D0411 and D0412 – ADA Quick Guide to In-Office Monitoring and Documenting Patient Blood Glucose and Hba1c Level
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetically Determined Hypoalbuminemia As a Risk Factor for Hypertension: Instrumental Variable Analysis Jong Wook Choi1, Joon‑Sung Park2* & Chang Hwa Lee2*
www.nature.com/scientificreports OPEN Genetically determined hypoalbuminemia as a risk factor for hypertension: instrumental variable analysis Jong Wook Choi1, Joon‑Sung Park2* & Chang Hwa Lee2* Hypoalbuminemia is associated with vascular endothelial dysfunction and the development of chronic cardiovascular diseases. However, the relationship between serum albumin concentration and blood pressure changes remains controversial. Community‑based longitudinal cohort data collected from Korean Genome and Epidemiology Study were used in this study. Hypoalbuminemia was defned as a serum albumin concentration of ≤ 4.0 g/dL. A total of 4325 participants were categorized into control (n = 3157) and hypoalbuminemia (n = 1168) groups. Serum albumin had a non‑linear relationship with the risk of hypertension development. A genome‑wide association study revealed 71 susceptibility loci associated with hypoalbuminemia. Among susceptibility loci, genetic variations at rs2894536 in LOC107986598 and rs10972486 in ATP8B5P were related to elevated blood pressure. Serum albumin (HR = 0.654, 95% CI 0.521–0.820) and polymorphisms of rs2894536 (HR = 1.176, 95% CI 1.015–1.361) and rs10972486 (HR = 1.152, 95% CI 1.009–1.316) were signifcant predictors of hypertension development. Increased albumin concentration instrumented by 2 hypoalbuminemia‑associated SNPs (rs2894536 and rs10972486) was associated with decreased HRs for hypertension development (HR = 0.762, 95% CI 0.659–0.882 and HR = 0.759, 95% CI 0.656–0.878). Our study demonstrated that genetically determined hypoalbuminemia is a signifcant predictor of incipient hypertension. Albumin, one of the major serum proteins, has multiple important physiological functions involving stabilization of plasma colloid osmotic pressure, transportation of diverse substances, and signifcant antioxidant activity, and its concentration is fnely regulated by various systems in the physiologic state 1. -

Glycated Hemoglobin and Glycated Albumin in Patients with Diabetes
Kitajima et al. Renal Replacement Therapy (2020) 6:10 https://doi.org/10.1186/s41100-020-0260-5 RESEARCH Open Access Glycated hemoglobin and glycated albumin in patients with diabetes undergoing hemodiafiltration Yukie Kitajima1*, Shunichiro Urabe2, Takashi Hosono2, Satoshi Yoshikawa3, Yuzuru Sato3 and Toru Hyodo2 Abstract Background: Online hemodiafiltration (OHDF), which results in high albumin leakage, is now widely used in Japan for dialysis, since the national insurance system began reimbursing its costs in 2012. Glycated albumin (GA) levels are affected by albumin leakage into effluent dialysate fluid. Therefore, GA levels in patients requiring diabetes- related dialysis undergoing OHDF require monitoring. However, there have been no previous reports on glycemic control indicators of patients with diabetes undergoing OHDF. We aimed to develop a glycemic control index for patients requiring diabetes-related dialysis undergoing OHDF. Methods: This study comprised 133 diabetic patients undergoing OHDF. We examined the correlation between GA and glycated hemoglobin (HbA1c) levels. We analyzed effluent dialysate fluid samples from 41 patients classified into 3 groups, namely, group A, non-protein-leaking OHDF (n = 20); group B, protein-leaking OHDF (n = 14); and group C, highly efficient protein-leaking OHDF (n = 7). We examined the association between GA and HbA1c levels in each group and among patients. Results: A significant positive correlation was observed between GA and HbA1c levels (r = 0.562, p < 0.0001). There was no significant correlation between pre-dialysis blood glucose levels and HbA1c or GA levels as observed on regular blood tests performed under non-fasting conditions. Patients were classified into 2 groups based on their mean albumin levels (3.4 g/dL cutoff). -

