A Cluster Randomized Implementation Trial to Measure the Effectiveness of an Intervention Package Aiming to Increase the Utiliza
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Food Security Bulletin 29
Nepal Food Security Bulletin Issue 29, October 2010 The focus of this edition is on the Mid and Far Western Hill and Mountain region Situation summary Figure 1. Percentage of population food insecure* 26% This Food Security Bulletin covers the period July-September and is focused on the Mid and Far Western Hill and Mountain (MFWHM) 24% region (typically the most food insecure region of the country). 22% July – August is an agricultural lean period in Nepal and typically a season of increased food insecurity. In addition, flooding and 20% landslides caused by monsoon regularly block transportation routes and result in localised crop losses. 18 % During the 2010 monsoon 1,600 families were reportedly 16 % displaced due to flooding, the Karnali Highway and other trade 14 % routes were blocked by landslides and significant crop losses were Oct -Dec Jan-M ar Apr-Jun Jul-Sep Oct -Dec Jan-M ar Apr-Jun Jul-Sep reported in Kanchanpur, Dadeldhura, western Surkhet and south- 08 09 09 09 09 10 10 10 eastern Udayapur. NeKSAP District Food Security Networks in MFWHM districts Rural Nepal Mid-Far-Western Hills&Mountains identified 163 VDCs in 12 districts that are highly food insecure. Forty-four percent of the population in Humla and Bajura are reportedly facing a high level of food insecurity. Other districts with households that are facing a high level of food insecurity are Mugu, Kalikot, Rukum, Surkhet, Achham, Doti, Bajhang, Baitadi, Dadeldhura and Darchula. These households have both very limited food stocks and limited financial resources to purchase food. Most households are coping by reducing consumption, borrowing money or food and selling assets. -

Food Security Bulletin - 21
Food Security Bulletin - 21 United Nations World Food Programme FS Bulletin, November 2008 Food Security Monitoring and Analysis System Issue 21 Highlights Over the period July to September 2008, the number of people highly and severely food insecure increased by about 50% compared to the previous quarter due to severe flooding in the East and Western Terai districts, roads obstruction because of incessant rainfall and landslides, rise in food prices and decreased production of maize and other local crops. The food security situation in the flood affected districts of Eastern and Western Terai remains precarious, requiring close monitoring, while in the majority of other districts the food security situation is likely to improve in November-December due to harvesting of the paddy crop. Decreased maize and paddy production in some districts may indicate a deteriorating food insecurity situation from January onwards. this period. However, there is an could be achieved through the provision Overview expectation of deteriorating food security of return packages consisting of food Mid and Far-Western Nepal from January onwards as in most of the and other essentials as well as A considerable improvement in food Hill and Mountain districts excessive agriculture support to restore people’s security was observed in some Hill rainfall, floods, landslides, strong wind, livelihoods. districts such as Jajarkot, Bajura, and pest diseases have badly affected In the Western Terai, a recent rapid Dailekh, Rukum, Baitadi, and Darchula. maize production and consequently assessment conducted by WFP in These districts were severely or highly reduced food stocks much below what is November, revealed that the food food insecure during April - July 2008 normally expected during this time of the security situation is still critical in because of heavy loss in winter crops, year. -

Feasibility Study of Kailash Sacred Landscape
Kailash Sacred Landscape Conservation Initiative Feasability Assessment Report - Nepal Central Department of Botany Tribhuvan University, Kirtipur, Nepal June 2010 Contributors, Advisors, Consultants Core group contributors • Chaudhary, Ram P., Professor, Central Department of Botany, Tribhuvan University; National Coordinator, KSLCI-Nepal • Shrestha, Krishna K., Head, Central Department of Botany • Jha, Pramod K., Professor, Central Department of Botany • Bhatta, Kuber P., Consultant, Kailash Sacred Landscape Project, Nepal Contributors • Acharya, M., Department of Forest, Ministry of Forests and Soil Conservation (MFSC) • Bajracharya, B., International Centre for Integrated Mountain Development (ICIMOD) • Basnet, G., Independent Consultant, Environmental Anthropologist • Basnet, T., Tribhuvan University • Belbase, N., Legal expert • Bhatta, S., Department of National Park and Wildlife Conservation • Bhusal, Y. R. Secretary, Ministry of Forest and Soil Conservation • Das, A. N., Ministry of Forest and Soil Conservation • Ghimire, S. K., Tribhuvan University • Joshi, S. P., Ministry of Forest and Soil Conservation • Khanal, S., Independent Contributor • Maharjan, R., Department of Forest • Paudel, K. C., Department of Plant Resources • Rajbhandari, K.R., Expert, Plant Biodiversity • Rimal, S., Ministry of Forest and Soil Conservation • Sah, R.N., Department of Forest • Sharma, K., Department of Hydrology • Shrestha, S. M., Department of Forest • Siwakoti, M., Tribhuvan University • Upadhyaya, M.P., National Agricultural Research Council -

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -
End Line Study of Sanitation, Hygiene and Water Management Project, Bajhang Final Report
End Line Study of Sanitation, Hygiene and Water Management Project, Bajhang Final Report Submitted to Nepal Red Cross Society Kathmandu By Chitra Bahadur Budhathoki, PhD Consultant June 2018 The Sanitation, Hygiene and Water Project is supported by the Australian Government through the Australian Red Cross and implemented by Nepal Red Cross Society. ii ACRONYMS ARC : Australian Red Cross BCC : Behaviour Change Communication CHAST : Child Hygiene and Sanitation Training CLTS : Community Led Total Sanitation DRR : Disaster Risk Reduction DWSS : Department of Water Supply and Sewerage D-WASH-CC : District WASH Coordination Committee FCHV : Female Community Health Volunteer FGD : Focus Group Discussion GoN : Government of Nepal IEC : Information, Education and Communication KPI : Key Performance Indicator MTR : Mid-Term Review NRCS : Nepal Red Cross Society PHAST : Participatory Hygiene and Sanitation Transformation ODF : Open Defecation Free RM : Rural Municipality R/M-WASH-CC : Rural/Municipality-Water Supply, Sanitation and Hygiene-Coordination Committee SHWM : Sanitation, Hygiene and Water Management VCA : Vulnerability and Capacity Assessment (VCA) VDC : Village Development Committee VMW : Village Maintenance Worker V-WASH-CC : Village WASH Coordination Committee WASH : Water Sanitation and Hygiene WHO : World Health Organization W-WASH-CC : Ward WASH Coordination Committee WSUC : Water and Sanitation User Committee WUC : Water Users Committee iii ACKNOWLEDGEMENTS This study is an outcome of the collective efforts of the study team and many individuals and institutions. First, I wish to express my sincere gratitude to Nepal Red Cross Society/Australian Red Cross for entrusting me to carry out this study. I would like to thank Mukesh Singh, Amar Mani Poudel, Suvechhya Manandhar and Ganga Shreesh for their continual supports in the entire process of this study. -
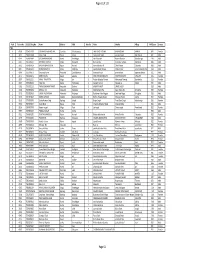
TSLC PMT Result
Page 62 of 132 Rank Token No SLC/SEE Reg No Name District Palika WardNo Father Mother Village PMTScore Gender TSLC 1 42060 7574O15075 SOBHA BOHARA BOHARA Darchula Rithachaupata 3 HARI SINGH BOHARA BIMA BOHARA AMKUR 890.1 Female 2 39231 7569013048 Sanju Singh Bajura Gotree 9 Gyanendra Singh Jansara Singh Manikanda 902.7 Male 3 40574 7559004049 LOGAJAN BHANDARI Humla ShreeNagar 1 Hari Bhandari Amani Bhandari Bhandari gau 907 Male 4 40374 6560016016 DHANRAJ TAMATA Mugu Dhainakot 8 Bali Tamata Puni kala Tamata Dalitbada 908.2 Male 5 36515 7569004014 BHUVAN BAHADUR BK Bajura Martadi 3 Karna bahadur bk Dhauli lawar Chaurata 908.5 Male 6 43877 6960005019 NANDA SINGH B K Mugu Kotdanda 9 Jaya bahadur tiruwa Muga tiruwa Luee kotdanda mugu 910.4 Male 7 40945 7535076072 Saroj raut kurmi Rautahat GarudaBairiya 7 biswanath raut pramila devi pipariya dostiya 911.3 Male 8 42712 7569023079 NISHA BUDHa Bajura Sappata 6 GAN BAHADUR BUDHA AABHARI BUDHA CHUDARI 911.4 Female 9 35970 7260012119 RAMU TAMATATA Mugu Seri 5 Padam Bahadur Tamata Manamata Tamata Bamkanda 912.6 Female 10 36673 7375025003 Akbar Od Baitadi Pancheswor 3 Ganesh ram od Kalawati od Kalauti 915.4 Male 11 40529 7335011133 PRAMOD KUMAR PANDIT Rautahat Dharhari 5 MISHRI PANDIT URMILA DEVI 915.8 Male 12 42683 7525055002 BIMALA RAI Nuwakot Madanpur 4 Man Bahadur Rai Gauri Maya Rai Ghodghad 915.9 Female 13 42758 7525055016 SABIN AALE MAGAR Nuwakot Madanpur 4 Raj Kumar Aale Magqar Devi Aale Magar Ghodghad 915.9 Male 14 42459 7217094014 SOBHA DHAKAL Dolakha GhangSukathokar 2 Bishnu Prasad Dhakal -

Nepal NTFP Alliance
Nepal NTFP Alliance Final Report December 2005 Cooperative Agreement Award No.: 367-A-00-02-00209-00 Project Title: Certification and Sustainable Marketing of Non-timber Forest Products (NTFP) – Private Public Alliance (PPA) Submitted to: USAID/Nepal Ravi Bhawan, Kathmandu Nepal Submitted by: Asia Network for Sustainable Agriculture and Bioresources (ANSAB) P.O. Box 11035 Baneshwor, Kathmandu, Nepal Contact: Dr. Bhishma P. Subedi, Executive Director Project Period: September 27, 2002 – September 30, 2005 Reporting Period: September 27, 2002 – September 30, 2005 ANSAB Final Report 2005 TABLE OF CONTENTS I. INTRODUCTION.......................................................................................................1 II. SUMMARY OF KEY ACHIEVEMENTS ..................................................................2 III. KEY ACHIEVEMENTS ...........................................................................................4 A) NTFP Alliance among national and international companies, networks of forest users and policy makers, NGOs, government programs, and donors developed..........................................................................4 B) Forest certification model developed and forest user groups received international recognition for sustainable forest management and organic production with FSC forest management and organic certifications..............................................................................................................................................................5 C) Capacity of forest -
Paani Program | पानी परियोजना Gender Equality and Social Inclusion Analysis
PAANI PROGRAM | पानी परियोजना GENDER EQUALITY AND SOCIAL INCLUSION ANALYSIS This publication was produced for review by the United States Agency for International Development. It was prepared by DAI Global LLC. The authors’ views expressed in this publication do not necessarily reflect the views of the United States Agency for International Development or the United States Government. Cover photo: Focus group discussion held in November 2018 as part of GESI assessment. Group included Dalit and marginalized community members impacted by environmental damage from unplanned road construction in Thalara Rural Municipality, Bajhang District of West Seti Watershed. Photo credit: USAID Paani Program/ Govinda Bhandari This publication was produced for review by the United States Agency for International Development. It was prepared by DAI Global LLC. The authors’ views expressed in this publication do not necessarily reflect the views of the United States Agency for International Development