CARM1 Inhibition Enables Immunotherapy of Resistant Tumors by Dual Action on Tumor Cells and T Cells
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Data
Figure 2S 4 7 A - C 080125 CSCs 080418 CSCs - + IFN-a 48 h + IFN-a 48 h + IFN-a 72 h 6 + IFN-a 72 h 3 5 MRFI 4 2 3 2 1 1 0 0 MHC I MHC II MICA MICB ULBP-1 ULBP-2 ULBP-3 ULBP-4 MHC I MHC II MICA MICB ULBP-1 ULBP-2 ULBP-3 ULBP-4 7 B 13 080125 FBS - D 080418 FBS - + IFN-a 48 h 12 + IFN-a 48 h + IFN-a 72 h + IFN-a 72 h 6 080125 FBS 11 10 5 9 8 4 7 6 3 MRFI 5 4 2 3 2 1 1 0 0 MHC I MHC II MICA MICB ULBP-1 ULBP-2 ULBP-3 ULBP-4 MHC I MHC II MICA MICB ULBP-1 ULBP-2 ULBP-3 ULBP-4 Molecule Molecule FIGURE 4S FIGURE 5S Panel A Panel B FIGURE 6S A B C D Supplemental Results Table 1S. Modulation by IFN-α of APM in GBM CSC and FBS tumor cell lines. Molecule * Cell line IFN-α‡ HLA β2-m# HLA LMP TAP1 TAP2 class II A A HC§ 2 7 10 080125 CSCs - 1∞ (1) 3 (65) 2 (91) 1 (2) 6 (47) 2 (61) 1 (3) 1 (2) 1 (3) + 2 (81) 11 (80) 13 (99) 1 (3) 8 (88) 4 (91) 1 (2) 1 (3) 2 (68) 080125 FBS - 2 (81) 4 (63) 4 (83) 1 (3) 6 (80) 3 (67) 2 (86) 1 (3) 2 (75) + 2 (99) 14 (90) 7 (97) 5 (75) 7 (100) 6 (98) 2 (90) 1 (4) 3 (87) 080418 CSCs - 2 (51) 1 (1) 1 (3) 2 (47) 2 (83) 2 (54) 1 (4) 1 (2) 1 (3) + 2 (81) 3 (76) 5 (75) 2 (50) 2 (83) 3 (71) 1 (3) 2 (87) 1 (2) 080418 FBS - 1 (3) 3 (70) 2 (88) 1 (4) 3 (87) 2 (76) 1 (3) 1 (3) 1 (2) + 2 (78) 7 (98) 5 (99) 2 (94) 5 (100) 3 (100) 1 (4) 2 (100) 1 (2) 070104 CSCs - 1 (2) 1 (3) 1 (3) 2 (78) 1 (3) 1 (2) 1 (3) 1 (3) 1 (2) + 2 (98) 8 (100) 10 (88) 4 (89) 3 (98) 3 (94) 1 (4) 2 (86) 2 (79) * expression of APM molecules was evaluated by intracellular staining and cytofluorimetric analysis; ‡ cells were treatead or not (+/-) for 72 h with 1000 IU/ml of IFN-α; # β-2 microglobulin; § β-2 microglobulin-free HLA-A heavy chain; ∞ values are indicated as ratio between the mean of fluorescence intensity of cells stained with the selected mAb and that of the negative control; bold values indicate significant MRFI (≥ 2). -

