Week of October 5, 2020 Behavioral Health Impact Situation Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Early Dance Division Calendar 17-18
Early Dance Division 2017-2018 Session 1 September 9 – November 3 Monday Classes Tuesday Classes September 11 Class September 12 Class September 18 Class September 19 Class September 25 Class September 26 Class October 2 Class October 3 Class October 9 Class October 10 Class October 16 Class October 17 Class October 23 Class October 24 Class October 30 Last Class October 31 Last Class Wednesday Classes Thursday Classes September 13 Class September 14 Class September 20 Class September 21* Class September 27 Class September 28 Class October 4 Class October 5 Class October 11 Class October 12 Class October 18 Class October 19 Class October 25 Class October 26 Class November 1 Last Class November 2 Last Class Saturday Classes Sunday Classes September 9 Class September 10 Class September 16 Class September 17 Class September 23 Class September 24 Class September 30* Class October 1 Class October 7 Class October 8 Class October 14 Class October 15 Class October 21 Class October 22 Class October 28 Last Class October 29 Last Class *Absences due to the holiday will be granted an additional make-up class. Early Dance Division 2017-2018 Session 2 November 4 – January 22 Monday Classes Tuesday Classes November 6 Class November 7 Class November 13 Class November 14 Class November 20 No Class November 21 No Class November 27 Class November 28 Class December 4 Class December 5 Class December 11 Class December 12 Class December 18 Class December 19 Class December 25 No Class December 26 No Class January 1 No Class January 2 No Class January 8 Class -

2020-2021 Academic Calendar
2020-2021 ACADEMIC CALENDAR QUARTER TERMS* Term ID Class Start Date Class End Date Holiday/Breaks WINTER 2020 Winter January 6, 2020 March 28, 2020 January 20, 2020 • Martin Luther King Jr. Day, No Classes March 29-April 5, 2020 • Spring Break, No Classes SPRING 2020 Spring April 6, 2020 June 27, 2020 May 25, 2020 • Memorial Day, College Closed June 28-July 5, 2020 • Summer Break, No Classes July 3, 2020 • Independence Day Observed, College Closed SUMMER 2020 Summer July 6, 2020 September 26, 2020 September 7, 2020 • Labor Day, College Closed September 27-October 4, 2020 • Fall Break, No Classes FALL 2020 Fall October 5, 2020 December 23, 2020 November 26-27, 2020 • Thanksgiving, College Closed December 24, 2020-January 10, 2021 • Winter Break, No Classes WINTER 2021 Winter January 11, 2021 April 3, 2021 January 18, 2021 • Martin Luther King Jr. Day, No Classes April 4-11, 2021 • Spring Break, No Classes SPRING 2021 Spring April 12, 2021 July 3, 2021 May 31, 2021 • Memorial Day, College Closed July 4-11, 2021 • Summer Break, No Classes July 5, 2021 • Independence Day Observed, College Closed SUMMER 2021 Summer July 12, 2021 October 2, 2021 September 6, 2021 • Labor Day, College Closed FALL 2021 Fall October 4, 2021 December 23, 2021 November 25-26, 2021 • Thanksgiving, College Closed December 24, 2021-January 9, 2022 • Winter Break, No Classes *All dates are subject to change without notice. SOUTHERNTECH.EDU 3 MODULAR TERMS* Term ID Class Start Date Class End Date Holidays / Breaks WINTER 2020 January 6, 2020 January 30, 2020 January 20, 2020 • Martin Luther King Jr. -

