When Body Art Goes Bad
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rockhounds Herald
The official bulletin of the Dothan Gem & Mineral Club, Inc. Rockhounds Herald 920 Yorktown Road, Dothan, AL 36301-4372 www.wiregrassrockhounds.com April 2012 Words from… The President No meeting this month since our gem and mineral show is scheduled for Saturday and Sunday, April 21 – 22. A lot of online calendars and other media sources have picked up the show announcement so we are expecting a really big turnout this year. Try to come at least one day, if you can…and bring your family and friends! If you are supplying door prizes for the show and have not yet given them to John Webber, please bring them directly to the show. Thanks. JoAn Announcements Jewelry Workshop – JoAn Lambert will be hosting a Frangipani Caterpillar Bracelet workshop at 1:00 PM on Saturday, April 28 at the fellowship hall. She will be bringing the printed patterns, but you’ll need to bring your own supplies. The following list of supplies will make one 7 ½ bracelet: 60 4mm faceted beads Size 12 beading needle Size 11 seed beads Size D beading thread or silamide Size 14 seed beads or charlottes Scissors ½” clasp bead or button Beeswax or Thread Heaven Note: If you’d like a longer bracelet, you’ll need to buy extra 4mm beads. The seed beads can be the same color as the 4mm beads or you can use gold or silver. Upcoming Shows April 21 – 22 Dothan Gem & Mineral Show Dothan, AL April 28 – 29 Memphis Mineral, Fossil, Jewelry Show Memphis, TN May 11 – 13 Georgia Mineral Society Show Marietta, GA Source: www.amfed.org/sfms/ Meeting3380688 Minutes – March 2012 – by Secretary The meeting was called to order by club President, JoAn Lambert, at 2:03 PM. -

Malachite Cu2(CO3)(OH)2 C 2001-2005 Mineral Data Publishing, Version 1
Malachite Cu2(CO3)(OH)2 c 2001-2005 Mineral Data Publishing, version 1 Crystal Data: Monoclinic. Point Group: 2/m. Crystals are acicular to prismatic, thick tabular, equant, with {100}, {010}, {001}, {110}, {201}, several other forms, rounded, in sprays and crude composite aggregates, to 9 cm; typically stalactitic, mammillary, botryoidal, as such, radially fibrous internally. Twinning: On {100}, {201}, very common as contact or penetration twins, also polysynthetic. Physical Properties: Cleavage: Perfect on {201}; fair on {010}. Fracture: Subconchoidal to uneven. Hardness = 3.5–4 D(meas.) = 4.05(2) D(calc.) = 3.983 Optical Properties: Translucent to opaque. Color: Bright green, dark green, blackish green, commonly banded in masses; green to yellowish green in transmitted light. Streak: Pale green. Luster: Adamantine to vitreous; silky if fibrous; dull to earthy if massive. Optical Class: Biaxial (–). Pleochroism: X = nearly colorless; Y = yellowish green; Z = deep green. Orientation: Y = b; X ∧ c = 23.5◦. Dispersion: r<v,moderately strong. α = 1.655(3) β = 1.875(3) γ = 1.909(3) 2V(meas.) = 43(2)◦ ◦ 0 Cell Data: Space Group: P 21/a. a = 9.502 b = 11.974 c = 3.240 β =98 45 Z=4 X-ray Powder Pattern: Synthetic. 2.857 (100), 3.693 (85), 5.055 (75), 5.993 (55), 2.520 (55), 2.778 (45), 2.464 (35) Chemistry: (1) (2) CO2 20.04 19.90 CuO 72.03 71.95 H2O 8.09 8.15 Total 100.16 100.00 (1) Rio Marina, Elba, Italy. (2) Cu2(CO3)(OH)2. Occurrence: A common secondary mineral formed in the oxidation zone of copper deposits; locally may be an ore of copper. -
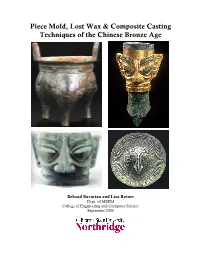
Piece Mold, Lost Wax & Composite Casting Techniques of The
Piece Mold, Lost Wax & Composite Casting Techniques of the Chinese Bronze Age Behzad Bavarian and Lisa Reiner Dept. of MSEM College of Engineering and Computer Science September 2006 Table of Contents Abstract Approximate timeline 1 Introduction 2 Bronze Transition from Clay 4 Elemental Analysis of Bronze Alloys 4 Melting Temperature 7 Casting Methods 8 Casting Molds 14 Casting Flaws 21 Lost Wax Method 25 Sanxingdui 28 Environmental Effects on Surface Appearance 32 Conclusion 35 References 36 China can claim a history rich in over 5,000 years of artistic, philosophical and political advancement. As well, it is birthplace to one of the world's oldest and most complex civilizations. By 1100 BC, a high level of artistic and technical