Meta-Analysis of Nasopharyngeal Carcinoma
BMC Genomics BioMed Central Research article Open Access Meta-analysis of nasopharyngeal carcinoma microarray data explores mechanism of EBV-regulated neoplastic transformation Xia Chen†1,2, Shuang Liang†1, WenLing Zheng1,3, ZhiJun Liao1, Tao Shang1 and WenLi Ma*1 Address: 1Institute of Genetic Engineering, Southern Medical University, Guangzhou, PR China, 2Xiangya Pingkuang associated hospital, Pingxiang, Jiangxi, PR China and 3Southern Genomics Research Center, Guangzhou, Guangdong, PR China Email: Xia Chen - [email protected]; Shuang Liang - [email protected]; WenLing Zheng - [email protected]; ZhiJun Liao - [email protected]; Tao Shang - [email protected]; WenLi Ma* - [email protected] * Corresponding author †Equal contributors Published: 7 July 2008 Received: 16 February 2008 Accepted: 7 July 2008 BMC Genomics 2008, 9:322 doi:10.1186/1471-2164-9-322 This article is available from: http://www.biomedcentral.com/1471-2164/9/322 © 2008 Chen et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: Epstein-Barr virus (EBV) presumably plays an important role in the pathogenesis of nasopharyngeal carcinoma (NPC), but the molecular mechanism of EBV-dependent neoplastic transformation is not well understood. The combination of bioinformatics with evidences from biological experiments paved a new way to gain more insights into the molecular mechanism of cancer. Results: We profiled gene expression using a meta-analysis approach. Two sets of meta-genes were obtained. Meta-A genes were identified by finding those commonly activated/deactivated upon EBV infection/reactivation. -
CPSF6 Links Alternative Polyadenylation to Metabolism
Tan et al. Journal of Experimental & Clinical Cancer Research (2021) 40:85 https://doi.org/10.1186/s13046-021-01884-z RESEARCH Open Access CPSF6 links alternative polyadenylation to metabolism adaption in hepatocellular carcinoma progression Sheng Tan1†, Ming Zhang2†, Xinglong Shi3†, Keshuo Ding4, Qiang Zhao3, Qianying Guo4, Hao Wang4, Zhengsheng Wu4, Yani Kang3, Tao Zhu5*, Jielin Sun1* and Xiaodong Zhao1* Abstract Background: Alternative polyadenylation (APA) is an important mechanism of gene expression regulation through generation of RNA isoforms with distinct 3′ termini. Increasing evidence has revealed that APA is actively involved in development and disease, including hepatocellular carcinoma (HCC). However, how APA functions in tumor formation and progression remains elusive. In this study, we investigated the role of cleavage factor I (CFIm) subunit CPSF6 in human hepatocellular carcinoma (HCC). Methods: Expression levels of CPSF6 in clinical tissues and cell lines were determined by qRT-PCR and western blot. Functional assays, including the cell number, MTT, colony formation and transwell, were used to determine the oncogenic role of CPSF6 in HCC. Animal experiments were used to determine the role of CPSF6 in HCC tumorigenicity in vivo. Deep sequencing-based 3 T-seq was used to profile the transcriptome-wide APA sites in both HCC cells and CPSF6 knockdown HCC cells. The function of CPSF6-affected target NQO1 with distinct 3′UTRs was characterized by metabolism assays. Results: We observed CPSF6 was upregulated in HCC and the high expression of CPSF6 was associated with poor prognosis in patients. Overexpression of CPSF6 promoted proliferation, migration and invasion of HCC cells in vitro and in vivo. -

Loss of Fam60a, a Sin3a Subunit, Results in Embryonic Lethality and Is Associated with Aberrant Methylation at a Subset of Gene
RESEARCH ARTICLE Loss of Fam60a, a Sin3a subunit, results in embryonic lethality and is associated with aberrant methylation at a subset of gene promoters Ryo Nabeshima1,2, Osamu Nishimura3,4, Takako Maeda1, Natsumi Shimizu2, Takahiro Ide2, Kenta Yashiro1†, Yasuo Sakai1, Chikara Meno1, Mitsutaka Kadota3,4, Hidetaka Shiratori1†, Shigehiro Kuraku3,4*, Hiroshi Hamada1,2* 1Developmental Genetics Group, Graduate School of Frontier Biosciences, Osaka University, Suita, Japan; 2Laboratory for Organismal Patterning, RIKEN Center for Developmental Biology, Kobe, Japan; 3Phyloinformatics Unit, RIKEN Center for Life Science Technologies, Kobe, Japan; 4Laboratory for Phyloinformatics, RIKEN Center for Biosystems Dynamics Research, Kobe, Japan Abstract We have examined the role of Fam60a, a gene highly expressed in embryonic stem cells, in mouse development. Fam60a interacts with components of the Sin3a-Hdac transcriptional corepressor complex, and most Fam60a–/– embryos manifest hypoplasia of visceral organs and die in utero. Fam60a is recruited to the promoter regions of a subset of genes, with the expression of these genes being either up- or down-regulated in Fam60a–/– embryos. The DNA methylation level of the Fam60a target gene Adhfe1 is maintained at embryonic day (E) 7.5 but markedly reduced at –/– *For correspondence: E9.5 in Fam60a embryos, suggesting that DNA demethylation is enhanced in the mutant. [email protected] (SK); Examination of genome-wide DNA methylation identified several differentially methylated regions, [email protected] (HH) which were preferentially hypomethylated, in Fam60a–/– embryos. Our data suggest that Fam60a is †These authors contributed required for proper embryogenesis, at least in part as a result of its regulation of DNA methylation equally to this work at specific gene promoters. -

