Reticular Dysgenesis and Mitochondriopathy Induced By
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Primate Specific Retrotransposons, Svas, in the Evolution of Networks That Alter Brain Function
Title: Primate specific retrotransposons, SVAs, in the evolution of networks that alter brain function. Olga Vasieva1*, Sultan Cetiner1, Abigail Savage2, Gerald G. Schumann3, Vivien J Bubb2, John P Quinn2*, 1 Institute of Integrative Biology, University of Liverpool, Liverpool, L69 7ZB, U.K 2 Department of Molecular and Clinical Pharmacology, Institute of Translational Medicine, The University of Liverpool, Liverpool L69 3BX, UK 3 Division of Medical Biotechnology, Paul-Ehrlich-Institut, Langen, D-63225 Germany *. Corresponding author Olga Vasieva: Institute of Integrative Biology, Department of Comparative genomics, University of Liverpool, Liverpool, L69 7ZB, [email protected] ; Tel: (+44) 151 795 4456; FAX:(+44) 151 795 4406 John Quinn: Department of Molecular and Clinical Pharmacology, Institute of Translational Medicine, The University of Liverpool, Liverpool L69 3BX, UK, [email protected]; Tel: (+44) 151 794 5498. Key words: SVA, trans-mobilisation, behaviour, brain, evolution, psychiatric disorders 1 Abstract The hominid-specific non-LTR retrotransposon termed SINE–VNTR–Alu (SVA) is the youngest of the transposable elements in the human genome. The propagation of the most ancient SVA type A took place about 13.5 Myrs ago, and the youngest SVA types appeared in the human genome after the chimpanzee divergence. Functional enrichment analysis of genes associated with SVA insertions demonstrated their strong link to multiple ontological categories attributed to brain function and the disorders. SVA types that expanded their presence in the human genome at different stages of hominoid life history were also associated with progressively evolving behavioural features that indicated a potential impact of SVA propagation on a cognitive ability of a modern human. -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

Genetic Features of Myelodysplastic Syndrome and Aplastic Anemia in Pediatric and Young Adult Patients
Bone Marrow Failure SUPPLEMENTARY APPENDIX Genetic features of myelodysplastic syndrome and aplastic anemia in pediatric and young adult patients Siobán B. Keel, 1* Angela Scott, 2,3,4 * Marilyn Sanchez-Bonilla, 5 Phoenix A. Ho, 2,3,4 Suleyman Gulsuner, 6 Colin C. Pritchard, 7 Janis L. Abkowitz, 1 Mary-Claire King, 6 Tom Walsh, 6** and Akiko Shimamura 5** 1Department of Medicine, Division of Hematology, University of Washington, Seattle, WA; 2Clinical Research Division, Fred Hutchinson Can - cer Research Center, Seattle, WA; 3Department of Pediatric Hematology/Oncology, Seattle Children’s Hospital, WA; 4Department of Pedi - atrics, University of Washington, Seattle, WA; 5Boston Children’s Hospital, Dana Farber Cancer Institute, and Harvard Medical School, MA; 6Department of Medicine and Department of Genome Sciences, University of Washington, Seattle, WA; and 7Department of Laboratory Medicine, University of Washington, Seattle, WA, USA *SBK and ASc contributed equally to this work **TW and ASh are co-senior authors ©2016 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2016.149476 Received: May 16, 2016. Accepted: July 13, 2016. Pre-published: July 14, 2016. Correspondence: [email protected] or [email protected] Supplementary materials Supplementary methods Retrospective chart review Patient data were collected from medical records by two investigators blinded to the results of genetic testing. The following information was collected: date of birth, transplant, death, and last follow-up, -

Understanding Brassicaceae Evolution Through Ancestral
Understanding Brassicaceae evolution through ancestral genome reconstruction Florent Murat, Alexandra Louis, Florian Maumus, Alix Armero Villanueva, Richard Cooke, Hadi Quesneville, Hugues Roest Crollius, Jerome Salse To cite this version: Florent Murat, Alexandra Louis, Florian Maumus, Alix Armero Villanueva, Richard Cooke, et al.. Understanding Brassicaceae evolution through ancestral genome reconstruction. Genome Biology, BioMed Central, 2015, 16 (262), 10.1186/s13059-015-0814-y. hal-01281832 HAL Id: hal-01281832 https://hal.archives-ouvertes.fr/hal-01281832 Submitted on 2 Mar 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Murat et al. Genome Biology (2015) 16:262 DOI 10.1186/s13059-015-0814-y RESEARCH Open Access Understanding Brassicaceae evolution through ancestral genome reconstruction Florent Murat1†, Alexandra Louis2,3,4†, Florian Maumus5†, Alix Armero1, Richard Cooke6, Hadi Quesneville5, Hugues Roest Crollius2,3,4 and Jerome Salse1* Abstract Background: Brassicaceae is a family of green plants of high scientific and economic interest, including thale cress (Arabidopsis thaliana), cruciferous vegetables (cabbages) and rapeseed. Results: We reconstruct an evolutionary framework of Brassicaceae composed of high-resolution ancestral karyotypes using the genomes of modern A. thaliana, Arabidopsis lyrata, Capsella rubella, Brassica rapa and Thellungiella parvula. -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

