10mg to a maximum of 20mg/day. Use in children and adolescents (under 18 years of age) Safety and efficacy have not been established in this population. Consequently, citalopram should not be used in children and adolescents under 18 years of age (see Section 4.4 Special warnings and precautions or use). -

Sertraline and Venlafaxine-Induced Nocturnal Enuresis
Case Report DOI: 10.5455/bcp.20140304091103 Sertraline and Venlafaxine-Induced Nocturnal Enuresis Inci Meltem Atay1, Gulin Ozdamar Unal2 ABS TRACT: Sertraline and venlafaxine-induced nocturnal enuresis Nocturnal enuresis is defined as the involuntary discharge of urine after the age of expected continence that occurs during sleep at night. Although there are a few reports in adults for nocturnal enuresis associated 1Assist. Prof., 2M.D., Suleyman Demirel University, School of Medicine, Department with serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs), the of Psychiatry, Isparta - Turkey mechanism or frequency of this side effect have not been identified yet. We report here a case of nocturnal Corresponding author: Dr. İnci Meltem Atay enuresis associated with both sertraline and venlafaxine in different major depressive episodes in an adult Süleyman Demirel Universitesi, Tıp Fakültesi, Psikiyatri Anabilim Dalı, Isparta - Türkiye patient that resolves after the discontinuation of the medications and continuation with escitalopram. To our E-ma il add ress: knowledge, in literature there have been no reports about nocturnal enuresis caused by those two agents in [email protected] the same patient. This case is discussed in detail for the recurrence of nocturnal enuresis, the importance of Date of submission: detailed assessment of even rare side effects and for their possible mechanisms. February 11, 2014 Date of acceptance: March 04, 2014 Keywords: nocturnal enuresis, venlafaxine, sertraline, depression Declaration of interest: I.M.A, G.O.U.: The authors reported no Klinik Psikofarmakoloji Bulteni - Bulletin of Clinical Psychopharmacology 2015;25(3):287-90 conflict of interest related to this article. INTRODUCTION side effect1-6. -
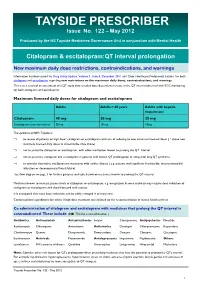
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -

(12) United States Patent (10) Patent No.: US 7,893,053 B2 Seed Et Al
US0078.93053B2 (12) United States Patent (10) Patent No.: US 7,893,053 B2 Seed et al. (45) Date of Patent: Feb. 22, 2011 (54) TREATING PSYCHOLOGICAL CONDITIONS WO WO 2006/127418 11, 2006 USING MUSCARINIC RECEPTORM ANTAGONSTS (75) Inventors: Brian Seed, Boston, MA (US); Jordan OTHER PUBLICATIONS Mechanic, Sunnyvale, CA (US) Chau et al. (Nucleus accumbens muscarinic receptors in the control of behavioral depression : Antidepressant-like effects of local M1 (73) Assignee: Theracos, Inc., Sunnyvale, CA (US) antagonist in the porSolt Swim test Neuroscience vol. 104, No. 3, pp. 791-798, 2001).* (*) Notice: Subject to any disclaimer, the term of this Lind et al. (Muscarinic acetylcholine receptor antagonists inhibit patent is extended or adjusted under 35 chick Scleral chondrocytes Investigative Ophthalmology & Visual U.S.C. 154(b) by 726 days. Science, vol.39, 2217-2231.* Chau D., et al., “Nucleus Accumbens Muscarinic Receptors in the (21) Appl. No.: 11/763,145 Control of Behavioral Depression: Antidepressant-like Effects of Local M1 Antagonists in the Porsolt Swin Test.” Neuroscience, vol. (22) Filed: Jun. 14, 2007 104, No. 3, Jun. 14, 2001, pp. 791-798. Bechtel, W.D., et al., “Biochemical pharmacology of pirenzepine. (65) Prior Publication Data Similarities with tricyclic antidepressants in antimuscarinic effects only.” Arzneimittelforschung, vol. 36(5), pp. 793-796 (May 1986). US 2007/O293480 A1 Dec. 20, 2007 Chau, D.T. et al., “Nucleus accumbens muscarinic receptors in the control of behavioral depression: antidepressant-like effects of local Related U.S. Application Data Mantagonist in the Porsolt Swim test.” Neuroscience, vol. 104(3), (60) Provisional application No. -

