Latex Allergy Draft
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genital Allergy C Sonnex
4 Sex Transm Infect: first published as 10.1136/sti.2003.005132 on 30 January 2004. Downloaded from REVIEW Genital allergy C Sonnex ............................................................................................................................... Sex Transm Infect 2004;80:4–7. doi: 10.1136/sti.2003.005132 Genital allergy should be considered as a possible Local responses consist of genital swelling, burning, irritation, or soreness which may occur diagnosis in all patients with genital soreness or irritation during or soon after intercourse, usually becom- for which no infection or dermatosis can be identified and ing maximal at 24 hours and lasting 2–3 days.45 in whom symptoms remain unchanged or worsen with Semen contact with non-genital skin may also give rise to localised itching and urticaria.67 treatment. Type I and IV hypersensitivity reactions are most Generalised reactions associated with semen commonly encountered and can be assessed by allergy include angioedema of the lips and performing skin prick testing/radioallergosorbent test eyelids,68 laryngeal oedema,9 bronchospasm,10 and anaphylaxis347 but, to date, death has not (RAST) or patch testing, respectively. Type IV reactions been reported. Semen allergy mainly affects (contact dermatitis) may sometimes prove difficult to younger women although postmenopausal cases distinguish clinically from an irritant dermatitis. This clinical are documented.11 12 An increasing intensity of reaction with subsequent episodes of coitus is a review attempts to summarise key features of genital common feature. Levine et al described a married allergy for the practising clinician. woman with a 15 year history of hay fever who ........................................................................... initially presented with swollen eyes, nasal congestion, and sneezing an hour after coitus. -

Comparative Durability and Abrasion Resistance of Natural and Synthetic
Comparative Durability and Abrasion Resistance of Natural and Synthetic Latex Gloves Ryan Michel2 and Katrina Cornish1,2 Department of Horticulture and Crop Science, 2Department of Food, Agricultural and Biological Engineering, Ohio Agricultural Research and Development Center, The Ohio State University, Wooster, OH 44691 Abstract Medical gloves assist with the prevention of the spread of germs and are required to be worn when working with blood, body tissues, mucous membrane, and broken skin. They should provide good protection between hands and bio hazardous fluids to prevent contamination and promote safety of all healthcare workers and patients. Hence, it is critical for medical gloves to meet a standard performance criterion. Under ASTM D 3577 and D 3578, medical gloves have requirements they must meet in order to be sold and distributed as new gloves. However, there are no industry standards for gloves to meet while in use. The goal of this project was to develop a standard test for glove durability after their initial use. For the tests, gloves were worn by a mechanized prosthetic hand that was put under different conditions which are normally experienced by professionals in the medical field. This design was developed and later confirmed by Dr. Katrina Cornish: Design: Effects of media outside the glove Phosphate buffered saline (PBS), 70% ethanol, air Gloves Tested: Chloroprene, Latex 2, Nitrile, Polyvinyl Chloride and Latex 1 To evaluate glove durability during use, the gloves were immersed in different media before being subjected to contact with an abrasive surface. From this design, ranking of commercially available gloves are developed based on the time until failure of the gloves in these tests. -

Medical Glove Guidance Manual
On December 19, 2016, the FDA published a final rule banning powdered gloves based on the unreasonable and substantial risk of illness or injury to individuals exposed to the powdered gloves (https://www.federalregister.gov/documents/2016/12/19/2016- 30382/banned-devices-powdered-surgeons-gloves-powdered-patient- examination-gloves-and-absorbable-powder). This guidance document has not been updated to reflect the ban. FDA is assessing how to revise this guidance to represent our current thinking on medical gloves. Guidance for Industry and FDA Staff Medical Glove Guidance Manual Document issued on January 22, 2008 This document supersedes Guidance for Medical Gloves – A Workshop Manual, September 30, 1996. For questions regarding this document contact the Infection Control Devices Branch Chief at (301) 796-5580. U.S. Department of Health and Human Services Food and Drug Administration Center for Devices and Radiological Health Office of Device Evaluation Division of Anesthesiology, General Hospital, Infection Control, and Dental Devices Infection Control Devices Branch Preface Public Comment You may submit electronic comments and suggestions at any time for Agency consideration to http://www.regulations.gov. Submit written comments to the Division of Dockets Management, Food and Drug Administration, 5630 Fishers Lane, Room 1061, (HFA-305), Rockville, MD 20852. Identify all comments with the docket number listed in the notice of availability that publishes in the Federal Register. Comments may not be acted upon by the Agency until the document is next revised or updated. Additional Copies Additional copies are available from the Internet. You may also send an e-mail request to [email protected] to receive a copy of the guidance. -

Elastomeric Film Products with Improved Chemical Resistance
Office europeen des brevets (fi) Publication number : 0 524 836 A1 @ EUROPEAN PATENT APPLICATION @ Application number: 92306810.0 @ Int. CI.5: C08L 9/04, C08L 13/02, C08J 5/02 (22) Date of filing : 24.07.92 (§) Priority : 26.07.91 US 736369 @ Inventor : Miller, Robert G. 73 Cherrystone Drive Willowdale, Ontario M2H 1S2 (CA) @ Date of publication of application : Inventor : MacKillop, Duncan A. 27.01.93 Bulletin 93/04 61 Hernshaw Crescent Etobicoke, Ontario M9C 3M6 (CA) Inventor : Tankovitz, Oskar @ Designated Contracting States : 85 Thorncliffe Park Drive, Suite 2606 BE DE DK ES FR GB GR IT LU NL PT Toronto M4H 1L6 (CA) (71) Applicant : ORTHO PHARMACEUTICAL © Representative : Fisher, Adrian John et al CORPORATION CARPMAELS & RANSFORD 43 Bloomsbury U.S. Route 202 P.O. Box 300 Square Raritan New Jersey 08869-0602 (US) London WC1A 2RA (GB) (54) Elastomeric film products with improved chemical resistance. (57) A latex film product such as a prophylactic condom, a surgical glove, a medical examination glove, and the like, having improved chemical resistance, such product comprising a shaped film consisting essentially of a cured mixture of (a) a copolymer of acrylonitrile and butadiene or isoprene, and (b) a high styrene content styrene-butadiene copolymer. < CO CO 00 LU Jouve, 18, rue Saint-Denis, 75001 PARIS EP 0 524 836 A1 The invention relates to elastomeric film products such as prophylactic condoms and surgical gloves made from certain acrylonitrile containing synthetic latexes. Background of the Invention 5 Commercial condoms have been manufactured from natural rubber (NR) latexfor over sixty years. NRIatex is an excellent material for the latex dipping process customarily employed for producing such articles as con- doms, medical gloves, and the like, since it is stable and can readily be compounded with aqueous dispersions of curatives, e.g. -
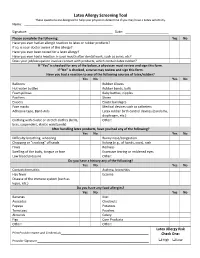
Latex Allergy Screening Tool These Questions Are Designed to Help Your Physician Determine If You May Have a Latex Sensitivity
Latex Allergy Screening Tool These questions are designed to help your physician determine if you may have a Latex sensitivity. Name: ____________________________________ __________ Signature: _________________________________ __________ Date: ______ _______________ Please complete the following: Yes No Have you ever had an allergic reaction to latex or rubber products? If so, is your doctor aware of this allergy? Have you ever been tested for a latex allergy? Have you ever had a reaction in your mouth after dental work, such as sores, etc? Does your job/occupation involve contact with products, which contain latex rubber? If “Yes” is checked for any of the below, a physician must review and sign this form. If “No” is checked, a nurse may review and sign this form. Have you had a reaction to any of the following sources of latex/rubber? Yes No Yes No Balloons Rubber Gloves Hot water bottles Rubber bands, balls Foam pillows Baby bottles, nipples Pacifiers Shoes Erasers Elastic bandages Face masks Medical devices such as catheters Adhesive tape, Band‐Aids Latex rubber birth control devices (condoms, diaphragm, etc.) Clothing with elastic or stretch clothes (belts, Other: bras, suspenders, elastic waistbands) After handling latex products, have you had any of the following? Yes No Yes No Difficulty breathing, wheezing Runny nose/congestion Chapping or “cracking” of hands Itching (e.g., of hands, eyes), rash Hives Redness Swelling of the body, tongue or face Excessive tearing or reddened eyes Low blood pressure Other: Do you have a history any of the following? Yes No Yes No Contact dermatitis Asthma, bronchitis Hay fever Eczema Disease of the immune system (such as lupus, etc.) Do you have any food allergies? Yes No Yes No Bananas Kiwi Avocados Chestnuts Papaya Potatoes Tomatoes Peaches Almonds Celery Figs Corn Products Other: Other: Latex Allergy Risk Print Provider Name and Credentials_________________________________________________ Check One: Provider Signature ______________________________________________________________ High Low . -

Latex Allergy/Student Effective Date: 1/1/10
OCHSNER CLINICAL SCHOOL POLICY Policy #: OCS 400.14 Title: Latex Allergy/Student Effective Date: 1/1/10 PURPOSE The purpose of this policy is to establish guidelines for the identification, follow-up and work practice modification for all OCS medical students with latex sensitivities or allergies to ensure a consistent safe workplace. Students will be classified in the category of Health Care Worker (HCW) on the Ochsner campuses. Health Care Workers with demonstrated latex sensitivity will be provided with engineering controls, protective apparel and other interventions that will minimize opportunities for development of a true latex allergy. HCW’s with a diagnosed latex allergy will be provided a latex safe environment to the extent possible. DEFINITIONS: Latex refers to natural rubber latex and includes products made from dry natural rubber. Natural rubber latex is the product manufactured from a milky fluid derived mainly from the rubber tree, Hevea brasiliensis. High-risk populations are groups known to have a higher risk for latex allergic reactions and include persons: • with occupational exposure to latex, • diagnosed with myelodysplasia, myeloma, congenital urologic abnormalities, or Spina bifida • with history of asthma, hay fever, contact dermatitis, or autoimmune disease (i.e. Lupus), • with food allergies such as bananas, avocados, potatoes, tomatoes, kiwi fruit, peaches, papaya, fruit or chestnuts and • who have exhibited contact dermatitis, itching or redness of the skin following the touching or wearing of latex products. Sensitization is the development of immunological memory in response to exposure to an antigen. Sensitivity is a clinical response that develops after sensitizations. Allergic reactions range from urticaria, rhinitis, conjunctivitis, angiodema, laryngeal edema, cardiovascular changes, GI upset, psychological distress, and bronchospasm, to severe life threatening anaphylaxis. -

Screening Tool
Natural Rubber Latex Allergy Patient Screening Questionnaire When patients are first being assessed, whether in out-patients, assessment clinics, admission or prior to any intervention in clinical settings, it is important that their allergic status is determined as far as is possible. This assessment tool should aid that process. 1. Initial Assessment i. Ask the patient if they have an allergy to any medicines, foods or other items ii. If the patient states that they have no allergies then treat as normal iii. If the patient states that they are allergic to any of the following, this should trigger additional questioning; balloons, contraceptives, rubber gloves, dental blocks, hot water bottles, erasers, rubber bands/balls, pillows, elastic dressing and bandages, elastic waistbands/underwear. iii. If the patient states that they are allergic to any of the following, this should trigger additional questioning; apples, avocados, bananas, celery, cherries, chestnuts, ficus, figs, grapes, kiwi, latex, mangoes, melons, passion fruit, peaches, pears, pistachios, potatoes, ragweed, strawberries, tomatoes. TREAT AS HIGH RISK 2. Further questions a. Ask the patient what symptoms they experience when they eat/touch the products listed above b. If the patient states any of the following symptoms, further questions should be asked; breathlessness, skin redness, chapping or cracking of hands, swelling of lips or tongue, runny nose, congestion, hives, itching. TREAT AS TYPE I 3. Assessment conclusion If the patient in addition to positive responses to the questions above, suffers from any of the following then treat as a high risk individual and follow the protocol; • Contact dermatitis • Spina bifida • Eczema • Multiple genitourinary • Asthma • Auto-immune disease (Lupus etc) • Hay fever TREAT AS TYPE I If the patient assessment results in a high-risk outcome, then label the patient’s notes and notify all others who may treat the patient. -