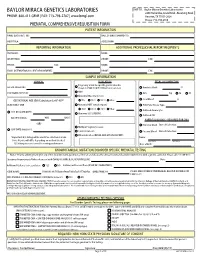
Molecular Diagnostic Requisition
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 MOLECULAR DIAGNOSTIC REQUISITION PATIENT INFORMATION SAMPLE INFORMATION NAME: DATE OF COLLECTION: / / LAST NAME FIRST NAME MI MM DD YY HOSPITAL#: ACCESSION#: DATE OF BIRTH: / / GENDER (Please select one): FEMALE MALE MM DD YY SAMPLE TYPE (Please select one): ETHNIC BACKGROUND (Select all that apply): UNKNOWN BLOOD AFRICAN AMERICAN CORD BLOOD ASIAN SKELETAL MUSCLE ASHKENAZIC JEWISH MUSCLE EUROPEAN CAUCASIAN -OR- DNA (Specify Source): HISPANIC NATIVE AMERICAN INDIAN PLACE PATIENT STICKER HERE OTHER JEWISH OTHER (Specify): OTHER (Please specify): REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: INDICATION FOR STUDY SYMPTOMATIC (Summarize below.): *FAMILIAL MUTATION/VARIANT ANALYSIS: COMPLETE ALL FIELDS BELOW AND ATTACH THE PROBAND'S REPORT. GENE NAME: ASYMPTOMATIC/POSITIVE FAMILY HISTORY: (ATTACH FAMILY HISTORY) MUTATION/UNCLASSIFIED VARIANT: RELATIONSHIP TO PROBAND: THIS INDIVIDUAL IS CURRENTLY: SYMPTOMATIC ASYMPTOMATIC *If family mutation is known, complete the FAMILIAL MUTATION/ VARIANT ANALYSIS section. NAME OF PROBAND: ASYMPTOMATIC/POPULATION SCREENING RELATIONSHIP TO PROBAND: OTHER (Specify clinical findings below): BMGL LAB#: A COPY OF ORIGINAL RESULTS ATTACHED IF PROBAND TESTING WAS PERFORMED AT ANOTHER LAB, CALL TO DISCUSS PRIOR TO SENDING SAMPLE. A POSITIVE CONTROL MAY BE REQUIRED IN SOME CASES. REQUIRED: NEW YORK STATE PHYSICIAN SIGNATURE OF CONSENT I certify that the patient specified above and/or their legal guardian has been informed of the benefits, risks, and limitations of the laboratory test(s) requested. -

Adenylate Kinase 2 / AK2 (1-239, His-Tag) Human Protein Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for AR09002PU-N Adenylate kinase 2 / AK2 (1-239, His-tag) Human Protein Product data: Product Type: Recombinant Proteins Description: Adenylate kinase 2 / AK2 (1-239, His-tag) human recombinant protein, 0.5 mg Species: Human Expression Host: E. coli Tag: His-tag Predicted MW: 28.6 kDa Concentration: lot specific Purity: >95% by SDS-PAGE Buffer: Presentation State: Purified State: Liquid purified protein Buffer System: 20 mM Tris pH 7.5, 5 mM DTT, 20% glycerol Bioactivity: Specific: > 1.5 units/ml One unit will convert 2.0 umoles of ADP to ATP + AMP per minute at pH 7.5 at 25°C. Endotoxin: < 1.0 EU per 1 µg of protein (determined by LAL method) Preparation: Liquid purified protein Applications: Protocol: Activity Assay 1. Prepare a 1.4 ml assay buffer (Assay buffer: 58 mM glycylglycine, 2.0 mM adenosine 5'- diphosphate, 2.3 mM beta-nicotinamide adenine dinucleotide phosphate, 10 mM magnesium chloride, 10 mM glucose, 2 unit hexokinase, 1 unit glucose-6-phosphate dehydrogenase, 0.003% (w/v) BSA, pH 7.5.) - G-6-PDH/Hex (sigma,Cat.No. H-8629) 2. Add 50 ul of recombinant Adenylate kinase isoenzyme 2 protein with various concentrations (0.5 ug, 1 ug) and read the increase in A340nm for 5 minutes. Protein Description: Recombinant human AK2 protein, fused to His-tag at N-terminus, was expressed in E.coli and purified by using conventional chromatography techniques. -