skill in bronze casting had been achieved by the Chinese. Bronze artifacts initially were copies of clay objects, but soon evolved into shapes invoking bronze material characteristics. Essentially, the bronze alloys represented in the copper-tin-lead ternary diagram are not easily hot or cold worked and are difficult to shape by hammering, the most common techniques used by the ancient Europeans and Middle Easterners. This did not deter the Chinese, however, for they had demonstrated technical proficiency with hard, thin walled ceramics by the end of the Neolithic period and were able to use these skills to develop a most unusual casting method called the piece mold process. Advances in ceramic technology played an influential role in the progress of Chinese bronze casting where the piece mold process was more of a technological extension than a distinct innovation. Certainly, the long and specialized experience in handling clay was required to form the delicate inscriptions, to properly fit the molds together and to prevent them from cracking during the pour. -

Jackson's Auction
Jackson's Auction Collector's Choice: Antiques & Collectibles Wednesday - September 19, 2012 Collector's Choice: Antiques & Collectibles 675: REED & BARTON STERLING SILVER FLATWARE, 148 PIECES USD 4,000 - 6,000 A LARGE 148 PIECE SET OF REED AND BARTON FRANCIS 1ST STERLING SILVER FLATWARE, MID 20TH CENTURY. Comprising 24 table knives, 24 table forks, 24 salad forks, 35 teaspoons, 13 cream soup spoons, 5 tablespoons, 12 individual butter knives and 11 various serving pieces. Contained in two fitted chests, not matching. Total weight approximately 194 troy oz. 676: DUTCH SILVER EPERGNE, 1853 USD 1,000 - 1,500 A VERY FINE DUTCH SILVER AND CUT CRYSTAL CENTERPIECE EPERGNE, 1853. Stamp hallmarks including "Z&B" probably for Pieter Zollner and William Beijoer (1849-1871) comprising a silver entwining stem with extending foliage supporting two scallop cut crystal trays below a tulip blossom finial raised on a scalloped floral repousse and chased bell form base. Additionally stamped "Pde Meyer te'Hage." Silver weight approximately 34.76 troy oz. Height 22.5 inches (57cm). 677: WALLACE ROSE POINT STERLING SILVER FLATWARE, 63 PIECES USD 1,200 - 1,800 A VERY FINE SET OF WALLACE ROSE POINT STERLING SILVER FLATWARE, MID 20TH CENTURY. 63 pieces comprising 10 each place knives, place forks and salad forks, 20 teaspoons, 10 individual butters, a gravy ladle, sugar shell and pastry server. All contained in a fitted mahogany chest with drawer. Weight approximately 60 troy oz. 678: A FINE CONTINENTAL SILVER BACCHANALIAN FOOTED BOWL USD 200 - 400 A FINE CONTINENTAL SILVER BACCHANALIAN FOOTED BOWL, 20TH CENTURY. With embossed and chased facial mask within hammered scalloped lobes and grape vine rim in deep relief. -
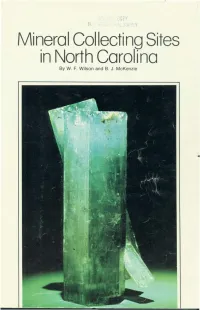
Mineral Collecting Sites in North Carolina by W
.'.' .., Mineral Collecting Sites in North Carolina By W. F. Wilson and B. J. McKenzie RUTILE GUMMITE IN GARNET RUBY CORUNDUM GOLD TORBERNITE GARNET IN MICA ANATASE RUTILE AJTUNITE AND TORBERNITE THULITE AND PYRITE MONAZITE EMERALD CUPRITE SMOKY QUARTZ ZIRCON TORBERNITE ~/ UBRAR'l USE ONLV ,~O NOT REMOVE. fROM LIBRARY N. C. GEOLOGICAL SUHVEY Information Circular 24 Mineral Collecting Sites in North Carolina By W. F. Wilson and B. J. McKenzie Raleigh 1978 Second Printing 1980. Additional copies of this publication may be obtained from: North CarOlina Department of Natural Resources and Community Development Geological Survey Section P. O. Box 27687 ~ Raleigh. N. C. 27611 1823 --~- GEOLOGICAL SURVEY SECTION The Geological Survey Section shall, by law"...make such exami nation, survey, and mapping of the geology, mineralogy, and topo graphy of the state, including their industrial and economic utilization as it may consider necessary." In carrying out its duties under this law, the section promotes the wise conservation and use of mineral resources by industry, commerce, agriculture, and other governmental agencies for the general welfare of the citizens of North Carolina. The Section conducts a number of basic and applied research projects in environmental resource planning, mineral resource explora tion, mineral statistics, and systematic geologic mapping. Services constitute a major portion ofthe Sections's activities and include identi fying rock and mineral samples submitted by the citizens of the state and providing consulting services and specially prepared reports to other agencies that require geological information. The Geological Survey Section publishes results of research in a series of Bulletins, Economic Papers, Information Circulars, Educa tional Series, Geologic Maps, and Special Publications. -

