Blood Bank Manual 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guidelines for Transfusions
Guidelines for Transfu- sion Prepared by: Community Transfusion Committee Lincoln, Nebraska CHAIR: Aina Silenieks, MD MEMBERS: L. Bausch, M.D. R. Burton, M.D. S. Dunder, M.D. D. Voigt, M.D. B. J. Wilson, M.D. COMMUNITY Becky Croner REPRESENTATIVES: Ellen DiSalvo Christa Engel Phyllis Ericson Kelly Gillaspie Pat Gilles Vic Grdina Jessica Henrichs Kelly Jensen Laurel McReynolds Christina Nickel Angela Novotny Kelley Thiemann Janet Wachter Jodi Wikoff Guidelines For Transfusion Community Transfusion Committee INTRODUCTION The Community Transfusion Committee is a multidisciplinary group that meets to monitor blood utilization practices, establish guidelines for transfusion and discuss relevant transfusion related topics. It is comprised of physicians from local hospitals, invited guests, and community representatives from the hospitals’ transfusion services, nursing services, perfusion services, health information management, and the Nebraska Community Blood Bank. These Guidelines for Transfusion are reviewed and revised biannually by the Community Trans- fusion Committee to ensure that the industry’s most current practices are promoted. The Guidelines are the standard by which utilization practices are evaluated. They are also de- signed to provide helpful information to assist physicians to provide appropriate blood compo- nent therapy to patients. Appendices have been added for informational purposes and are not to be used as guidance for clinical decision making. ADULT RED CELLS A. Indications 1. One of the following a. Hypovolemia and hypoxia (signs/symptoms: syncope, dyspnea, postural hypoten- sion, tachycardia, angina, or TIA) secondary to surgery, trauma, GI tract bleeding, or intravascular hemolysis, OR b. Evidence of acute loss of 15% of total blood volume or >750 mL blood loss, OR c. -

27. Clinical Indications for Cryoprecipitate And
27. CLINICAL INDICATIONS FOR CRYOPRECIPITATE AND FIBRINOGEN CONCENTRATE Cryoprecipitate is indicated in the treatment of fibrinogen deficiency or dysfibrinogenaemia.1 Fibrinogen concentrate is licenced for the treatment of acute bleeding episodes in patients with congenital fibrinogen deficiency, including afibrinogenaemia and hypofibrinogenaemia,2 and is currently funded under the National Blood Agreement. Key messages y Fibrinogen is an essential component of the coagulation system, due to its role in initial platelet aggregation and formation of a stable fibrin clot.3 y The decision to transfuse cryoprecipitate or fibrinogen concentrate to an individual patient should take into account the relative risks and benefits.3 y The routine use of cryoprecipitate or fibrinogen concentrate is not advised in medical or critically ill patients.2,4 y Cryoprecipitate or fibrinogen concentrate may be indicated in critical bleeding if fibrinogen levels are not maintained using FFP. In the setting of major obstetric haemorrhage, early administration of cryoprecipitate or fibrinogen concentrate may be necessary.3 Clinical implications y The routine use of cryoprecipitate or fibrinogen concentrate in medical or critically ill patients with coagulopathy is not advised. The underlying causes of coagulopathy should be identified; where transfusion is considered necessary, the risks and benefits should be considered for each patient. Specialist opinion is advised for the management of disseminated intravascular coagulopathy (MED-PP18, CC-PP7).2,4 y Cryoprecipitate or fibrinogen concentrate may be indicated in critical bleeding if fibrinogen levels are not maintained using FFP. In patients with critical bleeding requiring massive transfusion, suggested doses of blood components is 3-4g (CBMT-PP10)3 in adults or as per the local Massive Transfusion Protocol. -