Checking Blood Sugar Levels
Checking Blood Sugar Levels People with type 1 diabetes (T1D) must check their blood sugar (glucose) levels throughout the day using a blood glucose meter. The meter tells them how much glucose is in their blood at that particular moment. Based upon the reading, they take insulin, eat, or modify activity to keep blood sugars within their target range. Regularly checking blood sugar levels is an essential part of T1D care. Methods for Checking Blood Sugar Levels Checking, or testing, involves taking a drop of blood, usually from the fingertip, and placing it on a special test strip in a glucose meter. Blood sugar meters are easy to use, and even young children often learn quickly how to do their own blood sugar checks. In order to properly manage their diabetes, individuals with T1D check their blood sugar levels several times per day. For example, they may test before eating lunch and before strenuous exercise. Blood sugar levels are measured in milligrams per deciliter (mg/dL). A normal blood sugar level is between 70 and 120 mg/dL. Keeping blood sugar levels within this range may be difficult in children with diabetes. Therefore, an individual's doctor may adjust the target range (for example, 80-180 mg/dL). However, people with diabetes can't always maintain blood sugar levels within the target range, no matter how hard they try. A person's varying schedules and eating habits, as well as the physical changes that occur as they grow, can send blood sugar levels out of range for no apparent reason. -

Hba1c Matters
HbA1c Matters What is HbA1c? The HbA1c reading reveals your average blood sugar level over the past three months. When blood sugar levels are high, sugar attaches to the red blood cells. The HbA1c monitors how much sugar is attached to the red blood cells, which have a lifespan of about 3 months. The HbA1c reading is therefore able to show what your average blood sugar levels have been in the last 3 months. The units we report HbA1c in are changing, and in the future you will see it reported as a whole number rather than a percentage. Both units are given below. Why does it matter? HbA1c levels are linked with risk of diabetes complications, with higher readings increasing the chance of problems. This is illustrated in the graph below. 15 13 Retinopathy 11 Nephropathy Relative 9 Risk 7 Neuropathy 5 Microalbuminuria 3 1 6 7 8 9 10 11 12 Previous method % 42 53 64 75 86 97 108 New IFCC method HbA1c The graph shows the risk of complications associated with diabetes including retinopathy (eye damage that can lead to blindness), nephropathy (kidney damage that can lead to kidney failure and a need for dialysis), neuropathy (damage to the nerves) and microalbuminuria (protein in the urine which is associated with kidney damage). When HbA1c levels are below 7.5% or 58 mmol/mol, the risk of each of these complications is very low – approximately equivalent to people who do not have diabetes. The risk of each complication rises increasingly steeply as HbA1c levels rise above 7.5% or 58 mmol/mol. -

Deducing Serum Fructosamine Levels from the Fasting Blood Glucose Value: a Preliminary Study H
http://doi.org/10.4038/cjms.v44i2.4863 Deducing serum fructosamine levels from the fasting blood glucose value: a preliminary study H. Perns' The Ceylon Journal of Medical Science 2001; 44:25-28 Abstract However, recent studies have shown that fructosamine (glycated protein) can be used to The determination of glycated serum proteins differentiate between well and poorly stabilized (fructosamine) has become an accepted index for diabetics (1). Fructosamines are stable keto- assessing the metabolic situation in diabetic amines formed by a non-enzymatic reaction patients. The current study describes an alternative between a sugar and a protein. It has been known to measurement of fructosamine level, viz., to that a number of proteins, e.g., haemoglobin, predict the serum fructosamine based on the serum proteins, membrane proteins, protein in glucose concentration in fasting plasma. A cross- the lens of eye etc. are glycated by a non- sectional prospective study was performed on 44 enzymatic reaction and forms a stable fructo non-diabetic, 38 impaired glucose tolerance and samine (isoglucosamine) which depends on the 38 diabetic subjects attending clinics at Colombo glucose concentration. The glycated serum South Teaching Hospital. Fasting plasma glucose proteins form very quickly with changes in the and corresponding serum fructosamine glucose concentration than the glycated concentrations were determined on all subjects. haemoglobin (HbA ) formed in the erythrocytes. Fructosamine showed a positive linear correlation ]c The largest fraction, about 60-70% of glycated of r2 = 0.85 with the fasting plasma glucose serum proteins, consists of albumin with a half- concentrations. Regression equation relating to life in serum about 2-3 weeks (2). -