Egg Allergy: Diagnosis and Immunotherapy
International Journal of Molecular Sciences Review Egg Allergy: Diagnosis and Immunotherapy Dulashi Withanage Dona and Cenk Suphioglu * NeuroAllergy Research Laboratory (NARL), School of Life and Environmental Sciences, Faculty of Science, Engineering and Built Environment, Deakin University, 75 Pigdons Road, Geelong 3216 VIC, Australia; [email protected] * Correspondence: [email protected]; Tel.: +61-3-5227-2886 Received: 1 May 2020; Accepted: 14 July 2020; Published: 16 July 2020 Abstract: Hypersensitivity or an allergy to chicken egg proteins is a predominant symptomatic condition affecting 1 in 20 children in Australia; however, an effective form of therapy has not yet been found. This occurs as the immune system of the allergic individual overreacts when in contact with egg allergens (egg proteins), triggering a complex immune response. The subsequent instantaneous inflammatory immune response is characterized by the excessive production of immunoglobulin E (IgE) antibody against the allergen, T-cell mediators and inflammation. Current allergen-specific approaches to egg allergy diagnosis and treatment lack consistency and therefore pose safety concerns among anaphylactic patients. Immunotherapy has thus far been found to be the most efficient way to treat and relieve symptoms, this includes oral immunotherapy (OIT) and sublingual immunotherapy (SLIT). A major limitation in immunotherapy, however, is the difficulty in preparing effective and safe extracts from natural allergen sources. Advances in molecular techniques allow for the production of safe and standardized recombinant and hypoallergenic egg variants by targeting the IgE-binding epitopes responsible for clinical allergic symptoms. Site-directed mutagenesis can be performed to create such safe hypoallergens for their potential use in future methods of immunotherapy, providing a feasible standardized therapeutic approach to target egg allergies safely. -

What Is Natural Rubber Latex?
latex allergy latexallergy What is natural rubber latex? NATURAL RUBBER IS A HIGHLY PROCESSED PLANT PRODUCT FROM THE LATEX OF THE COMMERCIAL RUBBER TREE. ABOUT 90% IS PROCESSED FOR MANUFACTURE OF EXTRUDED RUBBER PRODUCTS, MOULDED GOODS OR PNEUMATIC TYRES. The remaining 10% is used for the manufacture of rubber gloves and other dipped products, such as condoms, swimming caps and balloons. Although there are traces of latex allergen in tyre dust, dipped rubber products are responsible for most allergic reactions. What is a latex allergy? A latex allergy is an allergy to products made from natural rubber latex. The allergy-causing particles become attached to the cornstarch powder in gloves, swimming caps and balloons. Moisture from the skin can enhance this process. The particles can become airborne and inhaled when products are used. Sensitized individuals react to these particles. Milk protein is sometimes mixed in with latex in surgical and household gloves and this can be the cause of reactions in milk allergic individuals. Who is at risk of a latex allergy? Adults and children most at risk are those with other allergies such as eczema, asthma and hayfever.Those who have regular contact with natural rubber latex such as powdered gloves or catheters are the most likely to become sensitized. What are the symptoms of a latex allergy? The reactions can be mild and cause rashes on the hands, itchy swollen eyes, runny nose and sneezing.An asthma attack can occur. latex allergy It is also possible to have a severe life threatening allergic reaction (anaphylactic shock).This is occurs when the latex particles come in contact with mucous membranes. -

A Critical Review of the Assessment of Medical Gloves
This is a repository copy of A critical review of the assessment of medical gloves. White Rose Research Online URL for this paper: http://eprints.whiterose.ac.uk/157053/ Version: Accepted Version Article: Preece, D., Lewis, R. orcid.org/0000-0002-4300-0540 and Carre, M.J. (2020) A critical review of the assessment of medical gloves. Tribology: Materials, Surfaces and Interfaces. ISSN 1751-5831 https://doi.org/10.1080/17515831.2020.1730619 This is an Accepted Manuscript of an article published by Taylor & Francis in Tribology: Materials, Surfaces and Interfaces on 23 Feb 2020, available online: http://www.tandfonline.com/10.1080/17515831.2020.1730619. Reuse Items deposited in White Rose Research Online are protected by copyright, with all rights reserved unless indicated otherwise. They may be downloaded and/or printed for private study, or other acts as permitted by national copyright laws. The publisher or other rights holders may allow further reproduction and re-use of the full text version. This is indicated by the licence information on the White Rose Research Online record for the item. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ A Critical Review of the Assessment of Medical Gloves D. Preecea*, R. Lewis and M. J. Carré aDepartment of Mechanical Engineering, University of Sheffield, Sheffield, United Kingdom; *[email protected] Abstract Medical protective gloves must be assessed to adequate standards before becoming available for commercial use. -

Latex Allergy in the Hospital
Latex Allergy in the Hospital What is a latex allergy? Latex is found in a variety of products, from everyday household items to many articles used in routine medical and dental care. An allergic reaction to natural rubber latex is actually a reaction to a protein contained in the sap of the Brazilian rubber tree (Hevea brasiliensis). This sap is used in manufacturing latex products. Who is at risk to develop latex allergy? People with spina bifida Health care workers such as: doctors, nurses, surgical staff, dentists, dental hygienists, emergency medical services personnel, lab technicians People with other types of allergies or asthma People who have had many surgeries or medical procedures Rubber industry workers: those working in tire factories, rubber manufacturing and glove manufacturing What are some of the symptoms of latex allergy? Skin rash or itching (generally on the hands) Hives Swollen red skin Swollen lips and tongue with difficulty breathing, wheezing Shortness of breath Dizziness Fainting Abdominal (belly) pain Diarrhea UMHS Hospitals and Health Centers - 1 - In very rare cases people with a latex allergy may suffer an anaphylactic shock, a severe allergic reaction that may be life threatening. Symptoms of anaphylaxis shock include: Throat hoarseness or swelling Persistent wheezing Fainting Low blood pressure The risk of anaphylactic shock seems to be greatest in people who have had: Previous allergic reactions to products that contain latex. Prior anaphylaxis with an unknown cause. What is the treatment? Certain medications may reduce allergy symptoms but the most effective approach is to reduce exposure to latex products. How can I avoid exposure to latex in the hospital? Many hospital items and supplies contain latex. -

Latex Allergy and Foods Positioned Here SUB TITLECARE POSITIONED INSTRUCTIONS HERE
Title of article is Latex Allergy and Foods positioned here SUB TITLECARE POSITIONED INSTRUCTIONS HERE The foods listed in the chart below have shown to cause allergic reactions in some individuals with latex allergy. Reactions can occur because these foods contain a protein that resembles a protein in latex. If you have had an allergic reaction to any of these foods, you should avoid them in the future. Some allergists recommend that ALL persons with latex allergy should avoid the four foods with the *highest prevalence of reactions. During your hospitalization, avocado, banana, chestnut and kiwi will be omitted from your diet. Please be aware that as more research is done this list may change. LATEX RELATED FOODS *HIGH PREVALENCE OF Moderate Prevalence of Lower Prevalence of REACTION Reaction Reaction Avocado Apple Apricot Banana Carrot Cherry Chestnut Celery Coconut Kiwi Cherimoya Fig Melons Grapes Papaya Loquat Potato Mango Tomato Nectarine Nuts (all) Passion fruit Peach Pear Plum Swiss chard This information is not intended to diagnose health problems or to take the place of medical advice or care you receive from your physician or other health care professional. If you have persistent health problems, or if you have additional questions, please consult your doctor. If you have questions or need more information about your medication, please speak to your pharmacist. Kaiser Permanente does not endorse any brand names; any similar products may be used. Herbs and supplements are sold over-the-counter. Kaiser Permanente carries only herb categories for which some evidence exists to show that the herbs may be effective to treat certain medical conditions.