Transfusion Service Introduction Blood/Blood Products Requests and Turnaround Time Expectations
Transfusion Service Introduction All blood products and blood components are supplied to UnityPoint Health-Meriter Hospital by the American Red Cross Blood Services. Pathology consultation is available regarding blood and/or components and dosages. ABO and Rho(D)—specific type is used whenever possible for leuko-poor packed cell transfusions. ABO-compatible blood is used for all plasma and platelet components whenever possible. For any orders involving HLA-matched components, the patient must have been HLA typed (sent to the American Red Cross) a minimum of 48 hours prior to intended infusion of the component. HLA typing is only required once. Blood components that are thawed, pooled, washed, volume-reduced, or deglycerolized for a patient will be charged to the patient even if not transfused. The charge is done because these components may not be suitable for another patient. Examples include: Autologous or directed donations Pooled cryoprecipitate 4-hour expiration Thawed fresh frozen plasma 24-hour expiration Thawed cryoprecipitate 6-hour expiration Deglycerolized red cells 24-hour expiration Washed red cells 24-hour expiration All blood components must be completely infused within 4 hours of release from UnityPoint Health-Meriter Laboratories Blood Bank, or be infused within the expiration time. Refer to UnityPoint Health -Meriter’s Blood and Blood Products Transfusion Policy #123 for additional information located on MyMeriter. Blood/Blood Products Requests and Turnaround Time Expectations Requests from UnityPoint Health-Meriter Hospital are entered in the hospital computer system and print in the UnityPoint Health- Meriter Laboratories Blood Bank. For the comfort of the patient, it is important to coordinate collection for other tests with Blood Bank specimens. -

Factors Affecting Mobilization of Peripheral Blood Progenitor Cells in Patients with Lymphoma’
Vol. 4, 311-316, February 1998 Clinical Cancer Research 311 Factors Affecting Mobilization of Peripheral Blood Progenitor Cells in Patients with Lymphoma’ Craig H. Moskowitz,2 Jill R. Glassman, (median, 13 versus 22 days; P 0.06). Patients who received 1l cycles of chemotherapy prior to PBPC mobilization David Wuest, Peter Maslak, Lilian Reich, tended to have delayed platelet recovery to >20,090/&l and Anthony Gucciardo, Nancy Coady-Lyons, to require more platelet transfusions than less extensively Andrew D. Zelenetz, and Stephen D. Nimer pretreated patients (median, 13.5 versus 23.5 days; P 0.15; Division of Hematologic Oncology, Department of Medicine median number of platelet transfusion episodes, 13 versus 9; [C. H. M., D. W., P. M., L. R., A. G., N. C-L., A. D. Z., S. D. N.] and P = 0.17). Department of Biostatistics [J. R. G.], Memorial Sloan-Kettering Cancer Center, New York, New York 10021 These data suggest that current strategies to mobilize PBPCs may be suboptimal in patients who have received either stem cell-toxic chemotherapy or 11 cycles of chem- ABSTRACT otherapy prior to PBPC mobilization. Alternative ap- The objective of this study was to identify factors asso- proaches, such as ex vivo expansion or the use of other ciated with poor mobilization of peripheral blood progenitor growth factors in addition to G-CSE, may improve mobili- cells (PBPCs) or delayed platelet engraftment after high- zation of progenitor cells for PBPC transplantation. dose therapy and autologous stem cell transplantation in patients with lymphoma. INTRODUCTION Fifty-eight patients with Hodgkin’s disease or non- The use of high-dose chemoradiotherapy supported by Hodgkin’s lymphoma underwent PBPC transplantation as cryopreserved autologous hematopoietic progenitor cells is ef- the “best available therapy” at Memorial Sloan-Kettering fective in treating relapsed HD3 and NHL; a high complete Cancer Center (New York, NY) between 1993 and 1995. -

Blood Product Replacement: Obstetric Hemorrhage
CMQCC OBSTETRIC HEMORRHAGE TOOLKIT Version 2.0 3/24/15 BLOOD PRODUCT REPLACEMENT: OBSTETRIC HEMORRHAGE Richard Lee, MD, Los Angeles County and University of Southern California Medical Center Laurence Shields, MD, Marian Regional Medical Center/Dignity Health Holli Mason, MD, Cedars-Sinai Medical Center Mark Rollins, MD, PhD, University of California, San Francisco Jed Gorlin, MD, Innovative Blood Resources/Memorial Blood Center, St. Paul, Minnesota Maurice Druzin, MD, Lucile Packard Children’s Hospital Stanford University Jennifer McNulty, MD, Long Beach Memorial Medical Center EXECUTIVE SUMMARY • Outcomes are improved with early and aggressive intervention. • Both emergency blood release and massive transfusion protocols should be in place. • In the setting of significant obstetric hemorrhage, resuscitation transfusion should be based on vital signs and blood loss and should not be delayed by waiting for laboratory results. • Calcium replacement will often be necessary with massive transfusion due to the citrate used for anticoagulation in blood products. • During massive transfusion resuscitation, the patient’s arterial blood gas, electrolytes, and core temperature should be monitored to guide clinical management and all transfused fluids should be warmed; direct warming of the patient should be initiated as needed to maintain euthermia and to avoid added coagulopathy. BACKGROUND AND LITERATURE REVIEW After the first several units of packed red blood cells (PRBCs) and in the face of continuing or worsening hemorrhage, aggressive transfusion therapy becomes critical. This report covers the experience with massive transfusion protocols. Lessons from military trauma units as well as civilian experience with motor vehicle accidents and massive obstetric hemorrhage have identified new principles such as earlier use of plasma (FFP/thawed plasma/plasma frozen within 24 hours/liquid plasma) and resuscitation transfusion while laboratory results are pending. -