Liquid QC™ Bilirubin Control
Hemoglobin A1C Reagent ® INTENDED USE FOR IN VITRO DIAGNOSTIC USE No special additives or preservatives other than anticoagulants are required. Collect Hemoglobin A1c (HbA1c) Reagent is intended for the quantitative determination of venous blood with EDTA using aseptic technique. Hemoglobin A1c in human blood. INTERFERING SUBSTANCES SUMMARY Bilrubin to 50 mg/dl, ascorbic acid to 50 mg/dl, triglycerides to 2000 mg/dl, The determination of HbA1c is most commonly performed for the evaluation of carbamylated Hb to 7.5 mmol/L and acetylated Hb to 5.0 mmol/L do not interfere with glycemic control in diabetes mellitus. HbA1c values provide an indication of glucose this assay. See also the LIMITATION SECTION. levels over the preceding 4-8 weeks. A higher HbA1c value indicates poorer glycemic control. PROCEDURE Throughout the circulatory life of the red cell, HbA1c is formed continuously by the Materials provided adduction of glucose to the N-terminal of the hemoglobin beta chain. This process, 85621 R1 1 x 30 mL which is non-enzymatic, reflects the average exposure of hemoglobin to glucose over R2A 1 x 9.5 mL an extended period. In a classical study, Trivelli, et al, (10.1) showed HbA1c in diabetic subjects to be elevated 2-3 fold over the levels found in normal individuals. R2B 1 x 0.5 mL Several investigators have recommended HbA1c serve as an indicator of metabolic R3 1 x 200 mL control of the diabetic, since HbA1c levels approach normal levels for diabetics in metabolic control. (10.2,10.3,10.4) HBA1c has been defined operationally as the “fast Materials required but not provided fraction” hemoglobins (HbA , A , A ) that elute first during column chromatography 1a 1b 1c 1. -

Profiling Glycated Hemoglobin Level, Lactate Dehydrogenase And
International Journal of Medical Laboratory 2017;4(2):135-141. Original Article Profiling Glycated Hemoglobin Level, Lactate Dehydrogenase and Alkaline Phosphatase Activity in Gestational Diabetes Mellitus Obese Women and Compare Them with Each Other Mohammadreza Nadimi Barforoushi1M.Sc. , Durdi Qujeq2,3*Ph.D Bostan Roudi1Ph.D. 1Department of Biology, Damghan Branch, Islamic Azad University, Damghan, Iran. 2Department of Clinical Biochemistry, Faculty of Medicine, Babol University of Medical Sciences, Babol, Iran. 3Cellular and Molecular Biology Research Center (CMBRC), Health Research Institute, Babol University of Medical Sciences, Babol, Iran. A B S T R A C T Article history Background and Aims: The aim of this study was profiling glycated Received 16 Feb 2017 hemoglobin (HbA1c) level, lactate dehydrogenase (LDH) and alkaline Accepted 7 May 2017 phosphatase (ALP) activity in obese women with gestational diabetes Available online 28 Jun 2017 mellitus (GDM) and evaluating the correlation between them. Key words Materials and Methods: Sample size was 90 subjects admitted to the Alkaline phosphatase activity clinical laboratory, who were divided into three groups, in each group Gestational diabetes mellitus (n=30). Subjects glycemic control was checked by HbA1c; ALP, LDH Glycated hemoglobin activity and serum glucose were determined with commercial kit. Age and Lactate dehydrogenase body mass index (BMI) was recorded for each subject. The correlation analysis between blood activity of ALP, LDH activity, HbA1c, glucose, BMI and age in diabetic and normal pregnant women was carried out. Results: The mean of HbA1c level was significantly higher in the GDM obese women than in women with normal pregnancy (p=0.01). In contrast, the means of ALP and LDH activity were lower in the GDM obese women Downloaded from ijml.ssu.ac.ir at 3:56 IRST on Thursday September 30th 2021 than in women with normal pregnancy (p=0.09, and p=0.15, respectively). -