or the United States Government. PAANI PROGRAM | पानी परियोजना GENDER EQUITY AND SOCIAL INCLUSION ANALYSIS PROGRAM TITLE: USAID PAANI PROGRAM DAI PROJECT NUMBER: 1002810 SPONSORING USAID OFFICE: USAID/NEPAL IDIQ NUMBER: AID-OAA-I-14-00014 TASK ORDER NUMBER: AID-367-TO-16-00001 CONTRACTOR: DAI GLOBAL LLC DATE OF PUBLICATION: APRIL 30, 2019 AUTHOR: BARUN GURUNG CONTENTS BACKGROUND 4 PURPOSE 4 ACTIVITY & TASK SUMMARY 5 METHODOLOGY 5 1. NUMBER OF PEOPLE INTERVIEWED 5 2. METHODS AND TOOLS 6 CONCEPTUAL FRAMEWORK OF THE STUDY 6 1. INNOVATION SYSTEMS APPROACH 6 2. PROGRAM INNOVATION STAGES 7 SOCIAL EXCLUSION / INCLUSION 7 1. THE THREE DIMENSIONS OF AN ORGANIZATION 8 2. ORGANIZATIONAL FRAMEWORK (SEE ANNEX 2 FOR QUESTIONS) 9 3. -

Notice Fifth Lot for All PMT Upto 2075.10.13 Selected & Alternate 2Nd Quintile
मत / / गतेको "गोरखाप दैनक "मा काशत सुचना अनुसार ावधक श ालयहमा डलोमा तहमा भनाx भएर वगत (चार पटक ) मा परयोजनाले सुचना काशन गदाx तो"कएको #यादभ$ आवेदन दताx गराउन छु टेका व(याथ*हले छा$वि-तृ आवेदन (Scholarship Application) फाराम परयोजनाको वेवसाइट www.event.gov.np बाट डाउनलोड गर2 भरेर श ालयले मा3णत गर2 प"रयोजना स%चवालय , वु'नगरमा मत /( /() काया* य समयभ दताx गराउनुहोला । सो5ह सुचना अनुसार डलोमा तहमा बाँक8 रहेका 99 कोटामा छा$वि-तमाृ छनोट गन: योजनका लाग पुवx काशन भएको पएमट2 यो;यता<म अनुसारको =>?@ जनाको नामावल2 । नोट : आवेदन फाराम प"रयोजनाका पुवx सुचनाह1 अनुसार दताx ग"रसकेका 2व3याथ5ह1ले भनु x नपन6 । Selected candidates for Diploma Ward Token VDC/Municipa PMT SN. SLC Reg No Name District Numb Father Mother Village No lity Score er 1 34871 7416018187 SRIJANA KUMARI MAHATO Siraha RamnagarMirchaiya 7 BINDESHWAR MAHATO SUDI RAM DULARI DEVI BAN KARYALAYA CHOWK884.5 2 28644 7259004015 DANSINGH ROKAYA Humla ShreeNagar 5 Barkhe Rokaya Gorikala Parki Rokaya Village 899 3 28719 7059004006 BANDANA PHADERA Humla ShreeNagar 4 Netra Phadera Pushi Phadera Phadera Gaun 905 4 32936 7224003027 JEEWAN KUMAR NEUPANE Rasuwa Dhaibung 4 Khem Raj Neupane Chet Kumari Neupane Katunje 907.5 5 32696 7063022017 KAMAL ROKAYA Jumla Lihi(Rara) 6 MAN BAHADUR ROKAYA MANMA ROKAYA LIHI 910 6 32817 7124013003 Ghyu Jyalmo Tamang Rasuwa Gatlang 8 Kawa Tamang Dawa Chamo Tamang Gre 910.5 7 29380 6562005014 Dipak Kumar Shahi Kalikot Jubika 6 Harsa Bahadur Shahi Padma Shahi Jubitha 911.7 8 30311 7372001067 DEEPA PARIYAR Doti Dipayal Silgadhi N.P.5 DILIP PARIYAR NIRMALA PARIYAR SILGADI 915.5 -

Government of Nepal
Government of Nepal District Transport Master Plan (DTMP) VOLUME – I MAIN REPORT Ministry of Federal Affairs and Local Development Department of Local Infrastructure Development and Agricultural Roads (DOLIDAR) District Development Committee, Bajhang January 2013 Submitted by (SIDeF) for the District Development Committee (DDC) and District Technical Office(DTO),Bajhang with Technical Assistance from the Department of Local Infrastructure and Agricultural Roads (DOLIDAR)Ministry of Federal Affairs and Local Development and grant supported by DFID.Ministry of Federal Affairs and Local Development and grant supported by DFID. Ministry of Federal Affairs and Local Development and grant supported by DFID i PREFACE / ACKNOWLEDGEMENTS This report on the of Preparation of District Transport Master Plan (DTMP) of Bajhang District has been prepared under the contract agreement between RTI SECTOR Maintenance Pilot for Office of District Development Committee, Bajhang District and SIDeF, Kathmandu. The consultant has prepared this report after extensive documentary consultation/ field work, road inventory study and interaction with stakeholders of the district. We would like to extend our heartfelt gratitude to the RTI SECTOR Maintenance Pilot for entrusting us to carry out this task and extend our thanks to all the team of RTI sector Maintenance for the cooperation and guidance in accomplishing the work. SIDeF would like to express our gratitude to Mr. Yuwaraj Kattel, Local Development Officer, Mr. Narendra K.C., Chief DTO, Mr.Lal Bahadur Thapa, Engineer, and all the DDC and DTO staffs for their valuable suggestions and co- operation for the preparation of this report. We also extend our sincere thanks to the representatives of political parties for their active and valuable participation in the process of DTMP preparation. -