2021 7 Day Working Days Calendar
2021 7 Day Working Days Calendar The Working Day Calendar is used to compute the estimated completion date of a contract. To use the calendar, find the start date of the contract, add the working days to the number of the calendar date (a number from 1 to 1000), and subtract 1, find that calculated number in the calendar and that will be the completion date of the contract Date Number of the Calendar Date Friday, January 1, 2021 133 Saturday, January 2, 2021 134 Sunday, January 3, 2021 135 Monday, January 4, 2021 136 Tuesday, January 5, 2021 137 Wednesday, January 6, 2021 138 Thursday, January 7, 2021 139 Friday, January 8, 2021 140 Saturday, January 9, 2021 141 Sunday, January 10, 2021 142 Monday, January 11, 2021 143 Tuesday, January 12, 2021 144 Wednesday, January 13, 2021 145 Thursday, January 14, 2021 146 Friday, January 15, 2021 147 Saturday, January 16, 2021 148 Sunday, January 17, 2021 149 Monday, January 18, 2021 150 Tuesday, January 19, 2021 151 Wednesday, January 20, 2021 152 Thursday, January 21, 2021 153 Friday, January 22, 2021 154 Saturday, January 23, 2021 155 Sunday, January 24, 2021 156 Monday, January 25, 2021 157 Tuesday, January 26, 2021 158 Wednesday, January 27, 2021 159 Thursday, January 28, 2021 160 Friday, January 29, 2021 161 Saturday, January 30, 2021 162 Sunday, January 31, 2021 163 Monday, February 1, 2021 164 Tuesday, February 2, 2021 165 Wednesday, February 3, 2021 166 Thursday, February 4, 2021 167 Date Number of the Calendar Date Friday, February 5, 2021 168 Saturday, February 6, 2021 169 Sunday, February -
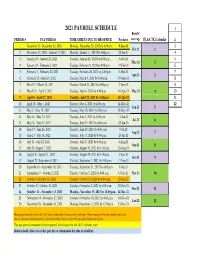
Payroll Calendar 2021
2021 PAYROLL SCHEDULE 1 Benefit PERIOD # PAY PERIOD TIME SHEETS DUE TO HR OFFICE Paydates coverage FLSA 7K Calendar 2 1 December 13- December 26, 2020 Monday, December 28, 2020 by 4:00 p.m. 8-Jan-21 3 Feb-21 1 2 December 27, 2020 - Janurary 9, 2021 Monday, January 11, 2021 by 4:00 p.m. 22-Jan-21 4 3 January 10 - January 23, 2021 Tuesday, January 26, 2021 by 4:00 p.m. 5-Feb-21 5 Mar-21 2 4 January 24 - February 6, 2021 Tuesday, February 9, 2021 by 4:00 p.m. 19-Feb-21 6 5 February 7 - February 20, 2021 Tuesday, February 26, 2021 by 4:00 p.m. 5-Mar-21 7 Apr-21 3 6 February 21 - March 6, 2021 Tuesday, March 9, 2021 by 4:00 p.m. 19-Mar-21 8 7 March 7 - March 20, 2021 Tuesday, March 23, 2021 by 4:00 p.m. 2-Apr-21 9 8 March 21 - April 3, 2021 Tuesday, April 6, 2021 by 4:00 p.m. 16-Apr-21 May-21 4 10 9 April 4 - April 17, 2021 Tuesday, April 20, 2021 by 4:00 p.m. 30-Apr-21 11 10 April 18 - May 1, 2021 Tuesday, May 4, 2021 by 4:00 p.m. 14-May-21 12 Jun-21 5 11 May 2 - May 15, 2021 Tuesday, May 18, 2021 by 4:00 p.m. 28-May-21 12 May 16 - May 29, 2021 Tuesday, June 1, 2021 by 4:00 p.m. 11-Jun-21 Jul-21 6 13 May 30 - June 12, 2021 Tuesday, June 15, 2021 by 4:00 p.m. -

BILLING CYCLE SCHEDULE Department of Procurement, Disbursements & Contract Services 1135 Old Main 600 Lincoln Avenue Charleston, IL 61920
Eastern Illinois University BILLING CYCLE SCHEDULE Department of Procurement, Disbursements & Contract Services 1135 Old Main 600 Lincoln Avenue Charleston, IL 61920 Billing Cycle Beginning Date Billing Cycle Ending Date June 26, 2018 July 25, 2018 Tuesday Wednesday July 26, 2018 August 24, 2018 Thursday Friday August 26, 2018 September 25, 2018 Sunday Tuesday September 26, 2018 October 25, 2018 Wednesday Thursday October 26, 2018 November 26, 2018 Friday Monday November 27, 2018 December 26, 2018 Tuesday Wednesday December 27, 2018 January 25, 2019 Thursday Friday January 26, 2019 February 25, 2019 Saturday Monday February 26, 2019 March 25, 2019 Tuesday Monday March 26, 2019 April 25, 2019 Tuesday Thursday April 26, 2019 May 24, 2019 Friday Friday May 26, 2019 June 25, 2019 Sunday Tuesday June 26, 2019 July 25, 2019 Wednesday Thursday Revised 2/2/18 1 Transactions with a Post Date of: Must be Reviewed Upload to Banner & Approved by: July 1, 2018 – July 6, 2018 July 12, 2018 July 13, 2018 Thursday Friday July 7, 2018 – July 13, 2018 July 19, 2018 July 20, 2018 Thursday Friday July 14, 2018 – July 20, 2018 July 26, 2018 July 27, 2018 Thursday Friday July 21, 2018 – July 27, 2018 August 2, 2018 August 3, 2018 Thursday Friday July 28, 2018 – August 3, 2018 August 9, 2018 August 10, 2018 Thursday Friday August 4, 2018 – August 10, 2018 August 16, 2018 August 17, 2018 Thursday Friday August 11, 2018 – August 17, 2018 August 23, 2018 August 24, 2018 Thursday Friday August 18, 2018 – August 24, 2018 August 30, 2018 August 31, 2018 Thursday -

University Senate – October 5, 2020
University Senate – October 5, 2020 University Senate Meeting Minutes October 5, 2020 3:00 - 5:00 p.m. IN ATTENDANCE: Miguel Barbosa, Terry Barry, Paul Bartoli, Andra Basu, Nurun Begum, Bill Broun, Elijah Brown, Joanne Bruno, Marguerite Carver, Kevin Casebolt, Robert Cohen, Ginger Coleman, Darla Darno, Susan Dillmuth-Miller, Caroline Dipipi-Hoy, Christopher Domanski, Johan Eliasson, Rene Fuanta, James Galdieri, Heather Garrison, Melissa Geiger, Diane Holben, Hoen Kim, Brooke Langan, Eun-Joo Lee, Kenneth Long, Karen Lucas, Andi McClanahan, Margaret Mullan, Erin O’Donnell, Mary Frances Postupack, Millie Roman-Buday, Melinda Rosen, Jessica Santiago, Elizabeth Scott, Denise Seigart, Leigh Smith, Robert Smith, Brandon Snyder, Tom Tauer, Nancy VanArsdale, Kelly Varcoe, Daisy Wang, Samantha Williams, Sylvester Williams, Xuemao Zhang ABSENT: Lonnie Allbaugh, Lorraine Arocho, Jill Boyle, Michele Conners, Kevin Davis, Brenda Friday, William Green, Eric Hunt, Shelby Jimcosky, Minkyo Lee, Clare Lenhart, Jevon Mitchell, Al Moranville, Richard Otto, Mariah Ranton, Albert Rivera, Arshad Rivers, Santiago Solis, Loreylinnette Trinidad, Shawn Watkins, Amani Yeboah, Xiaochen Zhou Roll Call 1) Review of September 2020 Minutes Approved with attendance changes made to minutes 2) University President’s Report: No report. 3) Fix the Agenda – no changes to the agenda. 4) Committee reports: a) Executive Committee – open discussion topics added to agenda. b) Rules and By-Laws – meeting to be scheduled c) Student Affairs – Decided on four goals for the academic year 20-21. i) Exploring mental health resources for students. Will be developing a survey to evaluate student counseling and psychological services. A subcommittee will review survey results and develop next steps. ii) Improving marketing and communication across campus. -

Federal Register/Vol. 85, No. 193/Monday, October 5, 2020
Federal Register / Vol. 85, No. 193 / Monday, October 5, 2020 / Rules and Regulations 62583 AIRAC date State City Airport FDC No. FDC date Subject 5–Nov–20 ..... AK St Mary’s ................. St Mary’s ................................. 0/6456 8/28/20 RNAV (GPS) RWY 35, Amdt 2D. 5–Nov–20 ..... MN Princeton ................. Princeton Muni ........................ 0/6742 9/8/20 RNAV (GPS) RWY 33, Orig-B. 5–Nov–20 ..... MN Princeton ................. Princeton Muni ........................ 0/6743 9/8/20 RNAV (GPS) RWY 15, Orig-C. 5–Nov–20 ..... AK Willow ..................... Willow ...................................... 0/7081 8/26/20 RNAV (GPS) RWY 13, Orig. 5–Nov–20 ..... AK Willow ..................... Willow ...................................... 0/7082 8/26/20 RNAV (GPS) RWY 31, Orig. 5–Nov–20 ..... NE Columbus ................ Columbus Muni ....................... 0/7087 8/31/20 RNAV (GPS) RWY 14, Orig-C. 5–Nov–20 ..... NE Columbus ................ Columbus Muni ....................... 0/7088 8/31/20 RNAV (GPS) RWY 32, Orig-B. 5–Nov–20 ..... NE Columbus ................ Columbus Muni ....................... 0/7089 8/31/20 LOC/DME RWY 14, Amdt 8C. 5–Nov–20 ..... NE Columbus ................ Columbus Muni ....................... 0/7090 8/31/20 VOR RWY 14, Amdt 14D. 5–Nov–20 ..... NE Columbus ................ Columbus Muni ....................... 0/7091 8/31/20 VOR RWY 32, Amdt 14C. 5–Nov–20 ..... HI Kapolei .................... Kalaeloa (John Rodgers Field) 0/7363 8/28/20 VOR/DME RWY 4R, Amdt 1. 5–Nov–20 ..... WI Eau Claire ............... Chippewa Valley Rgnl ............. 0/7631 9/1/20 ILS OR LOC RWY 22, Amdt 10. 5–Nov–20 ..... KS Ottawa .................... Ottawa Muni ............................ 0/8061 8/31/20 RNAV (GPS) RWY 17, Amdt 2. -
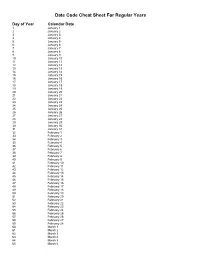
Julian Date Cheat Sheet for Regular Years
Date Code Cheat Sheet For Regular Years Day of Year Calendar Date 1 January 1 2 January 2 3 January 3 4 January 4 5 January 5 6 January 6 7 January 7 8 January 8 9 January 9 10 January 10 11 January 11 12 January 12 13 January 13 14 January 14 15 January 15 16 January 16 17 January 17 18 January 18 19 January 19 20 January 20 21 January 21 22 January 22 23 January 23 24 January 24 25 January 25 26 January 26 27 January 27 28 January 28 29 January 29 30 January 30 31 January 31 32 February 1 33 February 2 34 February 3 35 February 4 36 February 5 37 February 6 38 February 7 39 February 8 40 February 9 41 February 10 42 February 11 43 February 12 44 February 13 45 February 14 46 February 15 47 February 16 48 February 17 49 February 18 50 February 19 51 February 20 52 February 21 53 February 22 54 February 23 55 February 24 56 February 25 57 February 26 58 February 27 59 February 28 60 March 1 61 March 2 62 March 3 63 March 4 64 March 5 65 March 6 66 March 7 67 March 8 68 March 9 69 March 10 70 March 11 71 March 12 72 March 13 73 March 14 74 March 15 75 March 16 76 March 17 77 March 18 78 March 19 79 March 20 80 March 21 81 March 22 82 March 23 83 March 24 84 March 25 85 March 26 86 March 27 87 March 28 88 March 29 89 March 30 90 March 31 91 April 1 92 April 2 93 April 3 94 April 4 95 April 5 96 April 6 97 April 7 98 April 8 99 April 9 100 April 10 101 April 11 102 April 12 103 April 13 104 April 14 105 April 15 106 April 16 107 April 17 108 April 18 109 April 19 110 April 20 111 April 21 112 April 22 113 April 23 114 April 24 115 April -
