Contents Appendix 1A: List of Exposure Drugs in Nsaids and Pneumonia Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparing the Effects of Salts of Diclofenac and Almioprofen with Aspirin on Serum Electrolytes, Creatinine and Urea Levels in Rabbits
Comparing the effects of salts of diclofenac and almioprofen with aspirin on serum electrolytes, creatinine and urea levels in rabbits Nawazish-i-Husain Syed*, Farnaz Zehra, Amir Ali Rizvi Syed, Sabiha Karim and Farrakh Zia Khan University College of Pharmacy, University of the Punjab, Lahore, Pakistan Abstract: The effects of diclofenac sodium, diclofenac potassium, alminoprofen and aspirin on serum electrolytes (serum Na+ and K+), urea and creatinine were compared in rabbits in acute and chronic phases of treatment. The data suggested that all the four drugs markedly increased the serum electrolytes, urea and creatinine levels in both post- treatment phases. In conclusion, present study does not present any advantage of diclofenac sodium over diclofenac potassium at electrolyte levels on short and long term treatment. Nevertheless, current data support the evidence of renal function impairment by all the four drug therapies used in the present study, which is generally caused by NSAIDS. Keywords: NSAIDs, renal function, serum electrolytes. INTRODUCTION were given fodder twice daily, while water was available ad libitum. Throughout the study, environmental Inflammatory diseases including rheumatoid arthritis and conditions remained constant. Rabbits were divided into osteoarthritis are initially treated with non-steroidal anti- five groups, each of six animals. Same group of animals inflammatory drugs (NSAIDS) (Patrono and Rocca, were used for acute and chronic phases of the study. In 2009). Previously, steroids were prescribed to manage the both studies, rabbits of each group were orally chronic inflammatory diseases, however, due to their administered diclofenac Na+, diclofenac K+, severe adverse effects, NSAIDS has become the first alminoprofen, acetyl salicylic acid in a doses of 2.5mg, choice to treat these diseases. -

Table S1: Sensitivity, Specificity, PPV, NPV, and F1 Score of NLP Vs. ICD for Identification of Symptoms for (A) Biome Developm
Table S1: Sensitivity, specificity, PPV, NPV, and F1 score of NLP vs. ICD for identification of symptoms for (A) BioMe development cohort; (B) BioMe validation cohort; (C) MIMIC-III; (D) 1 year of notes from patients in BioMe calculated using manual chart review. A) Fatigue Nausea and/or vomiting Anxiety Depression NLP (95% ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P CI) 0.99 (0.93- 0.59 (0.43- <0.00 0.25 (0.12- <0.00 <0.00 0.54 (0.33- Sensitivity 0.99 (0.9 – 1) 0.98 (0.88 -1) 0.3 (0.15-0.5) 0.85 (0.65-96) 0.02 1) 0.73) 1 0.42) 1 1 0.73) 0.57 (0.29- 0.9 (0.68- Specificity 0.89 (0.4-1) 0.75 (0.19-1) 0.68 0.97 (0.77-1) 0.03 0.98 (0.83-1) 0.22 0.81 (0.53-0.9) 0.96 (0.79-1) 0.06 0.82) 0.99) 0.99 (0.92- 0.86 (0.71- 0.94 (0.79- 0.79 (0.59- PPV 0.96 (0.82-1) 0.3 0.95 (0.66-1) 0.02 0.95 (0.66-1) 0.16 0.93 (0.68-1) 0.12 1) 0.95) 0.99) 0.92) 0.13 (0.03- <0.00 0.49 (0.33- <0.00 0.66 (0.48- NPV 0.89 (0.4-1) 0.007 0.94 (0.63-1) 0.34 (0.2-0.51) 0.97 (0.81-1) 0.86 (0.6-0.95) 0.04 0.35) 1 0.65) 1 0.81) <0.00 <0.00 <0.00 F1 Score 0.99 0.83 0.88 0.57 0.95 0.63 0.82 0.79 0.002 1 1 1 Itching Cramp Pain NLP (95% ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P CI) 0.98 (0.86- 0.24 (0.09- <0.00 0.09 (0.01- <0.00 0.52 (0.37- <0.00 Sensitivity 0.98 (0.85-1) 0.99 (0.93-1) 1) 0.45) 1 0.29) 1 0.66) 1 0.89 (0.72- 0.5 (0.37- Specificity 0.96 (0.8-1) 0.98 (0.86-1) 0.68 0.98 (0.88-1) 0.18 0.5 (0-1) 1 0.98) 0.66) 0.88 (0.69- PPV 0.96 (0.8-1) 0.8 (0.54-1) 0.32 0.8 (0.16-1) 0.22 0.99 (0.93-1) 0.98 (0.87-1) NA* 0.97) 0.98 (0.85- 0.57 (0.41- <0.00 0.58 (0.43- <0.00 NPV 0.98 (0.86-1) 0.5 (0-1) 0.02 (0-0.08) NA* 1) 0.72) 1 0.72) 1 <0.00 <0.00 <0.00 F1 Score 0.97 0.56 0.91 0.28 0.99 0.68 1 1 1 *Denotes 95% confidence intervals and P values that could not be calculated due to insufficient cells in 2x2 tables. -