2020 Program Book
PROGRAM BOOK Note that TAGC was cancelled and held online with a different schedule and program. This document serves as a record of the original program designed for the in-person meeting. April 22–26, 2020 Gaylord National Resort & Convention Center Metro Washington, DC TABLE OF CONTENTS About the GSA ........................................................................................................................................................ 3 Conference Organizers ...........................................................................................................................................4 General Information ...............................................................................................................................................7 Mobile App ....................................................................................................................................................7 Registration, Badges, and Pre-ordered T-shirts .............................................................................................7 Oral Presenters: Speaker Ready Room - Camellia 4.......................................................................................7 Poster Sessions and Exhibits - Prince George’s Exhibition Hall ......................................................................7 GSA Central - Booth 520 ................................................................................................................................8 Internet Access ..............................................................................................................................................8 -

Inherited Variation in Mir-290 Expression Suppresses Breast Cancer Progression by Targeting the Metastasis Susceptibility Gene Arid4b
Published OnlineFirst February 27, 2013; DOI: 10.1158/0008-5472.CAN-12-3513 Cancer Tumor and Stem Cell Biology Research Inherited Variation in miR-290 Expression Suppresses Breast Cancer Progression by Targeting the Metastasis Susceptibility Gene Arid4b Natalie Goldberger1, Renard C. Walker1, Chang Hee Kim2, Scott Winter1, and Kent W. Hunter1 Abstract The metastatic cascade is a complex and extremely inefficient process with many potential barriers. Understanding this process is of critical importance because the majority of cancer mortality is associated with metastatic disease. Recently, it has become increasingly clear that microRNAs (miRNA) play important roles in tumorigenesis and metastasis, yet few studies have examined how germline variations may dysregulate miRNAs, in turn affecting metastatic potential. To explore this possibility, the highly metastatic MMTV-PyMT mice were crossed with 25 AKXD (AKR/J Â DBA/2J) recombinant inbred strains to produce F1 progeny with varying metastatic indices. When mammary tumors from the F1 progeny were analyzed by miRNA microarray, miR-290 (containing miR-290-3p and miR-290-5p) was identified as a top candidate progression-associated miRNA. The microarray results were validated in vivo when miR-290 upregulation in two independent breast cancer cell lines suppressed both primary tumor and metastatic growth. Computational analysis identified breast cancer progression gene Arid4b as a top target of miR-290-3p, which was confirmed by luciferase reporter assay. Surprisingly, pathway analysis identified estrogen receptor (ER) signaling as the top canonical pathway affected by miR-290 upregulation. Further analysis showed that ER levels were elevated in miR-290–expressing tumors and positively correlated with apoptosis. -

Multiple MYO18A-PDGFRB Fusion Transcripts in a Myeloproliferative
Sheng et al. Molecular Cytogenetics (2017) 10:4 DOI 10.1186/s13039-017-0306-8 CASEREPORT Open Access Multiple MYO18A-PDGFRB fusion transcripts in a myeloproliferative neoplasm patient with t(5;17)(q32;q11) Guangying Sheng1†, Zhao Zeng1†, Jinlan Pan1, Linbing Kou1, Qinrong Wang1, Hong Yao1, Lijun Wen1, Liang Ma1, Depei Wu1,2, Huiying Qiu1 and Suning Chen1,2* Abstract Background: Myeloproliferative neoplasms (MPNs), typically defined by myeloid proliferation and eosinophilia, and are only rarely caused by platelet-derived growth factor receptor beta (PDGFRB) gene rearrangements. Case presentation: Here, we report a unique case of MPN that is negative for eosinophilia and characterized by a novel PDGFRB rearrangement. After cytogenetic analysis revealed a karyotype of t(5;17) (q32;q11), we used fluorescence in situ hybridization to specifically identify the PDGFRB gene at 5q31-q33 as the gene that had been translocated. Subsequently, RNA sequencing identified a new MYO18A-PDGFRB gene fusion. This fusion presented a previously undescribed breakpoint composed of exon 37 of MYO18A and exon 13 of PDGFRB. Furthermore, both RT-PCR and Bi-directional Sanger sequencing confirmed this out-of-frame fusion. Interestingly, we simultaneously identified the presence of another three PDGFRB transcripts, all of which were in-frame fusions. After treating the patient with imatinib, the t(5;17) translocation was no longer detected by conventional cytogenetics or by FISH, and at the time of the last follow-up, the patient had been in complete remission for 26 months. Conclusion: We prove that MYO18A-PDGFRB fusions are recurrent genetic aberrations involved in MPNs, and identify multiple fusion transcripts with novel breakpoints. -

