Quarterly Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THE CONCISE GUIDE to PHARMACOLOGY 2017/18 Alexander, Stephen P
University of Dundee THE CONCISE GUIDE TO PHARMACOLOGY 2017/18 Alexander, Stephen P. H.; Fabbro, Doriano; Kelly, Eamonn; Marrion, Neil V.; Peters, John A.; Faccenda, Elena Published in: British Journal of Pharmacology DOI: 10.1111/bph.13876 Publication date: 2017 Licence: CC BY Document Version Publisher's PDF, also known as Version of record Link to publication in Discovery Research Portal Citation for published version (APA): Alexander, S. P. H., Fabbro, D., Kelly, E., Marrion, N. V., Peters, J. A., Faccenda, E., Harding, S. D., Pawson, A. J., Sharman, J. L., Southan, C., Davies, J. A., & CGTP Collaborators (2017). THE CONCISE GUIDE TO PHARMACOLOGY 2017/18: Catalytic receptors. British Journal of Pharmacology, 174 (Suppl. 1), S225-S271. https://doi.org/10.1111/bph.13876 General rights Copyright and moral rights for the publications made accessible in Discovery Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from Discovery Research Portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain. • You may freely distribute the URL identifying the publication in the public portal. Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 23. Sep. 2021 S.P.H. -

Quantum of Effectiveness Evidence in FDA's Approval of Orphan Drugs
Quantum of Effectiveness Evidence in FDA’s Approval of Orphan Drugs Cataloguing FDA’s Flexibility in Regulating Therapies for Persons with Rare Disorders by Frank J. Sasinowski, M.S., M.P.H., J.D.1 Chairman of the Board National Organization for Rare Disorders One of the key underlying issues facing the development of effective for their intended uses. all drugs, and particularly orphan drugs, is what kind of evi- dence the Food and Drug Administration (FDA) requires for FDA has for many decades acknowledged that there is a need approval. The Federal Food, Drug, and Cosmetic [FD&C] Act IRUÁH[LELOLW\LQDSSO\LQJLWVVWDQGDUGIRUDSSURYDO)RUH[- provides that for FDA to grant approval for a new drug, there ample, one of FDA’s regulations states that: “FDA will ap- must be “substantial evidence” of effectiveness derived from prove an application after it determines that the drug meets the “adequate and well-controlled investigations.” This language, statutory standards for safety and effectiveness… While the which dates from 1962, provides leeway for FDA medical re- statutory standards apply to all drugs, the many kinds of drugs viewers to make judgments as to what constitutes “substantial that are subject to the statutory standards and the wide range HYLGHQFHµRIDGUXJ·VHIIHFWLYHQHVVWKDWLVRILWVEHQHÀWWR RIXVHVIRUWKRVHGUXJVGHPDQGÁH[LELOLW\LQDSSO\LQJWKHVWDQ- patients. GDUGV7KXV)'$LVUHTXLUHGWRH[HUFLVHLWVVFLHQWLÀFMXGJPHQW to determine the kind and quantity of data and information an 7KHVROHODZWKDWDSSOLHVVSHFLÀFDOO\WRRUSKDQGUXJVWKH2U- applicant is required to provide for a particular drug to meet SKDQ'UXJ$FWRISURYLGHGÀQDQFLDOLQFHQWLYHVIRUGUXJ the statutory standards.” 21 C.F.R. § 314.105(c). FRPSDQLHVWRGHYHORSRUSKDQGUXJVZKLFKLVOHJDOO\GHÀQHG as products that treat diseases that affect 200,000 or fewer )'$SXEOLFO\KDVH[SUHVVHGVHQVLWLYLW\WRDSSO\LQJWKLVÁH[- patients in the U.S. -
