Anatomical Pathology Competencies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Medical Directors Arup Medical Directors and Consulting Faculty | 2015
MEDICAL DIRECTORS ARUP MEDICAL DIRECTORS AND CONSULTING FACULTY | 2015 MAY 2015 www.aruplab.com Information in this brochure is current as of May 2015. All content is subject to change. Please contact ARUP Client Services at (800) 522-2787 with any questions or concerns. ARUP LABORATORIES ARUP Laboratories is a national clinical and anatomic pathology reference laboratory and a nonprofit enterprise of the University of Utah and its Department of Pathology. Located in Salt Lake City, Utah, ARUP offers in excess of 3,000 tests and test combinations, ranging from routine screening tests to esoteric molecular and genetic assays. Rather than competing with its clients for physician office business, ARUP chooses instead to support clients’ existing test menus by offering complex and unique tests, with accompanying consultative support, to enhance their abilities to provide local and regional laboratory services. ARUP’s clients include many of the nation’s university teaching hospitals and children’s hospitals, as well as multihospital groups, major commercial laboratories, group purchasing organizations, military and other government facilities, and major clinics. In addition, ARUP is a worldwide leader in innovative laboratory research and development, led by the efforts of the ARUP Institute for Clinical and Experimental Pathology®. Since its formation in 1984 by the Department of Pathology at the University of Utah, ARUP has founded its reputation on reliable and consistent laboratory testing and service. This simple strategy contributes significantly to client satisfaction. When ARUP conducts surveys, clients regularly rate ARUP highly and respond that they would recommend ARUP to others. As the most responsive source of quality information and knowledge, ARUP strives to be the reference laboratory of choice for community healthcare systems. -

Understanding Your Pathology Report: Benign Breast Conditions
cancer.org | 1.800.227.2345 Understanding Your Pathology Report: Benign Breast Conditions When your breast was biopsied, the samples taken were studied under the microscope by a specialized doctor with many years of training called a pathologist. The pathologist sends your doctor a report that gives a diagnosis for each sample taken. Information in this report will be used to help manage your care. The questions and answers that follow are meant to help you understand medical language you might find in the pathology report from a breast biopsy1, such as a needle biopsy or an excision biopsy. In a needle biopsy, a hollow needle is used to remove a sample of an abnormal area. An excision biopsy removes the entire abnormal area, often with some of the surrounding normal tissue. An excision biopsy is much like a type of breast-conserving surgery2 called a lumpectomy. What does it mean if my report uses any of the following terms: adenosis, sclerosing adenosis, apocrine metaplasia, cysts, columnar cell change, columnar cell hyperplasia, collagenous spherulosis, duct ectasia, columnar alteration with prominent apical snouts and secretions (CAPSS), papillomatosis, or fibrocystic changes? All of these are terms that describe benign (non-cancerous) changes that the pathologist might see under the microscope. They do not need to be treated. They are of no concern when found along with cancer. More information about many of these can be found in Non-Cancerous Breast Conditions3. What does it mean if my report says fat necrosis? Fat necrosis is a benign condition that is not linked to cancer risk. -

Simple Technique to Identify Haemosiderin in Immunoperoxidase Stained Sections
J Clin Pathol: first published as 10.1136/jcp.37.10.1190 on 1 October 1984. Downloaded from 1190 Technical methods Phosphate buffer at pH 8*0 gave the sharpest 2 Rozenszajn L, Leibovich M, Shoham D, Epstein J. The esterase staining reactions, although there was little differ- activity in megaloblasts, leukaemic and normal haemopoietic cells. Br J Haematol 1968; 14:605-19. ence at pH 7-0 or pH 7-5. As the buffer pH was 3Hayhoe FGJ, Quaglino D. Haematological cytochemistry. Edin- increased above pH 8-0 staining with both substrates burgh: Churchill Livingstone, 1980. became progressively weaker, especially above pH 4Li CY, Lam KW, Yam LT. Esterases in human leucocytes. J 9.0. Below pH 7-0 staining with a-naphthyl butyrate Histochem Cytochem 1973;21:1-12. Yam LT, Li CY, Crosby WH. Cytochemical identification of became weaker, and below pH 5*0 staining with monocytes and granulocytes. Am J Clin Pathol 1971;55:283- naphthol AS-D chloroacetate began to disappear. 90. 6 Armitage RJ, Linch DC, Worman CP, Cawley JC. The morphol- This work was supported by a Medical Research ogy and cytochemistry of human T-cell subpopulations defined by monoclonal antibodies and Fc receptors. Br J Haematol Council project grant. I thank Professor FGJ 1983;51:605-13. Hayhoe for valuable advice. References Requests for reprints to: Dr DM Swirsky, Department of Gomori G. Chloroacyl esters as histochemical substrates. J His- Haematological Medicine, University Clinical School, Hills tochem Cytochem 1953;1:469-70. Road, Cambridge CB2 2QL, England. Simple technique to identify identification of the two compounds on the same haemosiderin in slide. -

