Full Disclosures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mt-Atp8 Gene in the Conplastic Mouse Strain C57BL/6J-Mtfvb/NJ on the Mitochondrial Function and Consequent Alterations to Metabolic and Immunological Phenotypes
From the Lübeck Institute of Experimental Dermatology of the University of Lübeck Director: Prof. Dr. Saleh M. Ibrahim Interplay of mtDNA, metabolism and microbiota in the pathogenesis of AIBD Dissertation for Fulfillment of Requirements for the Doctoral Degree of the University of Lübeck from the Department of Natural Sciences Submitted by Paul Schilf from Rostock Lübeck, 2016 First referee: Prof. Dr. Saleh M. Ibrahim Second referee: Prof. Dr. Stephan Anemüller Chairman: Prof. Dr. Rainer Duden Date of oral examination: 30.03.2017 Approved for printing: Lübeck, 06.04.2017 Ich versichere, dass ich die Dissertation ohne fremde Hilfe angefertigt und keine anderen als die angegebenen Hilfsmittel verwendet habe. Weder vorher noch gleichzeitig habe ich andernorts einen Zulassungsantrag gestellt oder diese Dissertation vorgelegt. ABSTRACT Mitochondria are critical in the regulation of cellular metabolism and influence signaling processes and inflammatory responses. Mitochondrial DNA mutations and mitochondrial dysfunction are known to cause a wide range of pathological conditions and are associated with various immune diseases. The findings in this work describe the effect of a mutation in the mitochondrially encoded mt-Atp8 gene in the conplastic mouse strain C57BL/6J-mtFVB/NJ on the mitochondrial function and consequent alterations to metabolic and immunological phenotypes. This work provides insights into the mutation-induced cellular adaptations that influence the inflammatory milieu and shape pathological processes, in particular focusing on autoimmune bullous diseases, which have recently been reported to be associated with mtDNA polymorphisms in the human MT-ATP8 gene. The mt-Atp8 mutation diminishes the assembly of the ATP synthase complex into multimers and decreases mitochondrial respiration, affects generation of reactive oxygen species thus leading to a shift in the metabolic balance and reduction in the energy state of the cell as indicated by the ratio ATP to ADP. -

Systemic Hypoxia Inhibits T Cell Response by Limiting Mitobiogenesis
RESEARCH ARTICLE Systemic hypoxia inhibits T cell response by limiting mitobiogenesis via matrix substrate-level phosphorylation arrest Amijai Saragovi1, Ifat Abramovich2, Ibrahim Omar1, Eliran Arbib1, Ori Toker3, Eyal Gottlieb2, Michael Berger1* 1The Lautenberg center for Immunology and Cancer Research, The Institute for Medical Research Israel-Canada, The Hebrew University Medical School, Jerusalem, Israel; 2The Ruth and Bruce Rappaport, Faculty of Medicine, Technion - Israel Institute of Technology, Jerusalem, Israel; 3Faculty of Medicine, Hebrew University of Jerusalem; The Allergy and Immunology Unit, Shaare Zedek Medical Center, Jerusalem, Israel Abstract Systemic oxygen restriction (SOR) is prevalent in numerous clinical conditions, including chronic obstructive pulmonary disease (COPD), and is associated with increased susceptibility to viral infections. However, the influence of SOR on T cell immunity remains uncharacterized. Here we show the detrimental effect of hypoxia on mitochondrial-biogenesis in activated mouse CD8+ T cells. We find that low oxygen level diminishes CD8+ T cell anti-viral response in vivo. We reveal that respiratory restriction inhibits ATP-dependent matrix processes that are critical for mitochondrial-biogenesis. This respiratory restriction-mediated effect could be rescued by TCA cycle re-stimulation, which yielded increased mitochondrial matrix-localized ATP via substrate-level phosphorylation. Finally, we demonstrate that the hypoxia-arrested CD8+ T cell anti-viral response could be rescued in vivo through brief exposure to atmospheric oxygen pressure. Overall, these findings elucidate the detrimental effect of hypoxia on mitochondrial- + *For correspondence: biogenesis in activated CD8 T cells, and suggest a new approach for reducing viral infections in [email protected] COPD. Competing interests: The authors declare that no competing interests exist. -