Gold Jewellery in Ptolemaic, Roman and Byzantine Egypt. Jack M
Gold Jewellery in Ptolemaic, Roman and Byzantine Egypt. Jack M. Ogden ABSTRACT This study deals with the gold jewellery made and worn in Egypt during the millennium between Alexander the Great's invasion of Egypt and the Arab conquest. Funerary jewellery is largely ignored as are ornaments in the traditional, older Egyptian styles. The work draws upon a wide variety of evidence, in particular the style, composition and construction of surviving jewellery, the many repre- sentations of jewellery in wear, such as funerary portraits, and the numerous literary references from the papyri and from Classical and early Christian writers. Egypt, during the period considered, has provided a greater wealth of such information than anywhere else in the ancient or medieval world and this allows a broadly based study of jewellery in a single ancient society. The individual chapters deal with a brief historical background; the information available from papyri and other literary sources; the sources, distribution, composition and value of gold; the origins and use of mineral and organic gem materials; the economic and social organisation of the goldsmiths' trade; and the individual jewellery types, their chronology, manufacture and significance. This last section is covered in four chapters which deal respectively with rings, earrings, necklets and pendants, and bracelets and armiets. These nine chapters are followed by a detailed bibliography and a list of the 511 illustrations. Gold Jewellery in Ptolemaic, Roman and Byzantine Egypt. In two volumes Volume 1 - Text. Jack M. Ogden Ph.D. Thesis Universtity of Durham, Department of Oriental Studies. © 1990 The copyright of this thesis rests with the author. -

Gemstones by Donald W
GEMSTONES By Donald W. olson Domestic survey data and tables were prepared by Nicholas A. Muniz, statistical assistant, and the world production table was prepared by Glenn J. Wallace, international data coordinator. In this report, the terms “gem” and “gemstone” mean any gemstones and on the cutting and polishing of large diamond mineral or organic material (such as amber, pearl, petrified wood, stones. Industry employment is estimated to range from 1,000 to and shell) used for personal adornment, display, or object of art ,500 workers (U.S. International Trade Commission, 1997, p. 1). because it possesses beauty, durability, and rarity. Of more than Most natural gemstone producers in the United states 4,000 mineral species, only about 100 possess all these attributes and are small businesses that are widely dispersed and operate are considered to be gemstones. Silicates other than quartz are the independently. the small producers probably have an average largest group of gemstones; oxides and quartz are the second largest of less than three employees, including those who only work (table 1). Gemstones are subdivided into diamond and colored part time. the number of gemstone mines operating from gemstones, which in this report designates all natural nondiamond year to year fluctuates because the uncertainty associated with gems. In addition, laboratory-created gemstones, cultured pearls, the discovery and marketing of gem-quality minerals makes and gemstone simulants are discussed but are treated separately it difficult to obtain financing for developing and sustaining from natural gemstones (table 2). Trade data in this report are economically viable deposits (U.S. -

Mineralogy of Non-Silicified Fossil Wood