Arginine Methylation Facilitates the Recruitment of TOP3B to Chromatin to Prevent R Loop Accumulation
Molecular Cell Article Arginine Methylation Facilitates the Recruitment of TOP3B to Chromatin to Prevent R Loop Accumulation Yanzhong Yang,1 Kevin M. McBride,1 Sean Hensley,1 Yue Lu,1 Frederic Chedin,2 and Mark T. Bedford1,* 1The University of Texas MD Anderson Cancer Center, P.O. Box 389, Smithville, TX 78957, USA 2Department of Molecular & Cellular Biology, The University of California at Davis, Davis, CA 95616, USA *Correspondence: [email protected] http://dx.doi.org/10.1016/j.molcel.2014.01.011 SUMMARY nine methyltransferase 1), which deposit the H4R3me2a and H3R17me2a marks, respectively (Yang and Bedford, 2013). Tudor domain-containing protein 3 (TDRD3) is a Both of these marks are recognized by the Tudor domain of major methylarginine effector molecule that reads TDRD3 (Yang et al., 2010), a protein that is enriched at the pro- methyl-histone marks and facilitates gene transcrip- moters of highly transcribed genes and can likely also associate tion. However, the underlying mechanism by which with the C-terminal domain (CTD) of RNA Polymerase II (RNAP II) TDRD3 functions as a transcriptional coactivator is (Sims et al., 2011). TDRD3 has no enzymatic activity of its unknown. We identified topoisomerase IIIB (TOP3B) own, but here we show that it is tightly complexed with DNA topoisomerase IIIb (TOP3B), an interaction that bestows, in as a component of the TDRD3 complex. TDRD3 part, coactivator activity on TDRD3. TOP3B is a member of serves as a molecular bridge between TOP3B and the 1A subfamily of DNA topoisomerases and, as such, targets arginine-methylated histones. The TDRD3-TOP3B underwound or negatively supercoiled DNA (Wang, 2002). -

Variation in Protein Coding Genes Identifies Information
bioRxiv preprint doi: https://doi.org/10.1101/679456; this version posted June 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Animal complexity and information flow 1 1 2 3 4 5 Variation in protein coding genes identifies information flow as a contributor to 6 animal complexity 7 8 Jack Dean, Daniela Lopes Cardoso and Colin Sharpe* 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Institute of Biological and Biomedical Sciences 25 School of Biological Science 26 University of Portsmouth, 27 Portsmouth, UK 28 PO16 7YH 29 30 * Author for correspondence 31 [email protected] 32 33 Orcid numbers: 34 DLC: 0000-0003-2683-1745 35 CS: 0000-0002-5022-0840 36 37 38 39 40 41 42 43 44 45 46 47 48 49 Abstract bioRxiv preprint doi: https://doi.org/10.1101/679456; this version posted June 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Animal complexity and information flow 2 1 Across the metazoans there is a trend towards greater organismal complexity. How 2 complexity is generated, however, is uncertain. Since C.elegans and humans have 3 approximately the same number of genes, the explanation will depend on how genes are 4 used, rather than their absolute number. -

