Clinically Relevant Interactions Between Atypical Antipsychotics and Anti-Infective Agents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

"Macrolides"? Classify Each Drug in This Chapter As a Macrolide Or Azalide, and As an Antibiotic Or Semi-Synthetic Derivative
STUDY GUIDE THE MACROLIDE/AZALIDE ANTIMICROBIAL AGENTS 1. Why are these antibiotics derivatives called "macrolides"? Classify each drug in this chapter as a macrolide or azalide, and as an antibiotic or semi-synthetic derivative. 2. What are the key structural differences between erythromycin, clarithromycin, azithromycin and dirithromycin? 3. Generally how does spiramycin and josamycin differ in structure from the commercial macrolides/azalides (2 reasons)? 4. What are the “ketolides and how do they differ in structure from the commercial macrolides? 5. What is the biosynthetic source of erythromycin? What is the lactone moiety of erythromycin called? What sugar moieties are present and what are their properties? 6. What hydrolysis product forms from erythromycin in aqueous acid or base? What is the significance of this reaction? Can it occur with other macrolides? 7. When does the “intramolecular cyclization” reaction occur with erythromycin? What is it's significance (two reasons) and how does it occur? Which functional groups are important for this reaction? 8. What salt forms of erythromycin are available? Which are water soluble? Which are water-insoluble? How is each salt form formulated and used (oral or parenteral)? 9. What ester and ester salt derivatives of erythromycin are available? What is the estolate? How is each salt form formulated and used (oral or parenteral)? What are the advantages of these esters dosage forms? 10. How does clarithromycin differ in structure from erythromycin? Why was this macrolide developed (the role of the 6-methoxy)? 11. How does azithromycin differ in structure from erythromycin? Why was this macrolide developed? 12. How does dirithromycin differ in structure from erythromycin? Why was this macrolide developed? What is the active form of this prodrug? 13. -

35 Cyproterone Acetate and Ethinyl Estradiol Tablets 2 Mg/0
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION PrCYESTRA®-35 cyproterone acetate and ethinyl estradiol tablets 2 mg/0.035 mg THERAPEUTIC CLASSIFICATION Acne Therapy Paladin Labs Inc. Date of Preparation: 100 Alexis Nihon Blvd, Suite 600 January 17, 2019 St-Laurent, Quebec H4M 2P2 Version: 6.0 Control # 223341 _____________________________________________________________________________________________ CYESTRA-35 Product Monograph Page 1 of 48 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION ....................................................................... 3 SUMMARY PRODUCT INFORMATION ............................................................................................. 3 INDICATION AND CLINICAL USE ..................................................................................................... 3 CONTRAINDICATIONS ........................................................................................................................ 3 WARNINGS AND PRECAUTIONS ....................................................................................................... 4 ADVERSE REACTIONS ....................................................................................................................... 13 DRUG INTERACTIONS ....................................................................................................................... 16 DOSAGE AND ADMINISTRATION ................................................................................................ 20 OVERDOSAGE .................................................................................................................................... -

Treatment of Psychosis: 30 Years of Progress
Journal of Clinical Pharmacy and Therapeutics (2006) 31, 523–534 REVIEW ARTICLE Treatment of psychosis: 30 years of progress I. R. De Oliveira* MD PhD andM.F.Juruena MD *Department of Neuropsychiatry, School of Medicine, Federal University of Bahia, Salvador, BA, Brazil and Department of Psychological Medicine, Institute of Psychiatry, King’s College, University of London, London, UK phrenia. Thirty years ago, psychiatrists had few SUMMARY neuroleptics available to them. These were all Background: Thirty years ago, psychiatrists had compounds, today known as conventional anti- only a few choices of old neuroleptics available to psychotics, and all were liable to cause severe extra them, currently defined as conventional or typical pyramidal side-effects (EPS). Nowadays, new antipsychotics, as a result schizophrenics had to treatments are more ambitious, aiming not only to suffer the severe extra pyramidal side effects. improve psychotic symptoms, but also quality of Nowadays, new treatments are more ambitious, life and social reinsertion. We briefly but critically aiming not only to improve psychotic symptoms, outline the advances in diagnosis and treatment but also quality of life and social reinsertion. Our of schizophrenia, from the mid 1970s up to the objective is to briefly but critically review the present. advances in the treatment of schizophrenia with antipsychotics in the past 30 years. We conclude DIAGNOSIS OF SCHIZOPHRENIA that conventional antipsychotics still have a place when just the cost of treatment, a key factor in Up until the early 1970s, schizophrenia diagnoses poor regions, is considered. The atypical anti- remained debatable. The lack of uniform diagnostic psychotic drugs are a class of agents that have criteria led to relative rates of schizophrenia being become the most widely used to treat a variety of very different, for example, in New York and psychoses because of their superiority with London, as demonstrated in an important study regard to extra pyramidal symptoms. -