Impact of Citalopram and Fluvoxamine on Platelet Response To
S24_5 Impact of Citalopram and Fluvoxamine on Platelet Response to Clopidogrel, a Randomized, Double-blind, Crossover Trial Bruria Hirsh Racch1, Galia Spectre2, Ella Shai2, Amit Ritter3, David Varon2, Ronny Alcalai3 1School of Pharmacy, Hadassah Hebrew University Medical Center, Israel 2Coagulation Unit, Hematology, Hadassah Hebrew University Medical Center, Israel 3Heart Institute, Hadassah Hebrew University Medical Center, Israel Background: Selective serotonin reuptake inhibitors (SSRI) are widely used antidepressant agents. Studies have shown that use of SSRI in combination with aspirin or warfarin is associated with an increased risk bleeding, while little information is known about the interaction of SSRIs and clopidogrel. Fluvoxamine and citalopram are both SSRIs and while fluvoxamine is an inhibitor of CYP2C19 and thus might reduce the efficacy of clopidogrel, the effect of citalopram on liver metabolism is unknown. Aim: The aim was to assess the effect these two different SSRIs on platelet aggregation and on the laboratory response to clopidogrel. Methods: A randomized, double-blind, crossover study in 15 healthy volunteers comparing the antiplatelet effect of clopidogrel with and without fluvoxamine or citalopram .The response to clopidogrel was assessed by Light Transmittance Aggregometry with10µmol/L ADP and by vasodilator-stimulated phosphoprotein (VASP) phosphorylation, a measure of P2Y12 receptor reactivity. Results: Mean baseline platelet aggregation was 80.1%±3.4 and reduced to 23.5% after treatment with clopidogrel. Both fluvoxamine and citalopram had modest effect on platelet reactivity (65.8%±6.4, p=0.06 vs. baseline and 67.3%±6.3, p=0.07 vs. baseline respectively). Laboratory response to clopidogrel was significantly better in the presence of citalopram as compared to fluvoxamine both in aggregometry (23.4%±3 vs. -

Adverse Effects of First-Line Pharmacologic Treatments of Major Depression in Older Adults
Draft Comparative Effectiveness Review Number xx Adverse Effects of First-line Pharmacologic Treatments of Major Depression in Older Adults Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov This information is distributed solely for the purposes of predissemination peer review. It has not been formally disseminated by the Agency for Healthcare Research and Quality. The findings are subject to change based on the literature identified in the interim and peer-review/public comments and should not be referenced as definitive. It does not represent and should not be construed to represent an Agency for Healthcare Research and Quality or Department of Health and Human Services (AHRQ) determination or policy. Contract No. 290-2015-00012I Prepared by: Will be included in the final report Investigators: Will be included in the final report AHRQ Publication No. xx-EHCxxx <Month, Year> ii Purpose of the Review To assess adverse events of first-line antidepressants in the treatment of major depressive disorder in adults 65 years or older. Key Messages • Acute treatment (<12 weeks) with o Serotonin norepinephrine reuptake inhibitors (SNRIs) (duloxetine, venlafaxine), but not selective serotonin reuptake inhibitors (SSRIs) (escitalopram, fluoxetine) led to a greater number of adverse events compared with placebo. o SSRIs (citalopram, escitalopram and fluoxetine) and SNRIs (duloxetine and venlafaxine) led to a greater number of patients withdrawing from studies due to adverse events compared with placebo o Details of the contributing adverse events in RCTs were rarely reported to more clearly characterize what adverse events to expect. -