Chlamydia Trachomatis Infection Is Driven by Nonprotective Immune Cells That Are Distinct from Protective Populations
Pathology after Chlamydia trachomatis infection is driven by nonprotective immune cells that are distinct from protective populations Rebeccah S. Lijeka,b,1, Jennifer D. Helblea, Andrew J. Olivea,c, Kyra W. Seigerb, and Michael N. Starnbacha,1 aDepartment of Microbiology and Immunobiology, Harvard Medical School, Boston, MA 02115; bDepartment of Biological Sciences, Mount Holyoke College, South Hadley, MA 01075; and cDepartment of Microbiology and Physiological Systems, University of Massachusetts Medical School, Worcester, MA 01605 Edited by Rafi Ahmed, Emory University, Atlanta, GA, and approved December 27, 2017 (received for review June 23, 2017) Infection with Chlamydia trachomatis drives severe mucosal immu- sequence identity, Chlamydia muridarum, the extent to which the nopathology; however, the immune responses that are required for molecular pathogenesis of C. muridarum represents that of Ct is mediating pathology vs. protection are not well understood. Here, unknown (6). Ct serovar L2 (Ct L2) is capable of infecting the we employed a mouse model to identify immune responses re- mouse upper genital tract when inoculated across the cervix into quired for C. trachomatis-induced upper genital tract pathology the uterus (7, 8) but it does not induce robust immunopathology. and to determine whether these responses are also required for This is consistent with the human disease phenotype caused by Ct L2, bacterial clearance. In mice as in humans, immunopathology was which disseminates to the lymph nodes causing lymphogranuloma characterized by extravasation of leukocytes into the upper genital venereum (LGV) and is not a major cause of mucosal immunopa- thology in the female upper genital tract (uterus and ovaries). tract that occluded luminal spaces in the uterus and ovaries. -

Department of Experimental Pathology, Immunology and Microbiology 531
Department of Experimental Pathology, Immunology and Microbiology 531 Department of Experimental Pathology, Immunology and Microbiology Interim Chairperson: Zaatari, Ghazi Vice Chairperson: Matar, Ghassan Professors: Abdelnoor, Alexander; Khouri, Samia; Matar, Ghassan; Sayegh, Mohamed; Zaatari, Ghazi Associate Professor: Rahal, Elias Assistant Professors: Al-Awar, Ghassan; El Hajj, Hiba; Shirinian, Margret; Zaraket, Hassan The Department of Experimental Pathology, Immunology and Microbiology offers courses to medical laboratory sciences (MLSP) students as well as nursing, medical, and graduate students. It offers a graduate program (discipline of Microbiology and Immunology) leading to a master’s degree (MS) or doctoral degree (PhD) in Biomedical sciences. The requirements for admission to the graduate program are stated on page 33 of this catalogue. IDTH 203 The immune System in Health and Disease 37.28; 3 cr. See Interdepartmental Courses. IDTH 205 Microbiology and Infectious Diseases 37.28; 5 cr. See Interdepartmental Courses. MBIM 223 Parasitology for MLSP Students 39.39; 4 cr. Second semester. MBIM 237 Microbiology and Immunology for Nursing Degree Students 32.64; 3 cr. A course on the fundamental aspects of medical microbiology and immunology for nursing students. Second semester. MBIM 260 Elective in Infectious Diseases for Medicine III and IV 0.180 A course on basic evaluation, diagnosis, and management of infectious diseases. One month. MBIM 261 Elective in Immunology for Medicine III and IV 0.180 A course that is an introduction to immunological research and its application to clinical practice. One month. MBIM 310 Basic Immunology 32.32; 3 cr. A course on innate and adaptive immune mechanisms, infection and immunity, vaccination, immune mechanisms in tissue injury and therapeutic immunology. -

Deciphering the Triad of Infection, Immunity and Pathology
INSIGHT DISEASE Deciphering the triad of infection, immunity and pathology The factors which drive and control disease progression can be inferred from mathematical models that integrate measures of immune responses, data from tissue sampling and markers of infection dynamics. FREDERIK GRAW immune actors in the body. Now, in eLife, Related research article Myers MA, Smith Amber Smith and colleagues at St. Jude Child- AP, Lane LC, Moquin DJ, Aogo R, Woolard ren’s Research Hospital, the University of Ten- S, Thomas P, Vogel P, Smith AM. 2021. nessee Health Science Center and the Dynamically linking influenza virus infection Washington University School of Medicine – kinetics, lung injury, inflammation, and dis- including Margaret Myers and Amanda Smith as ease severity. eLife 10:e68864. doi: 10. joing first authors – report how viral infection, 7554/eLife.68864 counteracting immune responses and lung pathology interact as mice fight off influenza A (Myers et al., 2021). First, the team tracked how viral load and the number of CD8+ T cells, an important immune fever, a cough, a splitting headache... actor that helps to clear infected cells, pro- Being sick often comes with tell-tale gressed over time. In combination with mathe- A signs which worsen as the disease pro- matical models, these measurements allowed gresses and tissues become damaged. These Myers et al. to estimate several parameters that symptoms result from complex interactions reflect the pace at which the virus replicates, the between the infecting pathogen, the inflamma- strength of the immune response, and the inter- tion process, and the response from the immune actions between these processes. -

Anatomical Pathology Residency Program PROGRAM DESCRIPTION and OUTLINE – Non-CBME
Anatomical Pathology Residency Program PROGRAM DESCRIPTION AND OUTLINE – Non-CBME The Anatomical Pathology Residency Program at the Schulich School of Medicine & Dentistry at Western University is a five year program based at the London Health Sciences Centre, University Hospital. There is a structured schedule of rotations designed to ensure that residents are able to fulfill all of the goals and objectives of training and acquire the necessary knowledge base to practice as competent consultant pathologists. There are also elective opportunities that permit the resident to tailor the program to their own needs and goals. There is a comprehensive education program, with various rounds and teaching sessions that supplement the rotations. Program Organization Rotations (4 week blocks) General Surgery 2 blocks General Internal Medicine 1 block Respirology or Nephrology 1 block Gynecologic Oncology 1 block Radiation Oncology 1 block Emergency Medicine 1 block PGY1 Urology 1 block Gastroenterology 1 block Hematology Oncology 1 block Anatomical Pathology 1 block Otolaryngology 1 block Pediatric Medicine 1 block The PGY1 year is a broad based clinical year designed to satisfy the specialty-specific objectives and Medical Council of Canada Qualifying Examination Part II requirements. Rotations are planned in conjunction with the resident in order to meet individual needs (the above-mentioned rotations may be changed). During this year, the resident attends the Pathology Academic Half Day, Department of Pathology Grand Rounds, and the Department -

Overview of Pathology and Its Related Disciplines - Soheir Mahmoud Mahfouz
MEDICAL SCIENCES – Vol.I -Overview of Pathology and its Related Disciplines - Soheir Mahmoud Mahfouz OVERVIEW OF PATHOLOGY AND ITS RELATED DISCIPLINES Soheir Mahmoud Mahfouz Cairo University, Kasr El Ainy Hospital, Egypt Keywords: Pathology, Pathology disciplines, Pathology techniques, Ancillary diagnostic methods, General Pathology, Special Pathology Contents 1. Introduction 1.1 Pathology coverage 1.1.1 Etiology and Pathogenesis of a Disease 1.1.2 Manifestations of Disease (Lesions) 1.1.3 Phases Of A Disease Process (Course) 1.2 Physician’s approach to patient 1.3 Types of pathologists and affiliated specialties 1.4 Role of pathologist 2. Pathology and its related disciplines 2.1 Cytology 2.1.1 Cytology Samples 2.1.2 Technical Aspects 2.1.3 Examination of Sample and Diagnosis 3. Pathology techniques and ancillary diagnostic methods 3.1 Macroscopic pathology 3.2 Light Microscopy 3.3 Polarizing light microscopy 3.4 Electron microscopy (EM) 3.5 Confocal Microscopy 3.6 Frozen section 3.7 Cyto/histochemistry 3.8 Immunocyto/histochemical methods 3.9 Molecular and genetic methods of diagnosis 3.10 Quantitative methods 4. Types of tests used in pathology 4.1 DiagnosticUNESCO tests – EOLSS 4.2 Quantitative tests 4.3 Prognostic tests 5. The scope of SAMPLEpathology & its main divisions CHAPTERS 6. Conclusions Glossary Bibliography Biographical sketch Summary Pathology is the science of disease. It deals with deviations from normal body function and ©Encyclopedia of Life Support Systems (EOLSS) MEDICAL SCIENCES – Vol.I -Overview of Pathology and its Related Disciplines - Soheir Mahmoud Mahfouz structure. Many disciplines are involved in the study of disease, as it is necessary to understand the complex causes and effects of various disorders that affect the organs and body as a whole. -

2019-General-Pathology-Faq.Pdf
FREQUENTLY ASKED QUESTIONS – 2019 Program: GENERAL PATHOLOGY Specialty/Field Questions: 1. a) What are some strengths about your specialty? What draws and keeps people in your specialty? • The opportunity to understand the nature of disease in an in-depth way that isn’t achieved in any other specialty. You get to practice scientific diagnostic medicine over a broad range of subjects and you have a fair degree of control over your schedule. You are very much a part of the team taking care of the patient (it just isn’t as obvious!), and this is becoming even more apparent in the era of precision medicine. • Although there is limited direct contact with patients, there is a great deal of contact with a variety of clinicians outside the laboratory as well as with physician, PhD, and technical staff colleagues within the laboratory. We get satisfaction from the interactions we have with others, and knowing that we are helping a clinician take the next step in diagnosing or treating a patient. The stereotypical image of the hermit- like pathologist who stays in their office and never talks to anyone is rapidly disappearing in today’s pathology practice. b) What are some common complaints about your specialty? • There is limited direct clinical contact – you’ll never have an office full of patients who regard you as their doctor and most pathologists have a hospital-based practice which can limit professional autonomy. • You often have to sit/stand at a microscope and/or computer a lot, so sometimes you need to get creative about staying active during the day. -

Consensus Guideline on Concordance Assessment of Image-Guided Breast Biopsies and Management of Borderline Or High-Risk Lesions
- Official Statement - Consensus Guideline on Concordance Assessment of Image-Guided Breast Biopsies and Management of Borderline or High-Risk Lesions Purpose To outline the management approach for borderline and high risk lesions identified on image-guided breast biopsy. Associated ASBrS Guidelines or Quality Measures 1. Image-Guided Percutaneous Biopsy of Palpable and Nonpalpable Breast Lesions 2. Performance and Practice Guidelines for Stereotactic Breast Procedures 3. Concordance Assessment Following Image-Guided Breast Biopsy Methods Literature review inclusive of recent randomized controlled trials evaluating the management of various borderline and high-risk lesions (including atypical hyperplasia, lobular neoplasia, papillary lesions, radial scars and complex sclerosing lesions, fibroepithelial lesions, mucocele-like lesions, spindle cell lesions, and pseudoangiomatous stromal hyperplasia [PASH]) identified on image-guided breast biopsies. This is not a complete systematic review but a comprehensive review of the modern literature on this subject. The ASBS Research Committee developed a consensus document which the ASBS Board of Directors reviewed and approved. Summary of Data Reviewed Percutaneous core needle biopsy (CNB) is the preferred, initial, minimally invasive diagnostic procedure for nonpalpable breast lesions or palpable breast masses.1 Concordance assessment of the histologic, imaging, and clinical findings determines further management. Discordance refers to the situation in which a breast CNB demonstrates benign histology, while the clinical or imaging findings are suspicious for malignancy. If there is discordance between imaging and pathology, histological evaluation is still needed. This can be accomplished either by repeat CNB, perhaps with consideration of larger gauge or vacuum- assisted device, or surgical excision.2-5 Some nonmalignant CNB findings are considered “borderline” because of their potential association with malignancy. -
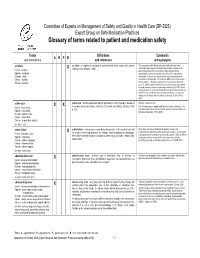
Glossary of Terms Related to Patient and Medication Safety
Committee of Experts on Management of Safety and Quality in Health Care (SP-SQS) Expert Group on Safe Medication Practices Glossary of terms related to patient and medication safety Terms Definitions Comments A R P B and translations and references and synonyms accident accident : an unplanned, unexpected, and undesired event, usually with adverse “For many years safety officials and public health authorities have Xconsequences (Senders, 1994). discouraged use of the word "accident" when it refers to injuries or the French : accident events that produce them. An accident is often understood to be Spanish : accidente unpredictable -a chance occurrence or an "act of God"- and therefore German : Unfall unavoidable. However, most injuries and their precipitating events are Italiano : incidente predictable and preventable. That is why the BMJ has decided to ban the Slovene : nesreča word accident. (…) Purging a common term from our lexicon will not be easy. "Accident" remains entrenched in lay and medical discourse and will no doubt continue to appear in manuscripts submitted to the BMJ. We are asking our editors to be vigilant in detecting and rejecting inappropriate use of the "A" word, and we trust that our readers will keep us on our toes by alerting us to instances when "accidents" slip through.” (Davis & Pless, 2001) active error X X active error : an error associated with the performance of the ‘front-line’ operator of Synonym : sharp-end error French : erreur active a complex system and whose effects are felt almost immediately. (Reason, 1990, This definition has been slightly modified by the Institute of Medicine : “an p.173) error that occurs at the level of the frontline operator and whose effects are Spanish : error activo felt almost immediately.” (Kohn, 2000) German : aktiver Fehler Italiano : errore attivo Slovene : neposredna napaka see also : error active failure active failures : actions or processes during the provision of direct patient care that Since failure is a term not defined in the glossary, its use is not X recommended. -

2021 Anatomic & Clinical Pathology
BEAUMONT LABORATORY 2021 ANATOMIC & CLINICAL PATHOLOGY Physician Biographies Expertise BEAUMONT LABORATORY • 800-551-0488 BEAUMONT LABORATORY ANATOMIC & CLINICAL PATHOLOGY • PHYSICIAN BIOGRAPHIES Peter Millward, M.D. Mitual Amin, M.D. Chief of Clinical Pathology, Beaumont Health Interim Chair, Pathology and Laboratory Medicine, Interim Chief of Pathology Service Line, Beaumont Health Royal Oak Interim Physician Executive, Beaumont Medical Group Interim Chair, Department of Pathology and Laboratory Medicine, Oakland University William Beaumont School Interim System Medical Director, Beaumont Laboratory of Medicine Outreach Services Board certification Associate Medical Director, Blood Bank and • Anatomic and Clinical Pathology, Transfusion Medicine, Beaumont Health American Board of Pathology Board certification Additional fellowship training • Anatomic and Clinical Pathology, • Surgical Pathology American Board of Pathology Special interests Subspecialty board certification • Breast Pathology, Genitourinary Pathology, • Blood Banking and Transfusion Medicine, Gastrointestinal Pathology American Board of Pathology Lubna Alattia, M.D. Kurt D. Bernacki, M.D. Cytopathologist and Surgical Pathologist, Trenton System Medical Director, Surgical Pathology Board certification Beaumont Health • Anatomic and Clinical Pathology, Chief, Pathology Laboratory, West Bloomfield American Board of Pathology Breast Care Center Subspecialty board certification Diagnostic Lead, Pulmonary Tumor Pathology • Cytopathology, American Board of Pathology Diagnostic