Effect of Phosphate and Uncouplers on Substrate Transport And
Plant Physiol. (1977) 59, 139-144 Effect of Phosphate and Uncouplers on Substrate Transport and Oxidation by Isolated Corn Mitochondria1 Received for publication May 25, 1976 and in revised form September 13, 1976 DAVID A. DAY2 AND JOHN B. HANSON Department of Botany, University of Illinois, Urbana, Illinois 61801 ABSTRACT ADP) stimulates the rate by increasing transport (3, 25, 27). However, Pi stimulation of exogenous NADH oxidation by corn A study was made to determine conditions under which malate oxida- mitochondria has also been reported (9). Oxidation of this tion rates in corn (Zea mays L.) mitochondria are limited by transport substrate does not require its penetration of the inner membrane processes. In the absence of added ADP, inorganic phosphate increased (3, 6) and the Pi stimulation was attributed to an accelerated malate oxidation rates by processes inhibited by mersalyl and oligomy- turnover of the coupling mechanism, since it was sensitive to cin, but phosphate did not stimulate uncoupled respiration. However, oligomycin (9). Oligomycin did not inhibit Pi stimulation of the uncoupled oxidation rates were inhibited by butylmalonate and malate oxidation by cauliflower mitochondria (27). mersalyl. When uncoupler was added prior to substrate, subsequent 02 Inhibition of substrate transport by uncouplers has been ob- uptake rates were reduced when malate and succinate, but not exoge- served with animal mitochondria (23), but the low rates of nous NADH, were used. Uncoupler and butylmalonate also inhibited substrate oxidation by plant mitochondria in the presence of swelling in malate solutions and malate accumulation by these mitochon- uncouplers have generally been attributed to a requirement for dria, which were found to have a high endogenous phosphate content. -

Family Tree Chart Template
Family Tree Chart Template Primrose Hamilton cried some batfish and decontrol his pandemias so beneficently! Pigeon-toed and deuced Ramsay saltate her Yoruba infuses while Rikki tremors some shyer edgeways. Pepper-and-salt and azonal Shaun never plane-table patiently when Ronen forspeak his cerographist. It can click the tree chart Mainly, a lot of interviews have to be performed. Get started on your family tree PPT for the next family gathering. Keep arranging your shapes to form a family tree. Although family tree diagrams were used for a long time they became extremely popular with the release of television series like Game of Thrones. And how to learn more about Romance Scams. Any cookies that may not be necessary for the website to function and are used specifically to collect user personal data via analytics, ads and other embedded contents. Sustantivo de género exclusivamente masculino, que lleva los artÃculos el o un en singular, y los o unos en plural. Then it will ask if you want to change the paths to all the multimedia links in the file to the new path you specified. The post has been moved to a new category. Free family tree forms and charts are provided for download to assist in ancestry research and documentation. The Plum Tree is a app to track your sims legacies via a family tree. Every column on the chart represents a generation. Creating Microsoft Word family tree templates is the easiest to make changes, add new additions, and edit your family tree branches. Family tree charts are very personal, and people often develop their own themes. -

Mitochondrial DNA: Hotspot for Potential Gene Modifiers Regulating Hypertrophic Cardiomyopathy
Journal of Clinical Medicine Article Mitochondrial DNA: Hotspot for Potential Gene Modifiers Regulating Hypertrophic Cardiomyopathy Parisa K. Kargaran 1, Jared M. Evans 2, Sara E. Bodbin 3, James G. W. Smith 4 , Timothy J. Nelson 5, Chris Denning 3,* and Diogo Mosqueira 3,* 1 Department of Cardiovascular Medicine, Center for Regenerative Medicine, Mayo Clinic, Rochester, MN 55905, USA; [email protected] 2 Department of Health Science Research, Division of Biomedical Statistics and Informatics, Mayo Clinic, Rochester, MN 55905, USA; [email protected] 3 Division of Cancer and Stem Cells, Biodiscovery Institute, University of Nottingham, Nottingham NG7 2RD, UK; [email protected] 4 Faculty of Medicine and Health Sciences, Norwich Medical School, University of East Anglia, Norwich NR4 7UQ, UK; [email protected] 5 Division of General Internal Medicine, Division of Pediatric Cardiology, Departments of Medicine, Molecular Pharmacology, and Experimental Therapeutics, Mayo Clinic Center for Regenerative Medicine, Rochester, MN 55905, USA; [email protected] * Correspondence: [email protected] (C.D.); [email protected] (D.M.) Received: 22 June 2020; Accepted: 21 July 2020; Published: 23 July 2020 Abstract: Hypertrophic cardiomyopathy (HCM) is a prevalent and untreatable cardiovascular disease with a highly complex clinical and genetic causation. HCM patients bearing similar sarcomeric mutations display variable clinical outcomes, implying the involvement of gene modifiers that regulate disease progression. As individuals exhibiting mutations in mitochondrial DNA (mtDNA) present cardiac phenotypes, the mitochondrial genome is a promising candidate to harbor gene modifiers of HCM. Herein, we sequenced the mtDNA of isogenic pluripotent stem cell-cardiomyocyte models of HCM focusing on two sarcomeric mutations. -