A Case of Acute Myeloid Leukemia with Promyelocytic Features Characterized by Expression of a Novel RARG-CPSF6 Fusion Christopher A
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2018 A case of acute myeloid leukemia with promyelocytic features characterized by expression of a novel RARG-CPSF6 fusion Christopher A. Miller Washington University School of Medicine in St. Louis Christopher Tricarico Washington University School of Medicine in St. Louis Zachary L. Skidmore Washington University School of Medicine in St. Louis Geoffrey L. Uy Washington University School of Medicine in St. Louis Yi-Shan Lee Washington University School of Medicine in St. Louis See next page for additional authors Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Recommended Citation Miller, Christopher A.; Tricarico, Christopher; Skidmore, Zachary L.; Uy, Geoffrey L.; Lee, Yi-Shan; Hassan, Anjum; O'Laughlin, Michelle D.; Schmidt, Heather; Tian, Ling; Duncavage, Eric J.; Griffith,al M achi; Griffith, Obi L.; Welch, John S.; and Wartman, Lukas D., ,"A case of acute myeloid leukemia with promyelocytic features characterized by expression of a novel RARG-CPSF6 fusion." Blood Advances.2,11. 1295-1299. (2018). https://digitalcommons.wustl.edu/open_access_pubs/7234 This Open Access Publication is brought to you for free and open access by Digital Commons@Becker. It has been accepted for inclusion in Open Access Publications by an authorized administrator of Digital Commons@Becker. For more information, please contact [email protected]. Authors Christopher A. Miller, Christopher Tricarico, Zachary L. Skidmore, Geoffrey L. Uy, Yi-Shan Lee, Anjum Hassan, Michelle D. O'Laughlin, Heather Schmidt, Ling Tian, Eric J. Duncavage, Malachi Griffith, Obi L. Griffith,o J hn S. Welch, and Lukas D. Wartman This open access publication is available at Digital Commons@Becker: https://digitalcommons.wustl.edu/open_access_pubs/7234 EXCEPTIONAL CASE REPORT A case of acute myeloid leukemia with promyelocytic features characterized by expression of a novel RARG-CPSF6 fusion Christopher A. -
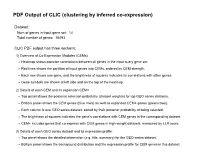
PDF Output of CLIC (Clustering by Inferred Co-Expression)
PDF Output of CLIC (clustering by inferred co-expression) Dataset: Num of genes in input gene set: 14 Total number of genes: 16493 CLIC PDF output has three sections: 1) Overview of Co-Expression Modules (CEMs) Heatmap shows pairwise correlations between all genes in the input query gene set. Red lines shows the partition of input genes into CEMs, ordered by CEM strength. Each row shows one gene, and the brightness of squares indicates its correlations with other genes. Gene symbols are shown at left side and on the top of the heatmap. 2) Details of each CEM and its expansion CEM+ Top panel shows the posterior selection probability (dataset weights) for top GEO series datasets. Bottom panel shows the CEM genes (blue rows) as well as expanded CEM+ genes (green rows). Each column is one GEO series dataset, sorted by their posterior probability of being selected. The brightness of squares indicates the gene's correlations with CEM genes in the corresponding dataset. CEM+ includes genes that co-express with CEM genes in high-weight datasets, measured by LLR score. 3) Details of each GEO series dataset and its expression profile: Top panel shows the detailed information (e.g. title, summary) for the GEO series dataset. Bottom panel shows the background distribution and the expression profile for CEM genes in this dataset. Overview of Co-Expression Modules (CEMs) with Dataset Weighting Scale of average Pearson correlations Num of Genes in Query Geneset: 14. Num of CEMs: 1. 0.0 0.2 0.4 0.6 0.8 1.0 Cpsf3l Polr2b Ints3 Ints7 Ints1 Ints4 Ints9 Ints2 -

This Thesis Has Been Submitted in Fulfilment of the Requirements for a Postgraduate Degree (E.G
This thesis has been submitted in fulfilment of the requirements for a postgraduate degree (e.g. PhD, MPhil, DClinPsychol) at the University of Edinburgh. Please note the following terms and conditions of use: This work is protected by copyright and other intellectual property rights, which are retained by the thesis author, unless otherwise stated. A copy can be downloaded for personal non-commercial research or study, without prior permission or charge. This thesis cannot be reproduced or quoted extensively from without first obtaining permission in writing from the author. The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the author. When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given. The CX3CR1/CX3CL1 Axis Drives the Migration and Maturation of Oligodendroglia in the Central Nervous System Catriona Ford Thesis Submitted for the Degree of Doctor of Philosophy The University of Edinburgh 2017 Abstract In the central nervous system, the axons of neurons are protected from damage and aided in electrical conductivity by the myelin sheath, a complex of proteins and lipids formed by oligodendrocytes. Loss or damage to the myelin sheath may result in impairment of electrical axonal conduction and eventually to neuronal death. Such demyelination is responsible, at least in part, for the disabling neurodegeneration observed in pathologies such as Multiple Sclerosis (MS) and Spinal Cord Injury. In the regenerative process of remyelination, oligodendrocyte precursor cells (OPCs), the resident glial stem cell population of the adult CNS, migrate toward the injury site, proliferate and differentiate into adult oligodendrocytes which subsequently reform the myelin sheath.