Immune Cellular Evaluation Following Newborn Screening for Severe T
In this issue: Clinical flow cytometry in 2019 This is a Platinum Open Access Journal distributed under the terms of the Creative Commons Attribution Non-Commercial License which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. Immune cellular evaluation following newborn screening for severe T and B cell lymphopenia Johannes Wolf1,2, Karolin Dahlenburg3, Stephan Borte2,4 1 Municipal Hospital St. Georg Leipzig, Academic Teaching Hospital of the University Leipzig, Department of Laboratory Medicine and Microbiology, Leipzig, Germany 2 Immuno Deficiency Center Leipzig (IDCL) at Hospital St. Georg Leipzig, Jeffrey Modell Diagnostic and Research Center for Primary Immunodeficiency Diseases, Leipzig, Germany 3 Faculty of Medicine, University Leipzig, Germany 4 Municipal Hospital St. Georg Leipzig, Academic Teaching Hospital of the University Leipzig, Department of Pediatrics, Leipzig, Germany ARTICLE INFO ABSTRACT Corresponding author: Newborn screening (NBS) for severe T and/or B cell Stephan Borte, MD, PhD Immuno Deficiency Center Leipzig (IDCL) lymphopenia to identify neonates with severe com- Hospital St. Georg Leipzig bined immunodeficiencies (SCID) or agammaglob- Delitzscher Strasse 141 ulinemia rapidly after birth has paved its way into D-04129 Leipzig clinical practice. Debate exists on the concept and Germany Phone: +49 341 909 4478 strategy for rapid verification and stratification of the E-mail: [email protected] cellular immune status of positively screened infants. We provide impulses for harmonization of flow cyto- Key words: newborn screening, T cell lymphopenia, metric approaches to allow rapid integration in the B cell lymphopenia, severe combined growing number of immunological laboratories in- immunodeficiency volved in follow-up and subdivision of SCID and non- Acknowledgement: SCID entities. -

Next-Generation Sequencing, FISH Mapping and Synteny- Based Modeling Reveal Mechanisms of Decreasing Dysploidy in Cucumis
The Plant Journal (2014) 77, 16–30 doi: 10.1111/tpj.12355 Next-generation sequencing, FISH mapping and synteny- based modeling reveal mechanisms of decreasing dysploidy in Cucumis Luming Yang1,†, Dal-Hoe Koo1,†, Dawei Li1,2, Tao Zhang1, Jiming Jiang1, Feishi Luan3, Susanne S. Renner4, Elizabeth Henaff 5, Walter Sanseverino6, Jordi Garcia-Mas6, Josep Casacuberta5, Douglas A. Senalik1,7, Philipp W. Simon1,7, Jinfeng Chen8 and Yiqun Weng1,7,* 1Horticulture Department, University of Wisconsin, Madison, WI 53706, USA, 2Horticulture College, Northwest A & F University, Yangling 712100, China, 3Horticulture College, Northeast Agricultural University, Harbin 150030, China, 4Department of Biology, University of Munich, 80638 Munich, Germany, 5Centre for Research in Agricultural Genomics Consejo Superior de Investigaciones Cientı´ficas-Institut de Recerca i Tecnolo- gia Agroalimenta` ries-Universitat Auto` noma de Barcelona-Universitat de Barcelona, 08193 Barcelona, Spain, 6Institut de Recerca i Tecnologia Agroalimenta` ries, Centre for Research in Agricultural Genomics Consejo Superior de Inves- tigaciones Cientı´ficas-Institut de Recerca i Tecnologia Agroalimenta` ries-Universitat Auto` noma de Barcelona-Universitat de Barcelona, 08193 Barcelona, Spain, 7US Department of Agriculture/Agricultural Research Service, Vegetable Crops Research Unit, 1575 Linden Drive, Madison, WI 53706, USA, and 8College of Horticulture, Nanjing Agricultural University, Nanjing 210095, China Received 27 July 2013; revised 7 October 2013; accepted 10 October 2013; published online 15 October 2013. *For correspondence (e-mail [email protected]). †These authors contributed equally to this work. SUMMARY In the large Cucurbitaceae genus Cucumis, cucumber (C. sativus) is the only species with 2n = 2x = 14 chro- mosomes. The majority of the remaining species, including melon (C. -

Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -

Blueprint Genetics Severe Combined Immunodeficiency Panel
Severe Combined Immunodeficiency Panel Test code: IM0101 Is a 80 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of combined immunodeficiencies. The genes on this panel are included in the Primary Immunodeficiency Panel. About Severe Combined Immunodeficiency Severe combined immunedeficiencies (SCIDs) are a group of primary immunodeficiencies characterized by specific mutations in genes of T and B-lymphocyte systems and leading to little or no immune response. Different subtypes of SCIDs are characterized and subdivided by the presence of circulating T and B cells. T cells are absent or markedly decreased in the most types, but levels of B cells vary. In addition, both of these disease subgroups (T-B+ and T-B-) can occur with or without NK cells. Patients with SCID are susceptible to recurrent infections that can be fatal. The worldwide prevalence of SCID is estimated to be at least 1:100,000 births, while some genetically more homogenous populations may show markedly increased numbers. Mutations in IL2RG are the most common reason for SCIDs, explaining approximately 50% of all cases and close to 100% of X-linked cases. Availability 4 weeks Gene Set Description Genes in the Severe Combined Immunodeficiency Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ADA Severe combined immunodeficiency due to adenosine deaminase AR 49 93 deficiency AK2 Reticular dysgenesis AR 14 17 ATM Breast cancer, Ataxia-Telangiectasia AD/AR 1047 1109 BCL11B Immunodeficiency