To Study the Co-Relationship Between Glycosylated Hemoglobin and Serum Calcium Levels in Type 2 Diabetes Mellitus Patients
International Journal of Medical and Health Research International Journal of Medical and Health Research ISSN: 2454-9142 Received: 13-01-2020; Accepted: 14-02-2020; Published: 09-03-2020 www.medicalsciencejournal.com Volume 6; Issue 03; 2020; Page No. 43-45 To study the co-relationship between glycosylated hemoglobin and serum calcium levels in type 2 diabetes mellitus patients Dr. Hardeep Singh Deep1, Dr. Jasmine Kaur2, Dr. Gurjyot Singh Nanda3, Dr. Seerat Kaur4 1 Professor MD Medicine Sri Guru Ram Das University of Health Sciences, Amritsar, Punjab, India 2 Assistant. Professor MD Medicine Sri Guru Ram Das University of Health Sciences, Amritsar, Punjab, India 3 junior resident Medicine Sri Guru Ram Das University of Health Sciences, Amritsar, Punjab, India 4 junior resident Radiodiagnosis Sri Guru Ram Das University of Health Sciences, Amritsar, Punjab, India Abstract Background: The incidence of type-2 Diabetes Mellitus has increased world-wide making it a major public health problem. Electrolyte and mineral abnormalities are common in patients with type-2 Diabetes Mellitus. Therefore, this study was undertaken to look for the correlation between HbA1c (glycated hemoglobin) and serum calcium levels in patients with type-2 Diabetes Mellitus. Aim: To study the co-relationship between glycosylated hemoglobin and serum calcium levels in type 2 diabetes mellitus patients. Materials and Methods: A total of 50 type 2 Diabetic patients and 50 healthy non-Diabetic individuals were included for the study. Both fasting and post prandial blood samples were collected from the two groups and were used for fasting blood sugar, HbA1c, serum calcium, RFT, LFT, CBC, UACR. -

Correlation Between Glycated Hemoglobin and Venous Blood Sugar in Diabetic Patients Monitored in Abidjan
Vol. 14(4), pp. 135-141, October-December 2020 DOI: 10.5897/AJBR2020.1102 Article Number: CD65C6E65033 ISSN 1996-0778 Copyright © 2020 Author(s) retain the copyright of this article African Journal of Biochemistry Research http://www.academicjournals.org/AJBR Full Length Research Paper Correlation between glycated hemoglobin and venous blood sugar in diabetic patients monitored in Abidjan MONDE Aké Absalome1*, CAMARA-CISSE Massara2, KOFFI Konan Gervais2, DIALLO Issiagha3, AKE AKE Alexandre4, YAPO-AKE Bénédicte4, ECRABEY Yann Christian3, KOUAKOU Francisk3, BENE YAO Roger Espérance4 and TIAHOU Georges5 1Félix HOUPHOUËT-BOIGNY University, Cocody, Abidjan, Côte d’Ivoire. 2Biochemistry Laboratory, Abidjan Medical School, Félix HOUPHOUËT BOIGNY University, Côte D'ivoire. 3Biochemistry Laboratory, University Hospital Center of Treichville, Côte D'ivoire. 4Laboratory of Medical Biochemistry, Faculty of Medical Sciences, Félix HOUPHOUËT-BOIGNY University, Côte D'ivoire. 5Laboratory of Medical Biochemistry, Faculty of Medical Sciences, Alassane OUATTARA University, Bouaké, Côte D'ivoire. Received 23 August, 2020; Accepted 2 October, 2020 The aim of this study was to determine the correlation between glycated hemoglobin and blood sugar levels in diabetic subjects carried out in Abidjan. This cross-sectional study included 100 patients with diabetes monitored, for three months, for whom glycated blood glucose and hemoglobin were performed, this after informed consent of the patients. Pearson and Spearman correlation tests were used, at the 5% threshold. The patients with normal HbA1C and normal blood glucose accounted for 55.34 and 32%, respectively. A sedentary lifestyle and body mass index > 25 kg/m² were associated with a significant increase in the risk of increased blood glucose and HbA1C. -

89 Abstract a Study of Gamma
89 A STUDY OF GAMMA-GLUTAMYLTRANSFERASE (GGT) IN TYPE 2 DIABETES MELLITUS AND ITS RISK FACTORS Shrawan Kumar Meena1, Alka Meena2, Jitendra Ahuja3, Vishnu Dutt Bohra1 1Dept. of Biochemistry, Jhalawar Medical College, And Hospital, Jhalawar (Raj) ijcrr 2Dept. of Biochemistry, Lady Harding medical college and hospital, New Delhi Vol 04 issue 11 3Dept. of Biochemistry, Geetanjali Medical College and Hospital, Udaipur (Raj) Category: Research Received on:18/04/12 Revised on:29/04/12 E-mail of Corresponding Author: [email protected] Accepted on:09/05/12 ABSTRACT Objective — To study the Serum gamma-glutamyltransferase (GGT), other liver derived enzymes and lipid profile in patients of type 2 Diabetes mellitus (DM) and find out the any correlation of liver derived enzymes with diabetic related risk factor and association between enzyme level and blood sugar level in diabetic and non diabetic subjects. Research Design and Methods— This is a cross-sectional prospective study in 60 cases of type 2 DM randomly selected from medical wards of a tertiary care hospital and 30 age, sex matched controls. Blood sugar, Serum gamma-glutamyl transferase (GGT), other liver enzymes like SGOT, SGPT, ALP, Lipid profile, BMI, waist circumference and prevalence of obesity and hypertension were assessed. To define the type 2 Diabetes mellitus (DM) we used revised criteria of ADA, 1997. Results— GGT, Fasting Blood glucose and BMI increased statistically significant (p<0.00l) in type 2 DM subjects when compared with the control subjects. Statistically significant difference (p<0.05) in SGPT was found in subjects of type 2 DM. Comparison of other parameters like BP, alkaline phosphates, PL, TG and VLDL were also found Statistically significant difference (p<0.01). -