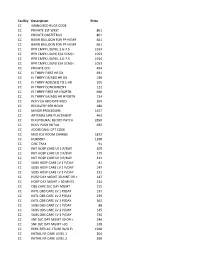
NMMC West Point CDM.Xlsx
Facility Description Price CC SWING BED RUGS CODE CC PRIVATE 1ST WEST 861 CC PRIVATE OBSTETRICS 861 CC BAKRI BALLOON FOR PP HEMR 661 CC BAKRI BALLOON FOR PP HEMR 661 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC PRIVATE ECU 494 CC IV THRPY FIRST HR DX 691 CC IV THRPY EA/ADD HR DX 190 CC IV THRPY ADD/SEQ TO 1 HR 205 CC IV THRPY CONCURRENT 122 CC IV THRPY FIRST HR HYDRTN 690 CC IV THRPY EA/ADD HR HYDRTN 134 CC INJ IV EA ADD DIFF MED 269 CC RECOVERY PER HOUR 280 CC MINOR PROCEDURE 1627 CC ARTERIAL LINE PLACEMENT 463 CC INJ EPIDURAL BLOOD PATCH 2850 CC INJ IV PUSH INITIAL 692 CC ADDITIONAL CPT CODE CC MED ICU ROOM CHARGE 1872 CC NURSERY 1200 CC CIRC TRAY 91 CC INIT HOSP CARE LV 1 P/DAY 205 CC INIT HOSP CARE LV 2 P/DAY 279 CC INIT HOSP CARE LV 3 P/DAY 412 CC SUBS HOSP CARE LV 1 P/DAY 81 CC SUBS HOSP CARE LV 2 P/DAY 147 CC SUBS HOSP CARE LV 3 P/DAY 212 CC HOSP DAY MGMT 30 MNT OR < 147 CC HOSP DAY MGMT > 30 MNTS 214 CC OBS CARE D/C DAY MGMT 155 CC INITL OBS CARE LV 1 P/DAY 197 CC INITL OBS CARE LV 2 P/DAY 239 CC INITL OBS CARE LV 3 P/DAY 362 CC SUBS OBS CARE LV 1 P/DAY 88 CC SUBS OBS CARE LV 2 P/DAY 145 CC SUBS OBS CARE LV 3 P/DAY 236 CC SNF D/C DAY MGMT 30 OR < 240 CC SNF D/C DAY MGMT >30 318 CC PERC REPLAC J TUBE W/O FL 1948 CC INITIAL NF CARE LEVEL 1 204 CC INITIAL NF CARE LEVEL 2 290 CC INITIAL NF CARE LEVEL 3 368 CC SUBSQENT NF CARE LEVEL 197 CC SUBSQENT NF CARE LEVEL 2 151 CC SUBSQENT NF CARE LEVEL 3 198 CC SUBSQENT NF CARE LEVEL 4 295 CC OBS OR I/P -

Monitoring and Mathematical Modeling of in Vitro Human Megakaryocyte Expansion and Maturation Dynamics
YOUNES LEYSI-DERILOU MONITORING AND MATHEMATICAL MODELING OF IN VITRO HUMAN MEGAKARYOCYTE EXPANSION AND MATURATION DYNAMICS Thèse présentée à la Faculté des études supérieures de l’Université Laval dans le cadre du programme de doctorat en génie chimique pour l’obtention du grade de Philosophiae doctor (Ph.D.) DEPARTMENT DE GÉNIE CHIMIQUE FACULTÉ DE SCIENCES ET GÉNIE UNIVERSITÉ LAVAL QUÉBEC 2011 © Younes Leysi-Derilou, 2011 ii Résumé La mégakaryopoïèse est un processus complexe, qui prend naissance à partir des cellules souches hématopoïétiques (HSC). Ces dernières se différencient par étapes successives en mégakaryocytes (MKs) qui, suite à leur maturation, libèrent les plaquettes. Afin de modéliser le sort des HSCs lors de la mégakaryopoïèse en culture, un nouveau modèle mathématique a été développé, basé sur un programme de différenciation tridimensionnelle (3-D) où chaque sous-population est représentée par un compartiment. Dans le but d’évaluer la prolifération, la différenciation des MKs immatures puis matures, la cinétique de mort cellulaire ainsi que le nombre de plaquettes produites, à partir des cellules de sang de cordon (CB) ombilical enrichies en CD34+, un ensemble d'équations différentielles a été déployé. Les cellules CD34+ ont été placées en culture dans un milieu optimisé pour la différenciation mégakaryocytaire. Les paramètres cinétiques ont été estimés pour deux températures d'incubation (37°C versus 39°C). Les résultats des régressions ont été validés par l'évaluation de l'estimabilité des paramètres, en utilisant des analyses de sensibilité locale et globale, puis la détermination d'un intervalle de confiance. Ceux-ci ont été comparés par le biais de tests statistiques et d’analyses en composante principale (ACP). -