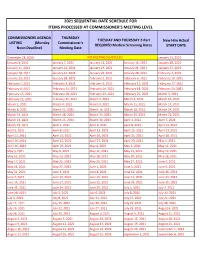
2021 Sequential Date List
2021 SEQUENTIAL DATE SCHEDULE FOR ITEMS PROCESSED AT COMMISSIONER'S MEETING LEVEL COMMISSIONERS AGENDA THURSDAY TUESDAY AND THURSDAY 2-Part New Hire Actual LISTING (Monday Commissioner's REQUIRED Medical Screening Dates START DATE Noon Deadline) Meeting Date December 28, 2020 NO MEETING SCHEDULED January 13, 2021 January 4, 2021 January 7, 2021 January 12, 2021 January 14, 2021 January 20, 2021 January 11, 2021 January 14, 2021 January 19, 2021 January 21, 2021 January 27, 2021 January 18, 2021 January 21, 2021 January 26, 2021 January 28, 2021 February 3, 2021 January 25, 2021 January 28, 2021 February 2, 2021 February 4, 2021 February 10, 2021 February 1, 2021 February 4, 2021 February 9, 2021 February 11, 2021 February 17, 2021 February 8, 2021 February 11, 2021 February 16, 2021 February 18, 2021 February 24, 2021 February 15, 2021 February 18, 2021 February 23, 2021 February 25, 2021 March 3, 2021 February 22, 2021 February 25, 2021 March 2, 2021 March 4, 2021 March 10, 2021 March 1, 2021 March 4, 2021 March 9, 2021 March 11, 2021 March 17, 2021 March 8, 2021 March 11, 2021 March 16, 2021 March 18, 2021 March 24, 2021 March 15, 2021 March 18, 2021 March 23, 2021 March 25, 2021 March 31, 2021 March 22, 2021 March 25, 2021 March 30, 2021 April 1, 2021 April 7, 2021 March 29, 2021 April 1, 2021 April 6, 2021 April 8, 2021 April 14, 2021 April 5, 2021 April 8, 2021 April 13, 2021 April 15, 2021 April 21, 2021 April 12, 2021 April 15, 2021 April 20, 2021 April 22, 2021 April 28, 2021 April 19, 2021 April 22, 2021 April 27, 2021 April -
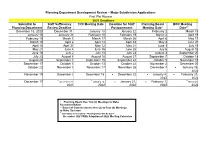
2021 Subdivision Calendar
Planning Department Development Review – Major Subdivision Applications First Plat Review 2021 Deadlines Submittal to Staff Sufficiency TRC Meeting Date Deadline for Staff Planning Board BOC Meeting Planning Department Review Deadline Postponement Meeting Date* Date** December 18, 2020 December 31 January 13 January 22 February 2 March 15 January 15 January 29 February 10 February 19 March 2 April 19 February 19 March 5 March 17 March 26 April 6 May 17 March 19 April 2 April 14 April 23 May 4 June 21 April 16 April 30 May 12 May 21 June 1 July 19 May 21 June 4 June 16 June 25 July 6 August 16 June 18 July 2 July 14 July 23 August 3 September 20 July 23 August 6 August 18 August 27 September 7 October 18 August 20 September 3 September 15 September 24 October 5 November 15 September 17 October 1 October 13 October 22 November 2 December 20 October 22 November 5 November 17 November 26 December 7 ▪ January 18, 2022 November 19 December 3 December 15 ▪ December 22 ▪ January 4, ▪ February 21, 2022 2022 ▪ ▪ ▪ December 17 December 31, January 12, ▪ January 21, ▪ February 1, March 21, 2021 2022 2022 2022 2022 * Planning Board Has Two (2) Meetings to Make Recommendation ** Board of Commissioners Has Up to Four (4) Meetings to Make Decision ▪ 2021 Dates are Tentative – Meeting Dates Will Be Set in December 2021 With Adoption of 2022 Meeting Calendars Construction/Final Plat Review – Administrative* 2021 Deadlines Submittal to Staff Sufficiency TRC Meeting Date Planning Review Deadline Department For TRC December 23, 2020 January 6 January 13 January -