Fresh Frozen Plasma in General Practice
Practical guide to using frozen and fresh frozen plasma in general practice Why every practice should keep a bag in the freezer Kit Sturgess; MA; VetMB; PhD; CertVR; DSAM; CertVC; FRCVS RCVS Recognised Specialist in Small Animal Medicine Advanced Practitioner in Veterinary Cardiology Introduction Keeping stock at reasonable levels in a practice is vital to good business management balancing the need to have a product available against the costs of keeping stock that is not used and potentially may go out of date and need to be replaced (as well as subtle small costs of space, stock taking, disposal of out-of-date product etc.). Practices need, therefore, to make decisions about preparedness for ‘what if’ scenarios and have protocols in place. The difficult question for many practices is how bizarre/uncommon should these scenarios be to warrant keeping a drug or treatment in stock or buying a specialist piece of equipment. This can only really be answered on an individual practice basis as it will depend on the type of cases seen as well as the likely ability of clients to want to pay if the treatment/investigation is expensive and the relationship with other local practices in terms of borrowing treatments or using equipment. It is also important to try and understand the value that a particular drug or treatment will have on morbidity and mortality of a particular condition and whether the patient could be referred onwards if necessary so not having calcium available if presented with a seizuring hypocalcaemic patient would be a significant issue in that patient’s care. -
Platelet Transfusion
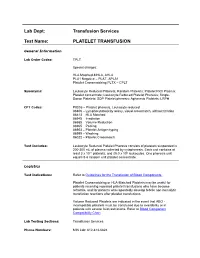
Lab Dept: Transfusion Services Test Name: PLATELET TRANSFUSION General Information Lab Order Codes: TPLT Special charges: HLA Matched-MHLA, AHLA PLA1 Negative – PLAT, APLA1 Platelet Crossmatching PLTX – CPLT Synonyms: Leukocyte Reduced Platelets; Random Platelets; Platelet Rich Plasma; Platelet concentrate; Leukocyte Reduced Platelet Pheresis; Single- Donor Platelets; SDP Platelet pheresis; Apheresis Platelets; LRPH CPT Codes: P9035 – Platelet pheresis, Leukocyte reduced 86806 – Lymphocytotoxicity assay, visual crossmatch, without titration 86813 – HLA Matched 86945 – Irradiation 86985 – Volume Reduction 86965 – Pooling 86903 – Platelet Antigen typing 86999 – Washing 86022 – Platelet Crossmatch Test Includes: Leukocyte Reduced Platelet Pheresis consists of platelets suspended in 200-300 mL of plasma collected by cytapheresis. Each unit contains at least 3 x 1011 platelets, and ≤5.0 x 106 leukocytes. One pheresis unit equals 5-6 random unit platelet concentrate. Logistics Test Indications: Refer to Guidelines for the Transfusion of Blood Components. Platelet Crossmatching or HLA-Matched Platelets may be useful for patients receiving repeated platelet transfusions who have become refractile, and for patients who repeatedly develop febrile non-hemolytic transfusion reactions after platelet transfusions. Volume Reduced Platelets are indicated in the event that ABO - incompatible platelets must be transfused due to availability or in patients with severe fluid restrictions. Refer to Blood Component Compatibility Chart Lab Testing Sections: Transfusion Services Phone Numbers: MIN Lab: 612-813-6824 STP Lab: 651-220-6558 Test Availability: Daily, 24 hours Turnaround Time: 1 - 2 hours Standard Dose/Volume: <10 kg: 10 – 15 mL/kg up to one unit or 50 mL maximum 10 – 15 kg: 1/3 pheresis unit 15 – 25 kg: 1/2 pheresis unit >25 kg: 1 pheresis unit Rate of Infusion: 10 minutes/unit, <4 hours Administration: Must be administered through a blood component administration filter. -