CDER List of Licensed Biological Products With
Center for Drug Evaluation and Research List of Licensed Biological Products with (1) Reference Product Exclusivity and (2) Biosimilarity or Interchangeability Evaluations to Date DATE OF FIRST REFERENCE PRODUCT DATE OF LICENSURE LICENSURE EXCLUSIVITY EXPIRY DATE INTERCHANGEABLE (I)/ BLA STN PRODUCT (PROPER) NAME PROPRIETARY NAME (mo/day/yr) (mo/day/yr) (mo/day/yr) BIOSIMILAR (B) WITHDRAWN 125118 abatacept Orencia 12/23/05 NA NA 103575 abciximab ReoPro 12/22/94 NA NA Yes 125274 abobotulinumtoxinA Dysport 04/29/09 125057 adalimumab Humira 12/31/02 NA NA 761071 adalimumab-adaz Hyrimoz 10/30/18 B 761058 adalimumab-adbm Cyltezo 08/25/17 B 761118 adalimumab-afzb Abrilada 11/15/19 B 761024 adalimumab-atto Amjevita 09/23/16 B 761059 adalimumab-bwwd Hadlima 07/23/19 B 125427 ado-trastuzumab emtansine Kadcyla 02/22/13 125387 aflibercept Eylea 11/18/11 103979 agalsidase beta Fabrazyme 04/24/03 NA NA 125431 albiglutide Tanzeum 04/15/14 017835 albumin chromated CR-51 serum Chromalbin 02/23/76 103293 aldesleukin Proleukin 05/05/92 NA NA 103948 alemtuzumab Campath, Lemtrada 05/07/01 NA NA 125141 alglucosidase alfa Myozyme 04/28/06 NA NA 125291 alglucosidase alfa Lumizyme 05/24/10 125559 alirocumab Praluent 07/24/15 103172 alteplase, cathflo activase Activase 11/13/87 NA NA 103950 anakinra Kineret 11/14/01 NA NA 020304 aprotinin Trasylol 12/29/93 125513 asfotase alfa Strensiq 10/23/15 101063 asparaginase Elspar 01/10/78 NA NA 125359 asparaginase erwinia chrysanthemi Erwinaze 11/18/11 761034 atezolizumab Tecentriq 05/18/16 761049 avelumab Bavencio 03/23/17 -

Evaluating the Effect of Oprelvekin on Cardiac Repolarization in Subjects with Chemotherapy-Induced Thrombocytopenia: an Observa
Journal of Case Reports and Studies Volume 5 | Issue 2 ISSN: 2348-9820 Case Report Open Access Evaluating the Effect of Oprelvekin on Cardiac Repolarization in Subjects with Chemotherapy-Induced Thrombocytopenia: An Observational Chart Review of a Phase 2 Clinical Trial in Laredo, Texas Soriano RA*1 and Gonzalez M2 1The London School of Economics and Political Science, London, UK 2Envision Clinical Research, LLC, Laredo Texas 78041, USA *Corresponding author: Soriano RA, The London School of Economics and Political Science, London, UK, E-mail: [email protected] Citation: Soriano RA, Gonzalez M (2017) Evaluating the Effect of Oprelvekin on Cardiac Repolarization in Subjects with Chemotherapy-Induced Thrombocytopenia: An Observational Chart Review of a Phase 2 Clinical Trial in Laredo, Texas. J Case Rep Stud 5(2): 204. doi: 10.15744/2348-9820.5.204 Received Date: March 05, 2017 Accepted Date: April 26, 2017 Published Date: April 28, 2017 Abstract This study tested for the cardiac effects of Oprelvekin, recombinant human interleukin-11, a thrombopoietic growth factor, in patients afflicted with chemotherapy-induced thrombocytopenia (platelet count<50,000 cells/ul). Chart-reviews of patients fulfilling the inclusion criteria of: 18-75 yrs of age, non-myeloid malignancy, with adequate hematologic, hepatic and renal parameters and normal electrocardiograms that were enrolled in this phase 2 trial were analyzed. Patients of child-bearing potential agreed to be on a reliable form of birth control for the duration of the study. Results on 4 patients suggest that Oprelvekin does not cause atrial nor ventricular arrhythmia, a rare severe cardiac side effect, in treating patients with chemotherapy-induced thrombocytopenia. -