Geriatric Psychopharmacology: Anti-Depressants Amber Mackey, D.O
Geriatric Psychopharmacology: Anti-depressants Amber Mackey, D.O. University of Reno School of Medicine Department of Psychiatry Chief Resident, PGY-4 Pharmacologic issues in the elderly More likely to experience drug induced adverse events Cardiac effects: Prolonged QTc, arrhythmias, sudden death Peripheral/central anticholinergic effects: constipation, delirium, urinary retention, delirium, and cognitive dysfunction Antihistaminergic effects: sedation Antiadrenergic effects: postural hypotension Other effects: Hyponatremia, bleeding, altered bone metabolism Pharmacokinetic Organ system Change consequence Circulatory system Decreased concentration Increased or decreased of plasma albumin and free concentration of drugs increased α1-acid in plasma glycoprotein Gastrointestinal Table tract 20-1 Decreased intestinal and Decreased rate of drug splanchnic blood flow absorption Kidney Decreased glomerular Decreased renal filtration rate clearance of active metabolites Liver Decreased liver size; Decreased hepatic decreased hepatic blood clearance flow; variable effects on cytochrome P450 isozyme activity Muscle Decreased lean body mass Altered volume of and increased adipose distribution of lipid-soluble tissue drugs, leading to increased elimination half-life Table 20-1, Physiological changes in elderly persons associated with altered pharmacokinetics, American Psychiatric Publishing Textbook of Geriatric Psychiatry, Fifth Edition, Chapter 20: Psychopharmacology. Other issues Illnesses that effect the elderly also play a role in diminishing -

New Antidepressants and the Treatment of Depression Barry H
Technology Review New Antidepressants and the Treatment of Depression Barry H. Guze, MD, and Michael Gitlin, MD Los Angeles, California Depression is a common and significant health problem antidepressant drugs, the new agents are generally safer associated with impairment in a patient’s ability to than traditional medications used to treat depression: function. The development of new antidepressant med they are well tolerated and, in case of overdose, less ications represents progress in its treatment. These new harmful than tricyclic antidepressants. agents work through the selective blockade of the re uptake of serotonin into the presynaptic neuron, thereby increasing the availability of this neurotrans Key words. Serotonin antagonists; antidepressants; de mitter at the synaptic cleft and enhancing its effective pression; antidepressive agents, tricyclic. ness. While no more effective than traditional tricyclic ( / Fam Pratt 1994; 38:49-57) Depression is a common condition.1 Among the nonin- probability of relapse include the severity of the initial stitutionalized elderly, the prevalence of clinically signif episode, the number of prior episodes, the response to icant depression is about 15%.2 With a lifetime preva prior treatment, and a history of chronic depression.10 lence of 6% and associated risks such as suicide, major Other important factors include comorbid conditions, depression is an important public health concern in the such as chronic medical conditions, and the degree of United States.3 In 1979 and still in 1989, suicide was the psychosocial perturbation. Because recurrence is so com fourth leading cause of death for white Americans.4 mon, early and aggressive treatment of depression has The economic impact of depression in the United been recommended.12 States has been estimated at more than $16 billion, only Depression is usually treated by primary care physi S2.1 billion of which is spent on diagnosis and treat cians. -

Prescribing Guidance for Citalopram and Escitalopram Hull and East Riding Prescribing Committee
Prescribing Guidance for Citalopram and Escitalopram Hull and East Riding Prescribing Committee Summary of Safety Alert (December 2011) – http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON137769 Citalopram and escitalopram are associated with dose-dependent QT interval prolongation and should not be used in those with: congenital long QT syndrome; known pre-existing QT interval prolongation; or in combination with other medicines that prolong the QT interval. ECG measurements should be considered for patients with cardiac disease, and electrolyte disturbances should be corrected before starting treatment. For citalopram, new restrictions on the maximum daily doses now apply: 40 mg for adults; 20 mg for patients older than 65 years; and 20 mg for those with hepatic impairment. For escitalopram, the maximum daily dose for patients older than 65 years is now reduced to 10 mg/day; other doses remain unchanged. Recommended actions for prescribers If dose is above maximum recommended dose or patient is taking other medications likely to prolong QTc: Need for more than 1. Discuss with service user/patient. citalopram 40mg daily 2. Consider continued need for citalopram and/or alternative therapies (adults), 20mg daily (elderly and reduced hepatic function) e.g. for OCD, PTSD Adult citalopram Elderly (or other risk factors) Taking ANY other medicines Elderly and escitalopram dose above citalopram dose above likely to cause QTc dose above 10mg daily: prolongation 40mg daily: 20mg daily: Consider risk/benefit with service user. Switch if 1-Consider switching relevant possible medication to alternative with no Monitor If under 18 refer to CAMHS effect on QTc prolongation or Reduce dose stepwise to 40mg citalopram daily for adults (unlicensed use). -