Blood Banking/Transfusion Medicine Fellowship Program
DEPARTMENT OF PATHOLOGY AND LABORATORY MEDICINE BLOOD BANKING/TRANSFUSION MEDICINE FELLOWSHIP PROGRAM THIS NEW ONE-YEAR ACGME-ACCREDITED FELLOWSHIP IN BLOOD BANKING/TRANSFUSION MEDICINE OFFERS STATE OF THE ART COMPREHENSIVE TRAINING IN BLOOD BANKING, COAGULATION, APHERESIS, AND HEMOTHERAPY AT THE MEMORIAL HERMANN HOSPITAL (MHH)-TEXAS MEDICAL CENTER (TMC) FOR PEDIATRICS AND ADULTS. This clinically-oriented fellowship is ideal for the candidate looking for exceptional experience in hemotherapy decision-making and coagulation consultation. We have a full spectrum of medical and surgical specialties, including a level 1 trauma center, as well as a busy solid organ transplant service (renal, liver, pancreas, cardiac, and lung). Fellows will rotate through: Our unique hemotherapy service: This innovative clinical consultative service for the Heart and Vascular Institute (HVI) allows fellows to serve as interventional blood banking consultants at the bed side as part of a multidisciplinary care team; our patients have complex bleeding and coagulopathy issues. Therapeutic apheresis service: This consultative service provide 24/7 direct patient care covering therapeutic plasmapheresis, red blood cell (RBC) exchanges, photopheresis, plateletpheresis, leukoreduction, therapeutic phlebotomies, and other related procedures on an inpatient and outpatient basis. We performed approximately over 1000 therapeutic plasma exchanges and RBC exchanges every year. Bloodbank: The MHH-TMC reference lab is one of the largest in Southeast Texas. This rotation provides extensive experience in interpreting antibody panel reports, working up transfusion reactions, investigating blood compatibility/incompatibility issues, and monitoring component usage. Gulf Coast Regional Blood Center: This rotation provides donor exposure in one of the largest community blood donation centers in the US as well as cellular therapy and immunohematology training. -

Apheresis Donation This Quick Reference Guide Will Help You Identify the Best Donation for Your Unique Blood Type
Apheresis Donation This quick reference guide will help you identify the best donation for your unique blood type. Donors now have the opportunity to make an apheresis (ay-fur-ee-sis) donation and donate just platelets, red cells, or plasma at blood drives. These individual components are vital for local patients in need. Platelets Control Bleeding Red Cells Deliver Oxygen Plasma transports blood cells & controls bleeding Donation Type Blood Types Requirements Donation Time A+, B+, O+ Over 75% of population has one of these blood types. Platelet Donation: Be healthy, weigh at least 114 lbs 2 hours cancer & surgery patients no aspirin for 48 hours Platelets only last five days after donation so the need is constant. O-, O+, A-, B- Special height, weight, Double Red: O-Negative is the 1 hour and hematocrit requirements. surgery, trauma patients, universal red cell donor. +25 min Please call us or see a staff member accident, & burn victims Only 17% of population has one of these negative blood types Plasma: AB+, AB- Trauma patients, burn Universal Plasma Donors 1 hour Be healthy, weigh at least 114 lbs victims, & patients with +30 min serious illness or injuries Only 4% of population How Apheresis works: Blood is drawn from the donor’s arm and the components are separated. Only the components being donated are collected while the remaining components are safely returned to the donor How to Schedule an Appointment: Please call 800-398-7888 or visit schedule.bloodworksnw.org. Walk-ins are also welcome at some blood drives, so be sure to ask our staff when you stop in. -

Blood Product Modifications: Leukofiltration, Irradiation and Washing
Blood Product Modifications: Leukofiltration, Irradiation and Washing 1. Leukocyte Reduction Definitions and Standards: o Process also known as leukoreduction, or leukofiltration o Applicable AABB Standards, 25th ed. Leukocyte-reduced RBCs At least 85% of original RBCs < 5 x 106 WBCs in 95% of units tested . Leukocyte-reduced Platelet Concentrates: At least 5.5 x 1010 platelets in 75% of units tested < 8.3 x 105 WBCs in 95% of units tested pH≥6.2 in at least 90% of units tested . Leukocyte-reduced Apheresis Platelets: At least 3.0 x 1011 platelets in 90% of units tested < 5.0 x 106 WBCs 95% of units tested pH≥6.2 in at least 90% of units tested Methods o Filter: “Fourth-generation” filters remove 99.99% WBCs o Apheresis methods: most apheresis machines have built-in leukoreduction mechanisms o Less efficient methods of reducing WBC content . Washing, deglycerolizing after thawing a frozen unit, centrifugation . These methods do not meet requirement of < 5.0 x 106 WBCs per unit of RBCs/apheresis platelets. Types of leukofiltration/leukoreduction o “Pre-storage” . Done within 24 hours of collection . May use inline filters at time of collection (apheresis) or post collection o “Pre-transfusion” leukoreduction/bedside leukoreduction . Done prior to transfusion . “Bedside” leukoreduction uses gravity-based filters at time of transfusion. Least desirable given variability in practice and absence of proficiency . Alternatively performed by transfusion service prior to issuing Benefits of leukoreduction o Prevention of alloimmunization to donor HLA antigens . Anti-HLA can mediate graft rejection and immune mediated destruction of platelets o Leukoreduced products are indicated for transplant recipients or patients who are likely platelet transfusion dependent o Prevention of febrile non-hemolytic transfusion reactions (FNHTR) . -