( 12 ) United States Patent
US010376507B2 (12 ) United States Patent (10 ) Patent No. : US 10 , 376 , 507 B2 Srinivasan et al. (45 ) Date of Patent: Aug. 13 , 2019 CRESEMBA® ( isavuconazonium sulfate ) , Highlights of Prescrib (54 ) METHOD OF TREATING A PATIENT WITH ing Information , Label ; Patient Information approved by the U . S . A CYP3A4 SUBSTRATE DRUG Food and Drug Administration ; Astellas Pharma US , Inc. ( Licensed from Basilea Pharmaceutics International Ltd . ) , Illinois, USA , Ini (71 ) Applicant: Bow River LLC , Corona Del Mar , CA tial U . S . Approval: 2015 , Revised Mar. 2015 , Reference ID : 3712237, ( US ) 28 pages . DIFLUCAN® ( fluconazole ), Label ; Patient Information , Reference ( 72 ) Inventors : Sundar Srinivasan , Corona Del Mar, ID : 3650838 , Roerig , Division of Pfizer Inc ., New York , NY, Revised Mar. 2013 , 35 pages. CA (US ) ; Christina Chow , Seattle , WA NIZORAL® (ketoconazole )Label ; Patient Information approved by (US ) the U . S . Food and Drug Administration , Reference ID : 3458324 , Copyright 2014 Janssen Pharmaceuticals, Inc . , New Jersey, USA , ( 73 ) Assignee : BOW RIVER LLC , Corona del Mar , Revised Feb . 2014 , 23 pages . NOXAFIL® (posaconazole ) , Highlights of Prescribing Informa CA (US ) tion , Label ; Patient Information approved by the U . S . Food and Drug Administration ; Copyright © 2006 , 2010 , 2013 , 2014 Merck ( * ) Notice : Subject to any disclaimer , the term of this Sharp & Dohme Corp . , a subsidiary of Merck & Co ., Inc ., New patent is extended or adjusted under 35 Jersey , USA , Revised Sep . 2016 , Reference ID : 3983525, 37 pages . U . S . C . 154 (b ) by 0 days. ORAVIG® (miconazole ) , Highlights of Prescribing Information , Label ; Patient Information approved by the U . S . Food and Drug Administration ; Copyright 2012 Praelia Pharmaceuticals , Inc . , North (21 ) Appl. -

Erythromycin Versus Tetracycline for Treatment of Mediterranean Spotted Fever
Arch Dis Child: first published as 10.1136/adc.61.10.1027 on 1 October 1986. Downloaded from Archives of Disease in Childhood, 1986, 61, 1027-1029 Erythromycin versus tetracycline for treatment of Mediterranean spotted fever T MUNOZ-ESPIN, P LOPEZ-PARtS, E ESPEJO-ARENAS, B FONT-CREUS, I MARTINEZ- VILA, J TRAVERIA-CASANOVA, F SEGURA-PORTA, AND F BELLA-CUETO Hospital de Sant Llatzer, Terrassa, Clinica Infantil del Nen Jesus, Sabadell, and Hospital Mare de Deu de la Salut, Sabadell, Barcelona, Spain SUMMARY Eighty one children aged between 1 and 13 years participated in a randomised comparative trial of tetracycline hydrochloride and erythromycin stearate for treatment of Mediterranean spotted fever. Both therapeutic regimens proved effective, but in patients treated with tetracycline both clinical symptoms and fever disappeared significantly more quickly. Likewise, when those patients who began treatment within the first 72 hours of illness are considered the febrile period had a significantly shorter duration in the group treated with tetracycline. One patient was switched to tetracycline because there was no improvement of clinical manifestations, with persistence of fever, myalgias, and prostration, after receiving eight days of treatment with erythromycin. These results suggest that tetracyclines are superior to erythromycin in the treatment of Mediterranean spotted fever. copyright. Mediterranean spotted fever is an acute infectious were not included in the trial; neither were those disease caused by Rickettsia conorii. During the -