2021 Rezoning Review Schedule
City of Waukee | 2021 ZONING AMENDMENT REVIEW SCHEDULE APPLICATION STAFF APPLICANT PUBLIC P & Z P & Z COUNCIL COUNCIL COUNCIL COUNCIL DUE COMMENTS REVISIONS by HEARING SUBMITTAL MEETING SUBMITTAL MEETING MEETING MEETING by 5:00 p.m. SENT 5:00 p.m. DATE SET by 5:00 p.m. 6:00 p.m. by 5:00 p.m. 5:30 p.m. 5:30 p.m. 5:30 p.m. 5:30 p.m. [1st Consider.] [2nd Consider.] [3rd Consider.] (TUES.) (TUES.) (TUES.) (MON.) (THUR.) (TUES.) (WED.) (MON.) (MON.) (MON.) November 17 November 24 December 1 December 7 December 17 December 22 December 30 January 4 January 18 February 1 December 8 December 15 December 22 December 21 January 7 January 12 January 13 January 18 February 1 *February 16* December 22 December 29 January 5 January 4 January 21 January 26 January 27 February 1 *February 16* March 1 January 5 January 12 January 19 January 18 February 4 February 9 February 10 *February 16* March 1 March 15 January 19 January 26 February 2 February 1 February 18 February 23 February 24 March 1 March 15 April 5 February 2 February 9 February 16 *February 16* March 4 March 9 March 10 March 15 April 5 April 19 February 16 February 23 March 2 March 1 March 18 March 23 March 31 April 5 April 19 May 3 March 2 March 9 March 16 March 15 April 8 April 13 April 14 April 19 May 3 May 17 March 16 March 23 March 30 April 5 April 22 April 27 April 28 May 3 May 17 June 7 March 30 April 6 April 13 April 19 May 6 May 11 May 12 May 17 June 7 June 21 April 13 April 20 April 27 May 3 May 20 May 25 June 2 June 7 June 21 *July 6* April 27 May 4 May 11 May 17 June 3 June 8 June -

Early Dance Division Session 1 2012-2013
Early Dance Division Session 1 2012-2013 *Classes will be held. Absences due to the holiday will be granted make-up class. Monday Classes Tuesday Classes September 10 Class September 11 Class September 17* Class September 18 Class September 24 Class September 25 Class October 1 Class October 2 Class October 8 Class October 9 Class October 15 Class October 16 Class October 22 Class October 23 Class October 29 Last Class October 30 Last Class Wednesday Classes Thursday Classes September 12 Class September 13 Class September 19 Class September 20 Class September 26* Class September 27 Class October 3 Class October 4 Class October 10 Class October 11 Class October 17 Class October 18 Class October 24 Class October 25 Class October 31 Last Class November 1 Last Class Friday Classes Saturday Classes September 14 Class September 8 Class September 21 Class September 15 Class September 28 Class September 22 Class October 5 Class September 29 Class October 12 Class October 6 Class October 19 Class October 13 Class October 26 Class October 20 Class November 2 Last Class October 27 Last Class Sunday Classes September 9 Class September 16 Class September 23 Class September 30 Class October 7 Class October 14 Class October 21 Class October 28 Last Class Early Dance Division Session 2 2012-2013 Monday Classes Tuesday Classes November 5 Class November 6 Class November 12 Class November 13 Class November 19 No Class November 20 No Class November 26 Class November 27 Class December 3 Class December 4 Class December 10 Class December 11 Class December 17