45 Part 606—Current Good Man- Ufacturing Practice
Food and Drug Administration, HHS Pt. 606 a presentation. The presiding officer ucts approved under § 601.91, the re- may, as a matter of discretion, permit strictions would no longer apply when questions to be submitted to the pre- FDA determines that safe use of the bi- siding officer for response by a person ological product can be ensured making a presentation. through appropriate labeling. FDA also (f) Judicial review. The Commissioner retains the discretion to remove spe- of Food and Drugs’ decision constitutes cific postapproval requirements upon final agency action from which the ap- review of a petition submitted by the plicant may petition for judicial re- sponsor in accordance with § 10.30 of view. Before requesting an order from a this chapter. court for a stay of action pending re- view, an applicant must first submit a PART 606—CURRENT GOOD MAN- petition for a stay of action under § 10.35 of this chapter. UFACTURING PRACTICE FOR BLOOD AND BLOOD COMPO- [67 FR 37996, May 31, 2002, as amended at 70 NENTS FR 14984, Mar. 24, 2005] § 601.93 Postmarketing safety report- Subpart A—General Provisions ing. Sec. Biological products approved under 606.3 Definitions. this subpart are subject to the post- marketing recordkeeping and safety Subpart B—Organization and Personnel reporting applicable to all approved bi- ological products. 606.20 Personnel. § 601.94 Promotional materials. Subpart C—Plant and Facilities For biological products being consid- 606.40 Facilities. ered for approval under this subpart, unless otherwise informed by the agen- Subpart D—Equipment cy, applicants must submit to the agency for consideration during the 606.60 Equipment. -

Red Blood Cells, Leukocyte Reduced Covenant and AHS Sites
This document applies to all Red Blood Cells, Leukocyte Reduced Covenant and AHS sites. Class: Human blood component, derived from OTHER NAMES: Packed red blood cells, Packed whole blood cells INTRAVENOUS OTHER ROUTES DIRECT IV Intermittent Continuous Infusion Infusion SC IM OTHER Acceptable No Yes No No No No Routes* * Professionals performing these restricted activities have received authorization from their regulatory college and have the knowledge and skill to perform the skill competently. DESCRIPTION OF PRODUCT: Red Blood Cell (RBC) concentrates are prepared from approximately 480mL whole blood usually collected in 70mL of anticoagulant. The unit is plasma reduced by centrifugation, platelet reduced by either centrifugation or filtration and leukocyte reduced by filtration. RBCs are typically resuspended in approximately 110mL of nutrient. Collected from volunteer donors by the Canadian Blood Services (CBS). Donor is screened and blood is tested for: i. Hepatitis B Surface Antigen (HBsAg) ii. Syphilis iii. Antibodies to Hepatitis B core antigen (HBcore), Hepatitis C Virus (HCV), Human T-cell Lymphotropic Virus (HTLV-1 and 2), Human Immune Deficiency Virus (HIV-1 and 2) iv. Nucleic Acid Testing (NAT) for presence of HCV RNA, HIV-1 RNA and West Nile Virus (WNV) RNA . CBS also tests blood for ABO/Rh and clinically significant antibodies. Some donors are tested for CMV status. RBCs do NOT contain any coagulation factors or platelets. AVAILABILITY: . Contact your local transfusion service/laboratory for ABO and Rh types stocked at your site. ABO compatible (not always identical) may be required if the transfusion service cannot provide sufficient quantities of the patient’s blood group (See ABO compatibility chart at: http://www.albertahealthservices.ca/assets/wf/lab/wf-lab-clin-tm-abo-compatability.pdf).