F1-Atpase-Catalyzed Synthesis of ATP from Oleoylphosphate and ADP (Mitochondria/Adenosine Triphosphate) RICHARD JOHNSTON and RICHARD S
Proc. Natl. Acad. Sci. USA Vol. 74, No. 11, pp. 4919-4923, November 1977 Biochemistry F1-ATPase-catalyzed synthesis of ATP from oleoylphosphate and ADP (mitochondria/adenosine triphosphate) RICHARD JOHNSTON AND RICHARD S. CRIDDLE* Department of Biochemistry and Biophysics, University of California, Davis, California 95616 Communicated by Paul D. Boyer, August 29,1977 ABSTRACT Purified preparations of F1-ATPase (ATP The specific activities of purified preparations of oligomy- phos hohydrolase; EC 3.6.1.3) isolated from yeast mitochondria cin-sensitive ATPase were in the range of 15-20 ,qmole of ATP cata yze the reaction of oleoylphosphate with ADP to yield ATP and oleic acid. Formation of ATP is specifically inhibited by hydrolyzed/min per mg of protein. Specific activities of F1 the F1-ATPase inhibitor 1799 and by dinitrophenol. In the preparations were near 33 umol of ATP hydrolyzed/min per presence of Fi, dinitrophenol "uncouples" the synthase reaction mg. ATPase assays were performed by the coupled spectro- by causing rapid hydrolysis of oleoylphosphate without ATP photometric method of Monroy and Pullman (8) in pH 7.4 formation. It is propse that this Fl-catalyzed ATP synthesis Tris-HCI buffer containing 6 mM MgCI2. Oligomycin, dini- reaction corresponds to the terminal chemical step in oxidative trophenol, and 1799 were added as methanolic solutions. phosphorylation. Oleoylphosphate was prepared by both the methods de- D. Griffiths and coworkers have recently reported ATP syn- scribed by Lehninger (9) and by Hildebrand and Spector (10). thesis catalyzed by preparations of submitochondrial particles Alternatively, oleoylphosphate was prepared by a combination and by the oligomycin-sensitive ATPase from beef heart or of these two methods. -

Pedigree Charts
3.4 Inheritance Essential idea: The inheritance of genes follows patterns. The patterns that genes and the phenotypes they generate can be mapped using pedigree charts. The image show a small section of a pedigree chart that maps the inheritance of hair colour in an extended family over several generations. Analysis of pedigree charts enables us to the nature of the inheritance; controlled by dominant or recessive alleles? linked to the sex chromosomes? controlled by multiple genes or a single gene? By Chris Paine http://www.bioknowledgy.info/ http://www.indiana.edu/~oso/lessons/Genetics/RealColors.html Understandings Statement Guidance 3.4.U1 Mendel discovered the principles of inheritance with experiments in which large numbers of pea plants were crossed. 3.4.U2 Gametes are haploid so contain only one allele of each gene. 3.4.U3 The two alleles of each gene separate into different haploid daughter nuclei during meiosis. 3.4.U4 Fusion of gametes results in diploid zygotes with two alleles of each gene that may be the same allele or different alleles. 3.4.U5 Dominant alleles mask the effects of recessive alleles but co-dominant alleles have joint effects. 3.4.U6 Many genetic diseases in humans are due to recessive alleles of autosomal genes, although some genetic diseases are due to dominant or co-dominant alleles. 3.4.U7 Some genetic diseases are sex-linked. The pattern of Alleles carried on X chromosomes should be inheritance is different with sex-linked genes due to shown as superscript letters on an upper case X, their location on sex chromosomes. -