Mid Essex CCG 'Guidance for the Treatment of Depression in Adults'
Guidance for the treatment of depression in adults MILD DEPRESSION - Medication is not first-line treatment or only treatment for depression Actively monitor symptoms, give life style advice, guided self- help or exercise MODERATE DEPRESSION Consider psychological intervention. This is accessed by referral or self-referral to Mid Essex IAPT (Improving Access to Psychological Therapies) and include Cognitive Behavioural Therapy (CBT) or Interpersonal Therapy (IPT) Ask about OTC/Herbal/St John’s Wort use – NO SSRI to be prescribed if already on St John’s Wort or stop St John’s Wort Consider referral to specialist care early if the patient has significant suicidal ideation, severe depression, depression in bipolar disorder. MODERATE to SEVERE DEPRESSION Discuss medication and treatment options with patient before prescribing, include side effects and risk of suicidal thoughts during onset of treatment. Consider patients co-morbidities when selecting antidepressant and ask about OTC/Herbal/St John’s Wort as described above. Refer to IAPT - Psychological therapies should be continued alongside medication. Ensure adequate duration of treatment has been tried before switching medication or increasing dose. CITALOPRAM 20mg daily or SERTRALINE 50mg daily Citalopram – consider Dose 10mg for 10days then Assess efficacy over 6-8 weeks. If effective see box 1 titration 20mg for 6-8 weeks Ineffective Sertraline – consider Poorly 25mg for 10days then tolerated 50mg for 6-8 weeks Increase to: Citalopram 30mg OD, Switch to fluoxetine or increase to 40mg after 6 line another SSRI or Mirtazapine. st weeks if required (MAX dose 1 Cross-taper when switching. Box 1. in elderly = 20mg) Increase to therapeutic dose. -

About Your Medication SERTRALINE
About your medication SERTRALINE (ZOLOFT® 50mg, 100mg tablets) Other brands may be available WHAT IS SERTRALINE? Sertraline is from a group of anti-depressant medications known as serotonin re- uptake inhibitors (SSRIs). It is only available on a doctor’s prescription. WHAT IS IT FOR? Sertraline is mainly used in adults to treat severe emotional problems that interfere with normal life. These problems can include severe forms of depression, anxiety, and obsessive compulsive disorder. In children and adolescents, there is less experience in treating severe emotional problems with sertraline. Most experience is in treating obsessive compulsive disorder. The use of sertraline to treat a child or adolescent with severe emotional problems should occur with caution and be part of a comprehensive treatment plan that includes non-medication treatments. Specialists such as Child Psychiatrists and Developmental Paediatricians should supervise treatment with these medicines. HOW TO TAKE THIS MEDICINE It is important that this medicine is given only as directed and not given to other people. Treatment starts with a low dose and is adjusted by your doctor according to the response. Most anti-depressant medications take time to work so don't be discouraged if the sertraline seems not to be working immediately. It may take two to four weeks or even longer to feel the full benefit of sertraline. Sertraline can be taken with food or on an empty stomach. It is best to give the medicine in the morning. If two doses a day are required, it is best given in the morning and the early afternoon. WHAT TO DO IF A DOSE IS MISSED If your child misses a dose of the medication it can be given as soon as you remember.