GAFSP Nepal CSO Mission Report 2014-06 Final
Nepal Agriculture Food Security Project (AFSP) 6TH CSO MISSION May 9-14, 2014 REPORT Executive Summary The Mission was conducted by Mr. Raul Socrates Banzuela, the Alternate Asia CSO Representative to the GAFSP Steering Committee last May 9-14, 2014, hosted by All Nepal Peasant Federation Association (ANPFA). The key objective of the mission was to get updates on the Nepal Agriculture and Food Security Project and the roles played by CSOs in project implementation. The mission included review of literature; field visit to Bahjhang District and meetings with staff of District Agricultural and Livestock Offices, sub-center, and farmer technician and farmer leaders; meetings with leaders of CSOs which included ANPFA (All Nepal Peasant Federation Association), CSRC (Community Self Reliance Center) and NLRF (National Land Rights Forum-Nepal) ; the Project Head, FAO Team Leader, and the WB's Sr. Rural Development Specialist (co-TTL). The Mission found the Project at its start up phase with both managers and implementers feeling upbeat and excited that after three years, the project had eventually taken off and started the learning stage. The key expected outcomes from the Project are: (i) increase in the productivity of targeted crops; (ii) increase in the yield of targeted livestock products (milk, meat and eggs); (iii) increase in proportion of pregnant and nursing mothers and children between 6-24 months’ age adopting appropriate feeding practices The highest project policy-making body, the Project Steering Committee, has been formed and had met seven months ago, involving a representative each of the National Peasant Coalition and the NGO Federation of Nepal. -

People's Perceptions of Sanitation: Report Findings from Nepal
Report People’s perception on sanitation: Findings from Nepal This document provides people’s insights on why some sanitation interventions successes and others fail. The study showed that awareness among the people about the importance of sanitation and hygiene for better health was higher than expected. Therefore, ignorance of community members cannot be an excuse for not investing in sanitation. The results of the national research, which has been conducted as part of a regional study to gauge people’s perception about water, sanitation and hygiene, emphasis that active engagement of community members coupled with responsive leadership and a strong management ––including aspects of monitoring and evaluation –– is essential for the sustainability of any sanitation intervention. Access to sanitation is directly related with self-esteem. The production of this document was led by Mr Rabin Lal Shrestha from WaterAid in Nepal with support of Advocacy Team Members comprising of Ms Shikha Shrestha, Ms Anita Pradhan and Mr Govind Bahadur Shrestha. Colleagues from WaterAid’s partners in Nepal Federation of Drinking Water and Sanitation Users Nepal, Lumanti Support Group for Shelter and Nepal Water for Health contributed in the collection of cases. Mr Bipin Acharya supported in compiling the national report which was later edited by Mr Abhaya Joshi. This document should be cited as WaterAid in Nepal (2011) Report - People’s perception on sanitation: Findings from Nepal. The document can be found in the documents section of the WaterAid in Nepal country programme website – www.nepal.wateraid.org A WaterAid in Nepal publication September 2011 WaterAid transforms lives by improving access to safe water, hygiene and sanitation in the world’s poorest communities.