Addyi Generic Name: Flibanserin Manufacturer
Brand Name: Addyi Generic Name: Flibanserin Manufacturer: Sprout Pharmaceuticals Drug Class: Central Nervous System Agent, Serotonin Agonist, Dopamine antagonist Uses: Labeled Uses: Indicated for the treatment of premenopausal women with acquired, generalized hypoactive sexual desire disorder (HSDD) as characterized by low sexual desire that causes marked distress or interpersonal difficulty and is NOT due to: A co-existing medical or psychiatric condition, problems within the relationship, or the effects of a medication or other drug substance. Unlabeled Uses: none. Mechanism of Action: The mechanism of action for flibanserin in the treatment of hypoactive sexual desire disorder is unknown. Flibanserin has high affinity for serotonin (5-hydroxytryptamine or 5-HT) 1A receptors, as an agonist, and 5-HT2A receptors, as an antagonist, and moderate affinity for 5- HT2B, 5-HT2C, and dopamine D4 receptors as an antagonist Pharmacokinetics: Absorption: Tmax 0.75 hours Vd 50L t ½ 11 hours Clearance Not reported Protein binding 98% (albumin) Bioavailability 33% Metabolism: Flibanserin is extensively metabolized primarily by CYP3A4 and, to a lesser extent, CYP2C19 to at least 35 metabolites, with most of the metabolites occurring in low concentrations in plasma. Elimination: Flibanserin is primarily excreted through the kidneys in to urine (44%) and feces (51%). Two metabolites could be characterized that showed plasma concentration similar to that achieved with flibanserin: 6,21-dihydroxy-flibanserin-6,21-disulfate and 6- hydroxy-flibanserin-6-sulfate. These two metabolites are inactive. Efficacy: Katz M, DeRogatis LR, Ackerman R, et al. Efficacy of flibanserin in women with hypoactive sexual desire disorder: results from the BEGONIA trial. J Sex Med. -
Medication Conversion Chart
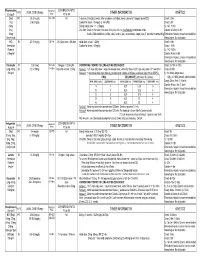
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -
Management of Side Effects of Antipsychotics
Management of side effects of antipsychotics Oliver Freudenreich, MD, FACLP Co-Director, MGH Schizophrenia Program www.mghcme.org Disclosures I have the following relevant financial relationship with a commercial interest to disclose (recipient SELF; content SCHIZOPHRENIA): • Alkermes – Consultant honoraria (Advisory Board) • Avanir – Research grant (to institution) • Janssen – Research grant (to institution), consultant honoraria (Advisory Board) • Neurocrine – Consultant honoraria (Advisory Board) • Novartis – Consultant honoraria • Otsuka – Research grant (to institution) • Roche – Consultant honoraria • Saladax – Research grant (to institution) • Elsevier – Honoraria (medical editing) • Global Medical Education – Honoraria (CME speaker and content developer) • Medscape – Honoraria (CME speaker) • Wolters-Kluwer – Royalties (content developer) • UpToDate – Royalties, honoraria (content developer and editor) • American Psychiatric Association – Consultant honoraria (SMI Adviser) www.mghcme.org Outline • Antipsychotic side effect summary • Critical side effect management – NMS – Cardiac side effects – Gastrointestinal side effects – Clozapine black box warnings • Routine side effect management – Metabolic side effects – Motor side effects – Prolactin elevation • The man-in-the-arena algorithm www.mghcme.org Receptor profile and side effects • Alpha-1 – Hypotension: slow titration • Dopamine-2 – Dystonia: prophylactic anticholinergic – Akathisia, parkinsonism, tardive dyskinesia – Hyperprolactinemia • Histamine-1 – Sedation – Weight gain -
Use of Antibiotics to Prevent Calf Diarrhea and Septiceinia
PEER REVIEWED Use of Antibiotics to Prevent Calf Diarrhea and Septiceinia Peter D. Constable, BVSc, PhD, DACVIM Department of Veterinary Clinical Medicine, University of Illinois at Urbana-Champaign, Urbana, IL 61802 Abstract l'oxytetracycline (0.15 to 6.0 mg/lb [0.32 to 13.2 mg/kg] au 24 h, per os) sont efficaces dans le traitement de la This article reviews studies related to the use of diarrhee chez les veaux et permettent un accroissement antimicrobial agents to prevent calf diarrhea and septi du taux de croissance des veaux nourris au lait. De cemia, and discusses whether prophylactic administra plus, la chlortetracycline permet la diminution du taux tion of antibiotics in neonatal calves is effective and de mortalite lorsque administree chez les veaux indicated. Orally administered chlortetracycline, oxytet nouveau-nes pour prevenir la diarrhee. 11 n'y a pas racycline, tetracycline and neomycin have label claims d'antibiotiques qui promettent de prevenir la in the US for the "control" or "aid in the control" of calf septicemie chez les veaux. Paree qu'il ne semble pas diarrhea caused by bacteria susceptible to the antibi exister d'etudes sur l'efficacite de la tetracycline et de otic. Chlortetracycline and oxytetracycline (0.15 to 6.0 la neomycine et parce que !'utilisation hors homologa mg/lb [0.32 to 13.2 mg/kg], q 24 h, PO) are efficacious tion des medicaments. n'est pas permise pour la for preventing calf diarrhea and increasing growth rate prevention routiniere des maladies ou !'augmentation in milk-fed calves, and chlortetracycline (3 mg/lb [7 mg/ du taux de croissance et du taux de conversion kg], q 12 h, PO) is efficacious for decreasing mortality alimentaire, selon le code de l'AMDUCA de 1994, seule when administered to prevent diarrhea in neonatal !'administration orale de chlortetracycline et calves. -