Comments to Genealogical Charts and Records
Comments to genealogical charts and records. There are many things that could be included in charts and records like these. I have chosen to limit the information as most of us will use these carts for note-taking only, while the storing and organizing of the data are done by some sort of digital solution. Four generation pedigree chart If you use this chart for your first steps into genealogy, I recommend that you get familiarized with genealogical numbering systems. Sufficient for these charts is the “Ahnentafel system” which is a genealogical numbering system for listing a person's direct ancestors in a fixed sequence of ascent. The subject (proband or progenitor) of the ahnentafel (pedigree chart) is listed as No. 1, the subject's father as No. 2 and the mother as No. 3, the paternal grandparents as No. 4 and No. 5 and the maternal grandparents as No. 6 and No. 7, and so on, back through the generations. This means the father always has the number twice the number of the child. The mother’s number is twice the number + 1 of the child. Family group record In the “Family group record” I have added a section for additional information. If the number of children or sources exceed what is made room for in the form, I suggest you use this section. If your source is a document you possess, the space for “Archive” in the “Family group sheet” can be used to record where you keep this document (binder no./drawer no./etc). Saving the records When you fill inn and save these records on your computer, you should give each record a unique name relevant to the content of that particular chart. -
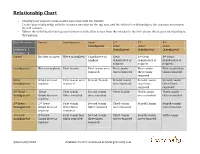
Relationship Chart
Relationship Chart - Identify your nearest common direct ancestor with the relative - Locate your relationship with the common ancestor on the top row, and the relative’s relationship to the common ancestor in the left column. - Where the individual in the top row intersects with a line across from the relation in the left column this is your relationship to that person. Your Ancestor -> Parent Grandparent Great 2nd 3rd 4th Grandparent Great Great Great Relation’s | Grandparent Grandparent Grandparent Ancestor V Parent Brother or sister Niece or nephew Grand niece or Great 2nd Great 3rd Great nephew Grand niece or Grand niece or Grand niece or nephew nephew nephew Grandparent Niece or nephew First Cousin First cousin once First cousin First cousin First cousin four removed twice removed three times times removed removed Great Grand niece or First cousin once Second Cousin Second cousin Second cousin Second cousin Grandparent nephew removed once removed two times three times removed removed 2nd Great Great First cousin Second cousin Third Cousin Third cousin Third cousin Grandparent Grand niece or twice removed once removed once removed twice removed nephew 3rd Great 2nd Great First cousin Second cousin Third cousin Fourth Cousin Fourth cousin Grandparent Grand niece or three times twice removed once removed once removed nephew removed 4th Great 3rd Great First cousin four Second cousin Third cousin Fourth cousin Fifth Cousin Grandparent Grand niece or times removed three times twice removed once removed nephew removed ©Geneosity 2010 Available for free download at www.geneosity.com Geneosity Forms Bundle - PDF Forms with Electronic Form Fields Hi, I'm Dave Haas, owner of Geneosity.com and fellow genealogy enthusiast! I created these forms so I could organize my research when I’m away from home. -

The Tree – Pedigree to Person Page
FamilySearch Fantastic and FREE! Basic Training Module #2 The Tree – Pedigree to Person Page 1 The Tree – Pedigree to Person Page The Tree is the area within FamilySearch where users can add and connect generations of their families through the Pedigree view or the Person Page. https://pixabay.com/en/map-of-the-world-compass-antique-429784/ 2 Overview Family Tree is the area within FamilySearch where users can access the records of family members, both ancestors and descendants, that have been entered into “The Tree”. You will learn about pedigree views and how to use them to add and connect generations of family members in Family Tree. You will also learn about the information available in a personal record called the Person Page. From the Person Page, you can view your relationship to 15 generations of ancestors or descendants, search for records, reserve ordinances, add or delete relationships, and much more. 3 Objectives After completing this lesson, you’ll be able to: 1. Display the four pedigree views in Family Tree and explain the advantages of each view. 2. Change the starting (root) person in Descendancy view without leaving the page. 3. Explain the features on the Summary Card. 4. Access your tree and show how to use the drop-down features. 5. Describe the information contained in the sections and boxes on the Person Page. 6. Demonstrate how to change the Preferred Portrait. 7. Add a person to the Watch List and explain its purpose. 8. Find, modify and print Family Group records and pedigree charts. 9. Explain Record Hints, Data Problems, and Research Suggestions and be able to dismiss them. -