Standard Specialty PA and QL List January 2015
Standard Specialty PA and QL List January 2015 Standard PA or PA with QL Programs Therapeutic Category Drug Name Quantity Limit Anti-infectives Antiretrovirals, Hepatitis B BARACLUDE (entecavir) 1 tab/day BARACLUDE (entecavir) Soln 630 ml/30days HEPSERA (adefovir) 1 tab/day TYZEKA (telbivudine ) 1 tab/day Antiretrovirals, HIV FUZEON (enfuvirtide) 60 vials or 1 kit/30 days SELZENTRY (maraviroc) None TRUVADA (emtricitabine/tenofovir) None Cardiology Antilipemic JUXTAPID (lomitapide) 20 mg 3 tabs/day JUXTAPID (lomitapide) 5 mg, 10 mg 1 tab/day KYNAMRO (mipomersen) 4 syringes/28 days Pulmonary Arterial Hypertension ADCIRCA (tadalafil) 2 tabs/day ADEMPAS (riociguat) 90 tabs/30 days FLOLAN (epoprostenol) None LETAIRIS (ambrisentan) 1 tab/day OPSUMIT (macitentan) 1 tab/day ORENITRAM (treprostinil diolamine) None REMODULIN (treprostinil) None REVATIO (sildenafil) 3 tabs or vials/day TRACLEER (bosentan) 2 tabs/day TYVASO (treprostinil) 1 ampule/day VELETRI (epoprostenol) None VENTAVIS (iloprost) 9 ampules/day Vasopressors NORTHERA (droxidopa) None Central Nervous System Anticonvulsants SABRIL (vigabatrin) None Depressant XYREM (sodium oxybate) 3 bottles (540 mL)/30 days Neurotoxins BOTOX (onabotulinumtoxinA) None DYSPORT (abobotulinumtoxinA) None MYOBLOC (rimabotulinumtoxinB) None XEOMIN (incobotulinumtoxinA) None Parkinson's APOKYN (apomorphine) None Sleep Disorder HETLIOZ (tasimelteon) 1 cap/day Dermatology Alkylating Agents VALCHLOR (mechlorethamine) Gel None Endocrinology & Metabolism Gonadotropins ELIGARD (leuprolide) 22.5 mg (3-month) 1 -

Pharmacology of Recombinant Or Genetically Engineered Drugs
Pharmacology Pharmacology of Recombinant or Genetically Engineered Drugs Kamal Kishore, Pawan Krishan1 Departments of Pharmacy, M.J.P. Rohilkhand University, Bareilly-243 006, Uttar Pradesh, 1Pharmaceutical Sciences and Drug Research, Punjabi University, Patiala-147 002, Punjab, India Address for correspondence: Dr. Kamal Kishore; E-mail: [email protected] ABSTRACT Recombinant technology or genetic engineering is a modern method used for the synthesis of therapeutic agents. The central theme of recombinant technology is the process of “gene cloning” which consists of the production of a deÞ ned fragment of DNA and its propagation and ampliÞ cation in a suitable host cell. Drugs developed by recombinant technology or genetic engineering are known as biologics, biopharmaceuticals, recombinant DNA expressed products, bioengineered, or genetically engineered drugs. A current list of various products developed by recombinant technology includes erythropoietin, coagulation modulators, enzymes, hormones, interferons, interleukins, granulocyte colony-stimulating factors, anti-rheumatoid drugs, and various other agents like TNF, becaplermin, hepatitis-B vaccine, antibodies etc. This article provides general as