Prescription Pattern of Primary Osteoarthritis in Tertiary Medical
Published online: 2020-04-21 Running title: Primary Osteoarthritis Nitte University Journal of Health Science Original Article Prescription Pattern of Primary Osteoarthritis in Tertiary Medical Centre Sowmya Sham Kanneppady1, Sham Kishor Kanneppady2, Vijaya Raghavan3, Aung Myo Oo4, Ohn Mar Lwin5 1Senior Lecturer and Head, Department of Pharmacology, Faculty of Medicine, Lincoln University College, Selangor Darul Ehsan, Malaysia, 2Senior Lecturer, School of Dentistry, International Medical University, Kuala Lumpur, Malaysia, 3Head of the Department of Pharmacology, KVG Medical College and Hospital, Kurunjibag, Sullia, Karnataka, India. 4Assistant Professor, Department of Biochemistry, Faculty of Medicine, Lincoln University College, Selangor Darul Ehsan, Malaysia, 5Post graduate student, Department of Physiology, Faculty of Medicine, University Malaya, Kuala Lumpur, Malaysia. *Corresponding Author : Sowmya Sham Kanneppady, Senior Lecturer and Head,Department of Pharmacology, Faculty of Medicine, Lincoln University College, No. 2, Jalan Stadium, SS 7/15, Kelana Jaya, 47301, Petaling Jaya, Selangor Darul Ehsan, Malaysia. E-mail : [email protected]. Received : 12.10.2017 Abstract Review Completed : 05.12.2017 Objectives: Osteoarthritis (OA) is one of the commonest joint/musculoskeletal disorders, Accepted : 06.12.2017 affecting the middle aged and elderly, although younger people may be affected as a result of injury or overuse. The study aimed to analyze the data, evaluate the prescription pattern and Keywords: Osteoarthritis, anti- rationality of the use of drugs in the treatment of primary OA with due emphasis on the inflammatory agents, prevalence available treatment regimens. Materials and methods: Medical case records of patients suffering from primary OA attending Access this article online the department of Orthopedics of a tertiary medical centre were the source of data. -

Health Reports for Mutual Recognition of Medical Prescriptions: State of Play
The information and views set out in this report are those of the author(s) and do not necessarily reflect the official opinion of the European Union. Neither the European Union institutions and bodies nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein. Executive Agency for Health and Consumers Health Reports for Mutual Recognition of Medical Prescriptions: State of Play 24 January 2012 Final Report Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Acknowledgements Matrix Insight Ltd would like to thank everyone who has contributed to this research. We are especially grateful to the following institutions for their support throughout the study: the Pharmaceutical Group of the European Union (PGEU) including their national member associations in Denmark, France, Germany, Greece, the Netherlands, Poland and the United Kingdom; the European Medical Association (EMANET); the Observatoire Social Européen (OSE); and The Netherlands Institute for Health Service Research (NIVEL). For questions about the report, please contact Dr Gabriele Birnberg ([email protected] ). Matrix Insight | 24 January 2012 2 Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Executive Summary This study has been carried out in the context of Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross- border healthcare (CBHC). The CBHC Directive stipulates that the European Commission shall adopt measures to facilitate the recognition of prescriptions issued in another Member State (Article 11). At the time of submission of this report, the European Commission was preparing an impact assessment with regards to these measures, designed to help implement Article 11. -
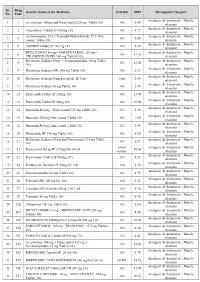
PMBJP Product.Pdf
Sr. Drug Generic Name of the Medicine Unit Size MRP Therapeutic Category No. Code Analgesic & Antipyretic / Muscle 1 1 Aceclofenac 100mg and Paracetamol 325 mg Tablet 10's 10's 8.00 relaxants Analgesic & Antipyretic / Muscle 2 2 Aceclofenac Tablets IP 100mg 10's 10's 4.37 relaxants Acetaminophen 325 + Tramadol Hydrochloride 37.5 film Analgesic & Antipyretic / Muscle 3 4 10's 8.00 coated Tablet 10's relaxants Analgesic & Antipyretic / Muscle 4 5 ASPIRIN Tablets IP 150 mg 14's 14's 2.70 relaxants DICLOFENAC 50 mg+ PARACETAMOL 325 mg+ Analgesic & Antipyretic / Muscle 5 6 10's 11.30 CHLORZOXAZONE 500 mg Tablets 10's relaxants Diclofenac Sodium 50mg + Serratiopeptidase 10mg Tablet Analgesic & Antipyretic / Muscle 6 8 10's 12.00 10's relaxants Analgesic & Antipyretic / Muscle 7 9 Diclofenac Sodium (SR) 100 mg Tablet 10's 10's 6.12 relaxants Analgesic & Antipyretic / Muscle 8 10 Diclofenac Sodium 25mg per ml Inj. IP 3 ml 3 ml 2.00 relaxants Analgesic & Antipyretic / Muscle 9 11 Diclofenac Sodium 50 mg Tablet 10's 10's 2.90 relaxants Analgesic & Antipyretic / Muscle 10 12 Etoricoxilb Tablets IP 120mg 10's 10's 33.00 relaxants Analgesic & Antipyretic / Muscle 11 13 Etoricoxilb Tablets IP 90mg 10's 10's 25.00 relaxants Analgesic & Antipyretic / Muscle 12 14 Ibuprofen 400 mg + Paracetamol 325 mg Tablet 10's 15's 5.50 relaxants Analgesic & Antipyretic / Muscle 13 15 Ibuprofen 200 mg film coated Tablet 10's 10's 1.80 relaxants Analgesic & Antipyretic / Muscle 14 16 Ibuprofen 400 mg film coated Tablet 10's 15's 3.50 relaxants Analgesic & Antipyretic -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Pharmacology on Your Palms CLASSIFICATION of the DRUGS
Pharmacology on your palms CLASSIFICATION OF THE DRUGS DRUGS FROM DRUGS AFFECTING THE ORGANS CHEMOTHERAPEUTIC DIFFERENT DRUGS AFFECTING THE NERVOUS SYSTEM AND TISSUES DRUGS PHARMACOLOGICAL GROUPS Drugs affecting peripheral Antitumor drugs Drugs affecting the cardiovascular Antimicrobial, antiviral, Drugs affecting the nervous system Antiallergic drugs system antiparasitic drugs central nervous system Drugs affecting the sensory Antidotes nerve endings Cardiac glycosides Antibiotics CNS DEPRESSANTS (AFFECTING THE Antihypertensive drugs Sulfonamides Analgesics (opioid, AFFERENT INNERVATION) Antianginal drugs Antituberculous drugs analgesics-antipyretics, Antiarrhythmic drugs Antihelminthic drugs NSAIDs) Local anaesthetics Antihyperlipidemic drugs Antifungal drugs Sedative and hypnotic Coating drugs Spasmolytics Antiviral drugs drugs Adsorbents Drugs affecting the excretory system Antimalarial drugs Tranquilizers Astringents Diuretics Antisyphilitic drugs Neuroleptics Expectorants Drugs affecting the hemopoietic system Antiseptics Anticonvulsants Irritant drugs Drugs affecting blood coagulation Disinfectants Antiparkinsonian drugs Drugs affecting peripheral Drugs affecting erythro- and leukopoiesis General anaesthetics neurotransmitter processes Drugs affecting the digestive system CNS STIMULANTS (AFFECTING THE Anorectic drugs Psychomotor stimulants EFFERENT PART OF THE Bitter stuffs. Drugs for replacement therapy Analeptics NERVOUS SYSTEM) Antiacid drugs Antidepressants Direct-acting-cholinomimetics Antiulcer drugs Nootropics (Cognitive -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

FORMULATION and EVALUATION of COLON TARGETED PELLETS of BUMADIZONE CALCIUM” Mr
THESIS ISSN: 2349-2678 Contents lists available at www.ijpba.in International Journal of Pharmaceutical and Biological Science Archive PubMed (National Library of Medicine ID: 101738825) Index Copernicus Value 2017: 71.80 Volume 7 Issue 3; May-June; 2019; Page No. 01-69 “FORMULATION AND EVALUATION OF COLON TARGETED PELLETS OF BUMADIZONE CALCIUM” Mr. Shah Akashkumar Nareshkumar1, Mr. Anil G. Raval2 1PG Research Scholar, Department of Pharmaceutics, Sharda School of Pharmacy, Pethapur, Gandhinagar, Gujarat 2Assistant Professor, Department of Pharmaceutics, Sharda School of Pharmacy, Pethapur, Gandhinagar, Gujarat ABSTRACT Aim: The aim of this study was to Formulation and Evaluation of colon targeted pellets of Bumadizone Calcium Objective: Bumadizone Calcium is an acetic acid derivative, having irritation in stomach. Bumadizone Calcium has short half-life (4hrs) and undergoes first pass metabolism. It is pH-dependent. This research work was carried out to improve the bioavailability, patient compliance on oral colon targeted drug delivery. Bumadizone Calcium sustained release enteric coated pellets were prepared, which minimize the release of drug in stomach for treatment of IBD formulated by Extrusion Spheronization process. Experimental work done: Enteric coated pellets prepared by Extrusion Spheronization technique. Eudragit S100, HPMC, PVP K30, and Ethyl Cellulose were used as rate controlling polymers. In this study, a pH dependent colon targeted enteric coated pellets was established using 32 full factorial design by giving enteric coating with Eudragit S100. Different Concentration of Eudragit S100 as an enteric coating material (4%, 5%, & %6) and PVP K30 as a Binder (0.5%, 1% & 1.5%) are taken for the measurements of % Drug Release that are performed by using USP dissolution 1 (Basket type) at 50 rpm. -

La Hepatotoxicidad Del Droxicam
Vol. 6, n.º 3 julio - septiembre 1993 butlletí groc Institut Català de Farmacologia Universitat Autònoma de Barcelona La hepatotoxicidad del droxicam Los antiinflamatorios no esteroides (AINE) pue- vía oral a animales de experimentación. 15 Cuando den producir alteraciones hepáticas, que van se disuelve en agua y en medio ácido, así co m o desde aumentos leves, transitorios y subclínicos en el quimo gástrico, se hidroliza inmediatamente de los enzimas hepáticos hasta cuadros bien es- a piroxicam y, según el laboratorio fabricante, se tablecidos de hepatitis citolítica, colostásica o absorbe en forma de piroxicam.16 De hecho, la mixta e, incluso, cuadros de hepatitis crónica. administración de droxicam a animales de labora- to r i o 16 y a seres humanos17 no da lugar a concen- No se conoce exactamente la frecuencia de es- traciones pIasmáticas detectables de droxicam,16 tas reacciones de hepatotoxicidad, pero parece sino de piroxicam. No obstante, se ha podido ser muy baja.1 No obstante, el potencial hepato- comprobar recientemente que tras la administra- tóxico no parece ser el mismo para todos los AINE. En realidad, algunos fueron retirados del ción de droxicam o de piroxicam por vía oral a mercado en los años setenta y ochenta por este ratas, los metabolitos que aparecen en orina no motivo (ibufenac, fenclofenac y benoxaprofeno). son los mismos con ambos fármacos; esto indica- Recientemente en España la Comisión Nacional ría que el metabolismo (probablemente hepático) de Farmacovigilancia recomendó la retirada del no es el mismo y que, por tanto, no se puede mercado del bendazac (Bendalina®), un AINE que, hablar de una equivalencia farmacocinética (y toxi- sin una eficacia clínica bien demostrada, se utili- cológica) absoluta entre los dos fármacos. -

Withdrawing Drugs in the U.S. Versus Other Countries Benson Ninan
Volume 3 | Number 3 Article 87 2012 Withdrawing Drugs in the U.S. Versus Other Countries Benson Ninan Albert I. Wertheimer Follow this and additional works at: http://pubs.lib.umn.edu/innovations Recommended Citation Ninan B, Wertheimer AI. Withdrawing Drugs in the U.S. Versus Other Countries. Inov Pharm. 2012;3(3): Article 87. http://pubs.lib.umn.edu/innovations/vol3/iss3/6 INNOVATIONS in pharmacy is published by the University of Minnesota Libraries Publishing. Commentary POLICY Withdrawing Drugs in the U.S. Versus Other Countries Benson Ninan, Pharm.D.1 and Albert I Wertheimer, PhD, MBA2 1Pharmacy Intern, Rite Aid Pharmacies, Philadelphia, PA and 2Temple University School of Pharmacy, Philadelphia PA Key Words: Drug withdrawals, dangerous drugs, UN Banned Drug list Abstract Since 1979, the United Nations has maintained a list of drugs banned from sale in member countries. Interestingly, there are a number of pharmaceuticals on the market in the USA that have been banned elsewhere and similarly, there are some drug products that have been banned in the United States, but remain on the market in other countries. This report provides a look into the policies for banning drug sales internationally and the role of the United Nations in maintaining the master list for companies and countries to use for local decision guidance. Background recently updated issue is the fourteenth issue, which contains At present, one of the leading causes of death in the U.S. is data on 66 new products with updated/new information on believed to be adverse drug reactions.1-14 More than 20 22 existing products. -

Semantic Query Modeling, Context, Section Detection, and Match Score Maximization
DutchHatTrick: Semantic query modeling, ConText, section detection, and match score maximization. Martijn Schuemie* Dolf Trieschnigg† Edgar Meij‡ ErasmusMC University of Twente University of Amsterdam [email protected] [email protected] [email protected] Introduction This report discusses the collaborative work of the ErasmusMC, University of Twente, and the University of Amsterdam on the TREC 2011 Medical track. Here, the task is to retrieve patient visits from the University of Pittsburgh NLP Repository for 35 topics. The repository consists of 101,711 patient reports, and a patient visit was recorded in one or more reports. Because the training set provided by the track organization was small and not made available until quite late in the competition, we decided to create a small training set ourselves. Not only did this allow us to test several ideas before submitting runs to TREC, it also led to several insights into the data. One finding was that synonyms are widely used. Query expansion was therefore deemed essential to achieve a reasonable performance. Query expansion has been used before in Information Retrieval (IR), and is often divided into statistical and knowledge-based query expansion. Statistical query expansion uses data derived from the corpus itself, and a well-known example is pseudo-relevance feedback [1]. In contrast, we investigated knowledge-based query expansion, which uses a knowledge base such as an ontology or a dictionary to find related terms. This type of query expansion has not always proven to be successful. For instance, Hersh et al. [2] found a decrease in overall search performance when using the Unified Medical Language System (UMLS) [3] to find related terms.