Relationship Between Diabetes Mellitus and Serum Uric Acid Levels
Int. J. Pharm. Sci. Rev. Res., 39(1), July – August 2016; Article No. 20, Pages: 101-106 ISSN 0976 – 044X Review Article Relationship between Diabetes Mellitus and Serum Uric Acid Levels J. Sarvesh Kumar*, Vishnu Priya V1, Gayathri R2 *B.D.S I ST YEAR, Saveetha Dental College, 162, P.H road, Chennai, Tamilnadu, India. 1Associate professor, Department of Biochemistry, Saveetha Dental College, 162, P.H Road, Chennai, Tamilnadu, India. 2Assistant professor, Department of Biochemistry, Saveetha Dental College, 162, P.H Road, Chennai, Tamilnadu, India. *Corresponding author’s E-mail: [email protected] Accepted on: 03-05-2016; Finalized on: 30-06-2016. ABSTRACT The aim of the study is to review the association between diabetes Mellitus and serum uric acid levels. The objective is to review how uric acid level is related to diabetes Mellitus. Diabetes is an increasingly important disease globally. New data from IDF showed that there are 336 million people with diabetes in 2011 and this is expected to rise to 552 million by 2030. It has been suggested that, diabetic epidemic will continue even if the level of obesity remains constant. The breakdown of foods high in protein into chemicals known as purines is responsible for the production of uric acid in the body. If there is too much of uric acid in the body it causes variety of side effects. Thus identifying risk factors of serum uric acid is required for the prevention of diabetes. The review was done to relate how serum uric acid level is associated with the risk of diabetes. -
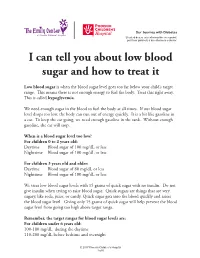
I Can Tell You How the Donor Will Be Determined
Our Journey with Diabetes Si usted desea esta información en español, por favor pídasela a su enfermero o doctor. I can tell you about low blood sugar and how to treat it Low blood sugar is when the blood sugar level goes too far below your child’s target range. This means there is not enough energy to fuel the body. Treat this right away. This is called hypoglycemia. We need enough sugar in the blood to fuel the body at all times. If our blood sugar level drops too low, the body can run out of energy quickly. It is a bit like gasoline in a car. To keep the car going, we need enough gasoline in the tank. Without enough gasoline, the car will stop. When is a blood sugar level too low? For children 0 to 2 years old: Daytime Blood sugar of 100 mg/dL or less Nighttime Blood sugar of 100 mg/dL or less For children 3 years old and older: Daytime Blood sugar of 80 mg/dL or less Nighttime Blood sugar of 100 mg/dL or less We treat low blood sugar levels with 15 grams of quick sugar with no insulin. Do not give insulin when trying to raise blood sugar. Quick sugars are things that are very sugary, like soda, juice, or candy. Quick sugar gets into the blood quickly and raises the blood sugar level. Giving only 15 grams of quick sugar will help prevent the blood sugar level from going too high above target range. Remember, the target ranges for blood sugar levels are: For children under 6 years old: 100-180 mg/dL during the daytime 110-200 mg/dL before bedtime and overnight © 2017 Phoenix Children’s Hospital 1 of 6 For children between 6 and 12 years old: 90-180 mg/dL during the daytime 100-180 mg/dL before bedtime and overnight For teens between 13 and 19 years old: 90-130 mg/dL during the daytime 90-150 mg/dL before bedtime and overnight The levels for blood sugars at night are slightly higher because it can be hard to feel and respond to symptoms of low blood sugar when we are sleeping.