well as recent pharmacological information on different aspects of recombinant drugs that may be useful for their better understanding by users and health care professionals. Key words: Biologics, erythropoietin, interferon, interleukins, insulin, thrombolytic enzymes DOI: 10.4103/0975-1483.55747 INTRODUCTION fragment of DNA and its propagation and ampliÞ cation in a suitable host cell. Recombinant technology was only Drugs developed using living organisms with the help of possible after the discovery of restriction endonucleases, biotechnology or genetic engineering are known as biologics, the enzymes used as cutters for a desired segment[3] of biopharmaceuticals, recombinant DNA expressed genes known as recognition sequences. -

Specialty Pharmacy Drug List
Specialty Pharmacy Drug List The Specialty Drug List applies to Members that have a “Specialty Drug Tier” under their pharmacy benefit. Check Plan documents for your benefits. Drugs indicated with a (SP) are required to be obtained from a Health Net contracted Specialty Pharmacy and are not available out of network, through Mail Order, or for an extended days supply. SPECIALTY DRUGS Arthritis / Psoriasis Brand Generic Name Comments ACTEMRA 162MG SYRINGE (N) TOCILIZUMAB SUB Q PRIOR AUTHORIZATION REQUIRED ENBREL (N) ETANERCEPT PRIOR AUTHORIZATION REQUIRED HUMIRA (N) ADALIMUMAB PRIOR AUTHORIZATION REQUIRED CIMZIA (EST) (N) CERTOLIZUMAB PEGOL PRIOR AUTHORIZATION REQUIRED KINERET (EST) (N) ANAKINRA PRIOR AUTHORIZATION REQUIRED METHOTREXATE (N) METHOTREXATE PRIOR AUTHORIZATION REQUIRED ORENCIA SUB Q 125MG/ML (N) ABATACEPT PRIOR AUTHORIZATION REQUIRED OTEZLA TABLETS (N) APREMILAST PRIOR AUTHORIZATION REQUIRED SIMPONI (N) GOLIMUMAB PRIOR AUTHORIZATION REQUIRED XELJANZ TABLETS (PA) (QL) TOFACITINIB PRIOR AUTHORIZATION REQUIRED Blood Modifiers Brand Generic Name Comments ARANESP (EST) (N) DARBEPOETIN ALFA-ALBUMIN PRIOR AUTHORIZATION REQUIRED EPOGEN (EST) (N) EPOETIN ALFA PRIOR AUTHORIZATION REQUIRED GRANIX (EST (N) TBO-FILGRASTIM PRIOR AUTHORIZATION REQUIRED Methoxy Polyethylene Glycol-Epoetin Beta MIRCERA (N) PRIOR AUTHORIZATION REQUIRED Injection NEULASTA (EST) (N) PEGFILGRASTIM PRIOR AUTHORIZATION REQUIRED NEUMEGA (N) OPRELVEKIN PRIOR AUTHORIZATION REQUIRED NEUPOGEN (N) FILGRASTIM PRIOR AUTHORIZATION REQUIRED PROCRIT (N) EPOETIN ALFA PRIOR AUTHORIZATION -

Medications Requiring Prior Authorization
Medications Requiring Prior Authorization IU Health Pharmacy Benefits Management 950 N Meridian Street, Suite 600, Indianapolis, IN 46204 Phone: 317-963-3347 877-769-0191 Prior Auth Fax: 866-429-8920 These infusions and injections require authorization prior to administering. Medical claims billed using these J-codes will not pay without prior authorization. Brand Generic HCPCS Code Immune Suppressants Blood Formation Products Cimzia certolizumab pegol J0718 Aranesp darbepoetin alfa J0881, J0882 Enbrel etanercept J1438 Epogen Humira adalimumab J0135 epoetin alfa J0885, J0886 Procrit Orencia abatacept J0129 Leukine sargramostim J2820 Remicade infliximab J1745 Neulasta pegfilgrastim J2505 Simponi golimumab J3590, C9399 Neumega oprelvekin J2355 Immunomodulators Neupogen filgrastim J1441, J1440 Actimmune interferon gamma-1b J9216 Dermatologic Agents Alferon N interferon