Article Mineralogy of Non-Silicified Fossil Wood George E. Mustoe Geology Department, Western Washington University, Bellingham, WA 98225, USA; [email protected]; Tel: +1-360-650-3582 Received: 21 December 2017; Accepted: 27 February 2018; Published: 3 March 2018 Abstract: The best-known and most-studied petrified wood specimens are those that are mineralized with polymorphs of silica: opal-A, opal-C, chalcedony, and quartz. Less familiar are fossil woods preserved with non-silica minerals. This report reviews discoveries of woods mineralized with calcium carbonate, calcium phosphate, various iron and copper minerals, manganese oxide, fluorite, barite, natrolite, and smectite clay. Regardless of composition, the processes of mineralization involve the same factors: availability of dissolved elements, pH, Eh, and burial temperature. Permeability of the wood and anatomical features also plays important roles in determining mineralization. When precipitation occurs in several episodes, fossil wood may have complex mineralogy. Keywords: fossil wood; mineralogy; paleobotany; permineralization 1. Introduction Non-silica minerals that cause wood petrifaction include calcite, apatite, iron pyrites, siderite, hematite, manganese oxide, various copper minerals, fluorite, barite, natrolite, and the chromium- rich smectite clay mineral, volkonskoite. This report provides a broad overview of woods fossilized with these minerals, describing specimens from world-wide locations comprising a diverse variety of mineral assemblages. Data from previously-undescribed fossil woods are also presented. The result is a paper that has a somewhat unconventional format, being a combination of literature review and original research. In an attempt for clarity, the information is organized based on mineral composition, rather than in the format of a hypothesis-driven research report. -

Healing Gemstones for Everyday Use
GUIDE TO THE WORLD’S TOP 20 MOST EFFECTIVE HEALING GEMSTONES FOR EVERYDAY USE BY ISABELLE MORTON Guide to the World’s Top 20 Most Effective Healing Gemstones for Everyday Use Copyright © 2019 by Isabelle Morton Photography by Ryan Morton, Isabelle Morton Cover photo by Jeff Skeirik All rights reserved. Published by The Gemstone Therapy Institute P.O. Box 4065 Manchester, Connecticut 06045 U.S.A. www.GemstoneTherapyInstitute.org IMPORTANT NOTICE This book is designed to provide information for purposes of reference and guidance and to accompany, not replace, the services of a qualified health care practitioner or physician. It is not the intent of the author or publisher to prescribe any substance or method to cure, mitigate, treat, or prevent any disease. In the event that you use this information with or without seeking medical attention, the author and publisher shall not be liable or otherwise responsible for any loss, damage, or injury directly or indirectly caused by or arising out of the information contained herein. CONTENTS Gemstones for Physical Healing Light Green Aventurine 5 Dark Green Aventurine 11 Malachite 17 Tree Agate 23 Gemstones for Emotional Healing Rhodonite 30 Morganite 36 Pink Chalcedony 43 Rose Quartz 49 Gemstones for Healing Memory, Patterns, & Habits Opalite 56 Leopardskin Jasper 62 Golden Beryl 68 Rhodocrosite 74 Gemstones for Healing the Mental Body Sodalite 81 Blue Lace Agate 87 Lapis Lazuli 93 Lavender Quartz 99 Gemstones to Nourish Your Spirit Amethyst 106 Clear Quartz / Frosted Quartz 112 Mother of Pearl 118 Gemstones For Physical Healing LIGHT GREEN AVENTURINE DARK GREEN AVENTURINE MALACHITE TREE AGATE https://GemstoneTherapyInstitute.org LIGHT GREEN AVENTURINE 5 Copyright © 2019 Isabelle Morton. -
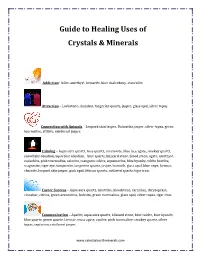
Guide to Healing Uses of Crystals & Minerals
Guide to Healing Uses of Crystals & Minerals Addiction- Iolite, amethyst, hematite, blue chalcedony, staurolite. Attraction – Lodestone, cinnabar, tangerine quartz, jasper, glass opal, silver topaz. Connection with Animals – Leopard skin Jasper, Dalmatian jasper, silver topaz, green tourmaline, stilbite, rainforest jasper. Calming – Aqua aura quartz, rose quartz, amazonite, blue lace agate, smokey quartz, snowflake obsidian, aqua blue obsidian, blue quartz, blizzard stone, blood stone, agate, amethyst, malachite, pink tourmaline, selenite, mangano calcite, aquamarine, blue kyanite, white howlite, magnesite, tiger eye, turquonite, tangerine quartz, jasper, bismuth, glass opal, blue onyx, larimar, charoite, leopard skin jasper, pink opal, lithium quartz, rutilated quartz, tiger iron. Career Success – Aqua aura quartz, ametrine, bloodstone, carnelian, chrysoprase, cinnabar, citrine, green aventurine, fuchsite, green tourmaline, glass opal, silver topaz, tiger iron. Communication – Apatite, aqua aura quartz, blizzard stone, blue calcite, blue kyanite, blue quartz, green quartz, larimar, moss agate, opalite, pink tourmaline, smokey quartz, silver topaz, septarian, rainforest jasper. www.celestialearthminerals.com Creativity – Ametrine, azurite, agatized coral, chiastolite, chrysocolla, black amethyst, carnelian, fluorite, green aventurine, fire agate, moonstone, celestite, black obsidian, sodalite, cat’s eye, larimar, rhodochrosite, magnesite, orange calcite, ruby, pink opal, blue chalcedony, abalone shell, silver topaz, green tourmaline, -

Vintage Jewellery & Accessories
Vintage Jewellery & Accessories Monday 20th July 2015 Vintage Jewellery & Accessories Monday 20th July 2015 at 10.00am For this sale we have managed to keep it to a much more acceptable We have some interesting Austro-Hungarian enamel pendants of Saints, number of lots, 1074, so this auction will run as normal, starting at 10am lot 317, a pendant depicting Saint Sebastian bound to a tree and shot and lasting most of the day. However I would like to make you aware with arrows. Also lot 318, a pendant designed as Saint George upon that we are reducing the amount of viewing days, please see dates and a white horse and holding his spear, suspending a second dragon times at the bottom of this page. pendant. As usual there is a great variety of pieces for you to bid on. Starting with There is an array of designer jewellery including Michaela Frey, Chanel, some interesting memorial rings, lot 2, a George II memorial ring for Tiffany & Co. and Georg Jensen, from lots 698 to 767. Sir Gilbert Heathcote who was the Governor of the Bank of England and Lord Mayor of London in the early 18th Century, also lot 26, a George III If designer names are your preference then the selection of designer Scottish enamel memorial ring for John Wetherall who was the Shire bags may also catch your eye, with some colourful Jimmy Choo bags, Commissioner for Dumfriesshire and a baronet in the early 18th century. lots 1009 and lot 1010, prefect for the summer. Also bags by Louis Vuitton and Gucci. -

GEMSTONES by Donald W
GEMSTONES By Donald W. Olson Domestic survey data and tables were prepared by Christine K. Pisut, statistical assistant, and the world production table was prepared by Glenn J. Wallace, international data coordinator. Gemstones have fascinated humans since prehistoric times. sustaining economically viable deposits (U.S. International They have been valued as treasured objects throughout history Trade Commission, 1997, p. 23). by all societies in all parts of the world. The first stones known The total value of natural gemstones produced in the United to have been used for making jewelry include amber, amethyst, States during 2001 was estimated to be at least $15.1 million coral, diamond, emerald, garnet, jade, jasper, lapis lazuli, pearl, (table 3). The production value was 12% less than the rock crystal, ruby, serpentine, and turquoise. These stones preceding year. The production decrease was mostly because served as status symbols for the wealthy. Today, gems are not the 2001 shell harvest was 13% less than in 2000. worn to demonstrate wealth as much as they are for pleasure or The estimate of 2001 U.S. gemstone production was based on in appreciation of their beauty (Schumann, 1998, p. 8). In this a survey of more than 200 domestic gemstone producers report, the terms “gem” and “gemstone” mean any mineral or conducted by the USGS. The survey provided a foundation for organic material (such as amber, pearl, and petrified wood) projecting the scope and level of domestic gemstone production used for personal adornment, display, or object of art because it during the year. However, the USGS survey did not represent possesses beauty, durability, and rarity.