Topical Corticosteroids and Fungal Keratitis: a Review of the Literature and Case Series
Journal of Clinical Medicine Review Topical Corticosteroids and Fungal Keratitis: A Review of the Literature and Case Series Karl Anders Knutsson 1,*, Alfonso Iovieno 2,3, Stanislav Matuska 1, Luigi Fontana 2 and Paolo Rama 1 1 Cornea and Ocular Surface Unit, San Raffaele Scientific Institute, 20132 Milan, Italy; [email protected] (S.M.); [email protected] (P.R.) 2 Arcispedale Santa Maria Nuova—IRCCS, 42123 Reggio Emilia, Italy; [email protected] (A.I.); [email protected] (L.F.) 3 Department of Ophthalmology, University of British Columbia, Vancouver, BC V6T 1Z, Canada * Correspondence: [email protected] or [email protected]; Tel./Fax: +39-022-6432-648 Abstract: The management of fungal keratitis is complex since signs and symptoms are subtle and ocular inflammation is minimal in the preliminary stages of infection. Initial misdiagnosis of the condition and consequent management of inflammation with corticosteroids is a frequent occurrence. Topical steroid use is considered to be a principal factor for development of fungal keratitis. In this review, we assess the studies that have reported outcomes of fungal keratitis in patients receiving steroids prior to diagnosis. We also assess the possible rebound effect present when steroids are abruptly discontinued and the clinical characteristics of three patients in this particular clinical scenario. Previous reports and the three clinical descriptions presented suggest that in fungal keratitis, discontinuing topical steroids can induce worsening of clinical signs. In these cases, we recommend to slowly taper steroids and continue or commence appropriate antifungal therapy. Citation: Knutsson, K.A.; Iovieno, A.; Keywords: fungal keratitis; topical corticosteroids; topical steroids; rebound effect Matuska, S.; Fontana, L.; Rama, P. -

Antiprotozoal and Antitumor Activity of Natural Polycyclic Endoperoxides: Origin, Structures and Biological Activity
molecules Review Antiprotozoal and Antitumor Activity of Natural Polycyclic Endoperoxides: Origin, Structures and Biological Activity Valery M. Dembitsky 1,2,*, Ekaterina Ermolenko 2, Nick Savidov 1, Tatyana A. Gloriozova 3 and Vladimir V. Poroikov 3 1 Centre for Applied Research, Innovation and Entrepreneurship, Lethbridge College, 3000 College Drive South, Lethbridge, AB T1K 1L6, Canada; [email protected] 2 A.V. Zhirmunsky National Scientific Center of Marine Biology, 17 Palchevsky Str., 690041 Vladivostok, Russia; [email protected] 3 Institute of Biomedical Chemistry, 10 Pogodinskaya Str., 119121 Moscow, Russia; [email protected] (T.A.G.); [email protected] (V.V.P.) * Correspondence: [email protected]; Tel.: +1-403-320-3202 (ext. 5463); Fax: +1-888-858-8517 Abstract: Polycyclic endoperoxides are rare natural metabolites found and isolated in plants, fungi, and marine invertebrates. The purpose of this review is a comparative analysis of the pharmacological potential of these natural products. According to PASS (Prediction of Activity Spectra for Substances) estimates, they are more likely to exhibit antiprotozoal and antitumor properties. Some of them are now widely used in clinical medicine. All polycyclic endoperoxides presented in this article demonstrate antiprotozoal activity and can be divided into three groups. The third group includes endoperoxides, which show weak antiprotozoal activity with a reliability of up to 70%, and this group includes only 1.1% of metabolites. The second group includes the largest number of endoperoxides, Citation: Dembitsky, V.M.; which are 65% and show average antiprotozoal activity with a confidence level of 70 to 90%. Lastly, Ermolenko, E.; Savidov, N.; the third group includes endoperoxides, which are 33.9% and show strong antiprotozoal activity with Gloriozova, T.A.; Poroikov, V.V.