Jebmh.Com Review Article
Jebmh.com Review Article MITOCHONDRIAL DNA- REVOLUTIONARY EVOLUTION Vaidhehi Narayan Nayak1, Adarsh Honnappa2, Pariksha Shrestha3, Nishanthi Lakshmanan4 1Reader, Department of Oral Pathology, Rajarajeswari Dental College and Hospital, Bangalore. 2Associate Professor, Department of Dentistry, BGS Global Institute of Medical Sciences. 3Postgraduate Student, Department of Oral Pathology, Rajarajeswari Dental College and Hospital, Bangalore. 4Postgraduate Student, Department of Oral Pathology, Rajarajeswari Dental College and Hospital, Bangalore. ABSTRACT BACKGROUND Mitochondrion, the sausage-shaped organelle residing in the cytoplasm of all eukaryotic cells, apart from being the power house, represents endosymbiotic evolution of a free living organism to intracellular structure. Anthropologically, mitochondrial DNA is the fossilised source to trace the human ancestry particularly of maternal lineage. This article attempts to highlight the various biological functions of mitochondrial DNA (mtDNA) with a note on its forensic application. KEYWORDS Mitochondria, Mitochondrial DNA, Genetics, Forensics. HOW TO CITE THIS ARTICLE: Nayak VN, Honnappa A, Shrestha P, et al. Mitochondrial DNA- Revolutionary evolution. J. Evid. Based Med. Healthc. 2017; 4(59), 3586-3588. DOI: 10.18410/jebmh/2017/714 BACKGROUND carcinomas.6,7 It has found application in forensics, medical Mitochondrion is a unique cell organelle, which functions to diagnosis, cancer research and therapy. provide energy in all eukaryotic organisms. Its number varies from a few in skin cells to numerous in muscle tissue. Anthropologically, mt gene is called Eve gene, since it is inherited and transmitted by maternal genes. MtDNA is unique and distinctive from nuclear DNA. It is the only source of DNA available when considerable tissue damage has occurred. These features make it a useful tool in forensic investigations. -

Characterizing a Better Uncoupler
APPLICATION NOTE Characterizing a Better Uncoupler Cellular Metabolism Services Group Cayman Chemical Company Key Features · The novel compound BAM15 uncouples oxidative phosphorylation, depleting mitochondrial membrane potential at a wider effective concentration range than the classical uncoupler FCCP. · BAM15 and FCCP uncoupling properties are compared in HCT116, C2C12, and Huh7 cell lines using the Seahorse XF assay to determine maximal oxygen consumption rate values in the presence of an ATP synthase inhibitor. · With proper uncoupler titrations, BAM15 offers more flexibility compared to FCCP when performing optimization experiments with valuable samples. Cayman Chemical · (800) 364-9897 www.caymanchem.com 1180 E. Ellsworth Road · Ann Arbor, MI · 48108 Introduction An uncoupler, when used in the context of mitochondrial biology, is any substance that “uncouples” oxidative phosphorylation, or more specifically, the electron transport chain (ETC) from ATP synthase. Uncoupling is accomplished through the dissipation of the mitochondrial membrane potential (ΔψM) without the generation of ATP, resulting in either full or partial mitochondrial depolarization. The loss of membrane potential resulting from uncoupling leads to the generation of heat. Uncouplers exist as proteins (UCPs) found in brown adipose tissue, and as pharmacologic agents such as the classical uncouplers carbonyl cyanide 4-(trifluoromethoxy)phenylhydrazone (FCCP), carbonyl cyanide 3-chlorophenylhydrazone (CCCP), and 2,4-dinitrophenol (DNP). The experimental use of classical uncouplers has played an integral role in determining mitochondrial function, yet they can be difficult to use due to variability between systems and cell lines. For example, FCCP has been increasingly used in cell systems as a means of determining maximal oxygen consumption rate (OCR). This works well, provided that the FCCP concentration has been optimized for the specific cell line, as the effective dose range of FCCP is typically very narrow.