alfa-n3 J9215 Regranex becaplermin S0157 J1826, Q3025, Avonex Interferon beta-1a Stelara ustekinumab J3357 Q3026 Enzyme Replacement/Modifiers Betaseron Interferon beta-1b J1830 Cerezyme imiglucerase J1786 Copaxone glatiramer J1595 Hormonal Modifiers Infergen interferon alfacon-1 J9212 Eligard, J9217, J9218, Intron-A interferon alfa-2b J9214 leuprolide Lupron J9219, J1950 Kineret anakinra J3590 Genotropin Pegasys peginterferon alfa-2a J3590 Humatrope Peg-Intron peginterferon alfa-2b J3590 Norditropin J3590,Q3026, Nutropin Rebif interferon beta-1a somatropin J2941 C9399 Omnitrope Interferon alfa-2b & Saizen Rebetron J9214, J8499 Serostim ribavirin Zorbtive Synagis palivizumab -

Biopharmaceutical Benchmarks 2018
FEATURE Biopharmaceutical benchmarks 2018 Gary Walsh Monoclonal antibodies (mAbs) continue to reign supreme, although cellular and gene therapies are slowly starting to gather momentum. Burgeoning growth in biosimilars may threaten future brand monopolies for mAbs and other biologics. ntibodies continue to dominate biophar- a Amaceutical approvals, but new nucleic 70 36 acid modalities and cellular therapies are US 28 also slowly launching on the market. This 60 EU article provides an update on three previous surveys of biopharmaceutical approvals1–3. 50 19 The current survey period (January 2014 23 19 to July 2018) witnessed the approval of 155 40 14 17 biopharmaceutical products (see Table 1 20 for definition) in the United States and/or 30 European Union, when counted by product trade name. Some products contain identical 20 active ingredients or are sold under different Number of product approvals trade names in the two regions. Taking this 10 into account, 129 distinct biopharmaceutical active ingredients entered the market. 0 With these new approvals, the number of 2014 2015 2016 2017 individual biopharmaceutical products hav- Year ing gained a license in these regions now b totals 374, containing 285 distinct active bio- 120 pharmaceutical ingredients. However, over 112 the years, 58 products have been withdrawn 100 from the market following approval in one or 80 both regions, almost always for commercial 60 reasons. When withdrawals are taken into 60 58 56 54 account, the number of individual biopharma- 40 ceutical products with current active licenses stands at 316 (Table 1). 20 16 9 Annual approval numbers over the cur- Number of product approvals 0 rent survey period ranged from a low of 14 in Up to 1989 1990–1994 1995–1999 2000–2004 2005–2009 2010–2014 2015–July 2018 Europe in 2014 to a high of 36, also in Europe, Time period in 2017 (Fig. -

INN Working Document 05.179 Update December 2010
INN Working Document 05.179 Update December 2010 International Nonproprietary Names (INN) for biological and biotechnological substances (a review) INN Working Document 05.179 Distr.: GENERAL ENGLISH ONLY 12/2010 International Nonproprietary Names (INN) for biological and biotechnological substances (a review) Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Essential Medicines and Pharmaceutical Policies (EMP) International Nonproprietary Names (INN) for biological and biotechnological substances (a review) © World Health Organization 2010 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters.