Uthealth Population Health Strategic Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical School
Medical School Texas A&M Professional School Advising can advise you realistically on whether you are a competitive applicant for admission to medical school, however only you can decide if medical school is truly what you want to do. One way to explore your interest is to gain exposure by volunteering and shadowing in the different healthcare professions we advise for. You can also observe or shadow a physician and talk to professionals in the different fields of healthcare. Another way is to read information about professional schools and medicine as a career and to join one of the campus pre-health organizations. What type of major looks best? Many applicants believe that medical schools want science majors or that certain programs prefer liberal arts majors. In actuality medical schools have no preference in what major you choose as long as you do well and complete the pre-requisite requirements. Texas A&M does not have a pre-medical academic track which is why we suggest that you choose a major that leads to what you would select as an alternative career. The reason for this line of logic is that you generally do better in a major you are truly passionate and interested in and in return is another great way to determine whether medicine is the right choice. Plus an alternative career provides good insurance if you should happen to change direction or postpone entry. Texas A&M University offers extensive and exciting majors to choose from in eleven diverse colleges. If your chosen major does not include the prerequisite courses in its curriculum, you must complete the required courses mentioned below either as science credit hours or elective credit hours. -

Greater LIFE ALONG the TEXAS GULF COAST
Greater LIFE ALONG THE TEXAS GULF COAST BAYTOWNAugust 2019 Outpatient Rehabilitation done right Weight-loss Surgery Common Questions Telepsychiatry Helping Teens with mental health KEEP YOU MOVING without joint pain Live life without joint pain. At Houston Methodist Orthopedics & Sports Medicine in Baytown, we know that joint pain affects every part of your life. With treatment plans customized for you, our specialists offer a full range of advanced nonsurgical and surgical techniques, including: • Innovative pain control methods • Physical therapy to improve mobility and range of motion Baytown • Latest technology, including minimally invasive surgical techniques • Presurgical education programs for joint replacement We can help you fi nd relief from joint pain — so you can keep moving. Schedule an appointment: houstonmethodist.org/jointpain 281.427.7400 HEALTHCARE KEEP TRAINING YOU Dental Assistant Program MOVING EKG Technician without joint pain Certified Nurse Aide (CNA) Emergency Medical Technician (EMT) Live life without joint pain. At Houston Methodist Orthopedics & Sports Medicine in Baytown, we know that joint pain affects every part of your life. With treatment plans customized for you, our specialists offer a full range of advanced nonsurgical and surgical techniques, including: • Innovative pain control methods • Physical therapy to improve mobility and range of motion Baytown • Latest technology, including minimally invasive surgical techniques • Presurgical education programs for joint replacement We can help you fi nd relief from joint pain — so you can keep moving. Schedule an appointment: houstonmethodist.org/jointpain 281.427.7400 Greater LIFE ALONG THE TEXAS GULF COAST Welcome to the Health edition of Greater Baytown. You will findBAYTOWN many interesting stories inside, including topics such as Houston Methodist Baytown Hospital doctors, Our staff physical therapists and the many services they provide. -

ALLOPATHIC MEDICINE (MD) Austin College Health Professions Advising Guide
ALLOPATHIC MEDICINE (MD) Austin College Health Professions Advising Guide WHAT IS ALLOPATHIC MEDICINE? Allopathy is the current term for modern, science-based medicine. Physicians trained in allopathic medicine receive an MD degree, and can practice in various specialties of medical practice, as well as teaching and research. MEDICAL SCHOOL PROGRAMS: Medical school programs include a four-year professional curriculum which is typically followed by a residency lasting from three to as many as seven or eight years depending on the specialty. The core of basic science courses and clinical clerkships is similar at all accredited medical schools. TEXAS MEDICAL SCHOOLS (Offering MD degree): There are currently ten medical schools in Texas offering the MD degree, nine of which you can apply to with a single application to the Texas Medical & Dental Schools Application Service (TMDSAS) www.tmdsas.com. You must apply to Baylor College of Medicine through the American Medical College Application Service (AMCAS) https://students-residents.aamc.org/applying-medical-school/applying-medical-school-process/applying- medical-school-amcas/ . Texas Medical Schools Website The University of Texas Southwestern Medical http://www.utsouthwestern.edu/education/medical- Center* school/admissions/ The University of Texas Medical Branch at https://som.utmb.edu/Admissions/ Galveston* Texas A&M Health Science Center, College of https://medicine.tamhsc.edu/admissions/ Medicine* McGovern Medical School* https://med.uth.edu/admissions/ The University of Texas School of Medicine at San http://som.uthscsa.edu/admissions/ Antonio* The University of Texas at Austin, Dell Medical http://dellmedschool.utexas.edu/prospective- School* students The University of Texas Rio Grande Valley School http://www.utrgv.edu/school-of- of Medicine* medicine/admissions-and-aid/index.htm Texas Tech University Health Science Center http://www.ttuhsc.edu/som/admissions/ School of Medicine* Texas Tech University Health Sciences Center El http://elpaso.ttuhsc.edu/som/admissions/ Paso, Paul L. -

Jane Elizabeth Hamilton, Phd, MPH, LCSW
Jane Elizabeth Hamilton, PhD, MPH, LCSW Date: February 13, 2017 PRESENT TITLE: Assistant Professor of Psychiatry-Clinical WORK ADDRESS: 1941 East Road, Suite 1204 Houston, TX 77054 UNDERGRADUATE EDUCATION: University of Nebraska-Omaha, BS Environmental Science GRADUATE EDUCATION: University of Texas School of Public Health, Doctor of Philosophy, Health Services Research, Health Policy, and Biostatistics. (2013) University of Texas School of Public Health, Master of Public Health (2007) University of Houston Graduate College of Social Work, Master of Social Work (1999) POSTGRADUATE TRAINING: McGovern Medical School, Department of Psychiatry and Behavioral Sciences. Postdoctoral Fellowship in Outcomes Research ACADEMIC & ADMINISTRATIVE APPOINTMENTS: McGovern Medical School, Department of Psychiatry and Behavioral Sciences. HOSPITAL APPOINTMENTS: UTHealth Harris County Psychiatric Center LICENSURE: Licensed Clinical Social Worker-Texas Board Approved Supervisor HONORS AND AWARDS: Golden Key National Honor Society JOURNAL PEER REVIEWER Journal of Affective Disorders Psychiatry Research Journal of Psychiatric Research BMC Family Practice UNIVERSITY SERVICE: McGovern Medical School Curriculum Committee. Appointed September 1, 2016 to August 31, 2017. 1 SERVICE TO THE COMMUNITY: TMF Quality Innovation Network CMS Quality Improvement Organization (QIN-QIO). Oral presentation with Stephen Glazier, M.B.A., FACHE, Chief Operating Officer, UTHealth HCPC on behavioral health issues and coordination of care in the Houston area at the Houston Recovery Place on February 23, 2017. TMF Quality Innovation Network CMS Quality Improvement Organization (QIN-QIO). Community Stakeholder: Presented webinar: “Translating Research into Practice: Implementing a Hospital-Based Readmissions Reduction Performance Improvement Project.” Webinar presentation: June 16, 2016. Primary Care Innovation Center (PCIC) Baylor College of Medicine: Stakeholder. Participate in clinic staffing and patient home visits. -
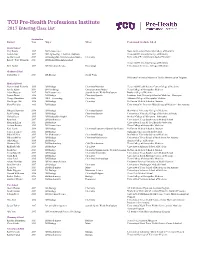
TCU Pre‐Health Professions Institute 2017 Entering Class List
TCU Pre‐Health Professions Institute 2017 Entering Class List Graduation Student Year Major Minor Professional/Graduate School Dental School Cary Brown 2017 BS Neuroscience Nova Southeastern University College of Dentistry Lauren Getz 2017 BS Engineering - Electrical Emphasis Texas A&M University College of Dentistry Joe Raftevold 2017 BS Biology/BS Communication Studies Chemistry University of Pennsylvania School of Dentistry Robert "Will" Rudnicki 2017 BS Biology/BA Anthropology Texas A&M University College of Dentistry Kim Taylor 2017 BS Movement Science Psychology University of Tennessee College of Dentistry Graduate School Taylor Hayes 2017 BA Biology Social Work Oklahoma University Masters of Health Administration Program Medical School Marien Abud-Pichardo 2015 BS Biology Chemistry/Nutrition Texas A&M Health Science Center College of Medicine Ariella Azimi 2014 BS Psychology Communication Studies Texas College of Osteopathic Medicine Adam Burgess 2017 BS Neuroscience Spanish for the Health Professions Baylor College of Medicine Lauren Dawn 2016 BS Biology Chemistry/Spanish Louisiana State University School of Medicine - Shreveport George Downham 2016 BBA - Accounting Chemistry Alabama College of Osteopathic Medicine MacGregor Hall 2016 BS Biology Chemistry McGovern Medical School at Houston Mary Hamblen 2016 BS Biology University of the Incarnate Word School of Medicine - San Antonio Mikayla Hamilton 2016 BS Biology Chemistry/Spanish Des Moines University College of Medicine Paul Harding 2015 BS Biology Chemistry/Spanish University -

COPHS Faculty Curriculum Vitae
Faculty CVs CURRICULUM VITAE NAME: Cyril V. Abobo DEGREE: Doctor of Pharmacy Florida A & M University College of Pharmacy & Pharmaceutical Sciences Tallahassee, Florida Bachelor of Science/Pharmacy Texas Southern University College of Pharmacy & Health Sciences Houston, Texas ADDITIONAL American Association of Colleges of Pharmacy TRAINING: Fellowship (2004-2005) University of Georgia, College of Pharmacy, Department of Pharmaceutics. Assay development, animal dosing techniques, and pre-clinical studies of anti-retroviral agents. (January - May, 1992) Licensure Texas State Board of Pharmacy Certifications Physical Assessment in Patient Care Management Nova Southeastern University, July 2002. Delivering Medication Therapy Management Services in the Community. American Pharmacists Association, May 2010. Pharmacy Based Immunization Delivery: Certificate Program for Pharmacists. American Pharmacists Association, October, 2011. PROFESSIONAL EXPERIENCE: 1993-Present Associate Professor, Pharmacy Practice Texas Southern University College of Pharmacy and Health Sciences 1993-2008 Part Time/Registry Pharmacist (Inpatient) - Weekends Ben Taub General Hospital Houston, Texas 77030 1988-1993 Assistant Professor, Pharmacy Practice Texas Southern University College of Pharmacy and Health Sciences 1988-Present Clinical Pharmacy Preceptor Texas Southern University College of Pharmacy and Health Sciences Internal/General Medicine Michael E. DeBakey Veterans Affairs Medical Center Houston Texas 1987-88 Clinical staff pharmacist/Clinical Preceptor Ben Taub General Hospital Houston, Texas 77030 1985-86 Lecturer University of Benin School of Pharmacy Benin City, Nigeria 1983-85 Clinical staff pharmacist/Clinical Preceptor Ben Taub General Hospital Houston, Texas 77030 RESEARCH/SCHOLARSHIP Publications Abobo CV, Ma J, Liang D. Effect of menthol on nicotine pharmacokinetics in rats after cigarette smoke inhalation. Nicotine Tob Res. 2012: doi: 10.1093/ntr/ntr287. -

Smu Medical School Admissions Statistics (2020 Entering Class)
SMU MEDICAL SCHOOL ADMISSIONS STATISTICS (2020 ENTERING CLASS) SMU Applicants (Total) 77 SMU Accepted Applicants 44 SMU Acceptance Rate 57% National Acceptance Rate 44% ACCEPTED MEDICAL SCHOOLS ALABAMA COLLEGE OF OSTEOPATHIC MEDICINE SMU HPRC Applicants 32 ALBANY MEDICAL COLLEGE SMU HPRC Acceptance Rate 69% ARIZONA COLLEGE OF OSTEOPATHIC MEDICINE/MIDWESTERN UNIV. ARKANSAS COLLEGE OF OSTEOPATHIC MEDICINE National Average Accepted GPA 3.73 A.T. STILL UNIV. SCHOOL OF OSTEOPATHIC MEDICINE/ARIZONA SMU Average Accepted GPA 3.75 BAYLOR COLLEGE OF MEDICINE SMU Average Applicant GPA 3.69 CALIFORNIA HEALTH SCIENCES COLLEGE OF OSTEOPATHIC MEDICINE CALIFORNIA UNIV. OF SCIENCE AND MEDICINE DONALD AND BARBARA ZUCKER SCHOOL OF MEDICINE AT HOFSTRA National Average Accepted Science GPA 3.66 SMU Average Accepted Science GPA 3.70 EAST TENNESSEE STATE UNIV. JAMES H. QUINLAN COM SMU Average Applicant Science GPA 3.61 KANSAS CITY UNIVERSITY COLLEGE OF OSTEOPATHIC MEDICINE LAKE ERIE COLLEGE OF OSTEOPATHIC MEDICINE LIBERTY UNIVERITY COLLEGE OF OSTEOPATHIC MEDICINE National Average Accepted MCAT 511.6 LONG SCHOOL OF MEDICINE AT UT HSC SAN ANTONIO SMU Average Accepted MCAT 511.4 LOUISIANA STATE UNIV. SOM/NEW ORLEANS SMU Average Applicant MCAT 509.4 LOUISIANA STATE UNIV. SOM/SHREVEPORT MCGOVERN MEDICAL SCHOOL AT UT HSC HOUSTON Majors of Accepted Applicants MEHARRY MEDICAL COLLEGE MOREHOUSE SCHOOL OF MEDICINE Biochemistry Journalism Biological Sciences Mechanical Engineering NYIT OF TECH. COLLEGE OF OSTEPATHIC MED/ARKANSAS Business Music NORTHWESTERN UNIV. THE FIENBERG SCHOOL OF MEDICINE Chemistry Political Science NEW YORK MEDICAL COLLEGE Dance Performance Psychology NOVA SOUTHEASTERN COLLEGE OF OSTEOPATHIC MEDICINE Economics Public Policy RUTGERS, ROBERT WOOD JOHNSON MEDICAL SCHOOL Electrical Engineering Pure Mathematics SAINT LOUIS UNIV. -

Fifty Highlights
1 FIFTY YEARS — FIFTY HIGHLIGHTS YEAR IN REVIEW MCGOVERN MEDICAL SCHOOL YEAR IN REVIEW CREDITS Year in Review is published by McGovern Medical School All correspondence should be addressed to: Office of Communications 6431 Fannin Street, B.340 Houston, TX 77030 E-mail: [email protected] Articles and photos may be reprinted with permission. EDITOR Darla Brown Director Office of Communications WRITERS Darla Brown TABLE OF CONTENTS Roman Petrowski Mika Stepankiw Amy Laukka 1 Harris Health Message from the Dean 2 DESIGN News of Note Omar Aguado Roy Prichard 6 Fifty Years, 50 Highlights PHOTOGRAPHY 32 Dwight Andrews Accolades Archival Randy Gay 34 Philanthropy 40 Distinguished Alumni 42 Department Profiles 54 In Memoriam McGOVERN MEDICAL SCHOOL 3 MESSAGE FROM THE DEAN McGovern Medical School has a rich history. We are a patchwork of incredible people whose contributions have made the school what it is today. This year we had the honor of looking back and celebrating the school’s 50-year history – our people, programs, and traditions. We celebrated this 50th year with a number of special events and nationally recognized speakers. In addition, we invited all members of our medical school family – past and present – to share their medical school stories and personal reflections with us, in a unique video project we are calling Time Capsules. I invite you to view these special video remembrances on the McGovern Medical School YouTube site (https://www.youtube.com/user/utmedicalschool/ videos). Please contact our office ([email protected]. edu) if you are interested in sharing your own McGovern history with us. -
John P. and Kathrine G. Mcgovern Medical School History Established by the Texas Legislature in June 1969, the First Class of 19 Students Entered in 1970
John P. and Kathrine G. McGovern Medical School History Established by the Texas Legislature in June 1969, the first class of 19 students entered in 1970. By 1979, class sizes of 200 were legislatively supported through state formula funding. From a new school with no buildings or students, to one of the nation’s outstanding centers of academic medicine, The John P. and Kathrine G. McGovern Medical School at The University of Texas Health Science Center at Houston (UTHealth) continues to develop into one of the leading centers of excellence devoted to medical education, research, quality patient care, and community outreach. Take a moment to review a brief summary of milestones that tell the unfolding story of McGovern Medical School. JANUARY 1968 Original affiliation agreement is signed between the Hermann Hospital Estate and The University of Texas Board of Regents, MAY 1969 making Hermann Hospital the primary The Texas Legislature approves the teaching facility for the proposed University UT Medical School at Houston. of Texas Medical School at Houston. JUNE 1969 Gov. Preston Smith signs House Bill 80 into law at Texas Medical Center ceremonies in the Sammons Auditorium of the Jesse H. Jones Library Building. 19 70 APRIL 1970 Cheves McCord Smythe, MD, is SEPTEMBER 1970 appointed first dean of the new school. The first class of 19 students is selected and enrolls at UT campuses in three cities. JUNE 1971 The first entering class of 32 students to complete all studies in AUGUST 1971 Houston is welcomed at orientation. John H. Freeman Building construction begins. OCTOBER 1972 George Bush, U.S. -

A Year to Remember. a Future to Embrace
A YEAR TO REMEMBER. A FUTURE TO EMBRACE. 2018 REPORT TO THE COMMUNITY 1 Unexpected challenges bring out our best 2 For more than 50 years, Harris Health System has served as the safety net for the people Our vision of Harris County, providing exceptionally Harris Health will become the premier public high-quality healthcare to those most in need. academic healthcare system in the nation. Hurricane Harvey made this last fiscal year even more eventful than most, which is why we are especially proud to present this annual report. Our mission It is our privilege and our passion to be here, Harris Health is a community-focused as always, sharing our community’s triumphs academic healthcare system dedicated to and challenges while working to provide the improving the health of those most in need in best care, the latest technology and the most Harris County through quality care delivery, innovative healthcare services. coordination of care and education. 3 Message to our community No look back at the past year can ignore the devastating storm that dominated our lives and headlines. As Harvey’s drama unfolded, we saw Houstonians come together in amazing ways. But Harvey also confirmed something we’ve known for more than 50 years. As the health system for those most in need in our community, we have a critical responsibility to always be ready to provide the highest level of treatment and service. We are pleased to be making substantial investments and improvements throughout our system. Vital renovations at Ben Taub Hospital are moving forward. We’ve added home-based dialysis and Houston Hospice care programs. -

The Graduate Medical Education (GME) Report: an Assessment of Opportunities for Graduates of Texas Medical Schools to Enter Residency Programs in Texas
Academic Quality and Workforce (Add division The Graduate Medical Education (GME) Report: An Assessment of Opportunities for Graduates of Texas Medical Schools to Enter Residency Programs in Texas A Report to the Texas Legislature per Texas Education Code, Section 61.0661 October 2018 This page has been left blank intentionally. Texas Higher Education Coordinating Board Stuart W. Stedman, CHAIR Houston Fred Farias III, OD, VICE CHAIR McAllen John T. Steen Jr., SECRETARY TO THE BOARD San Antonio Arcilia C. Acosta Dallas S. Javaid Anwar Midland Michael J. Plank Houston Ricky A. Raven Sugarland Donna N. Williams Arlington Welcome Wilson Jr. Houston Michelle Q. Tran, STUDENT REPRESENTATIVE Houston Raymund A. Paredes, COMMISSIONER OF HIGHER EDUCATION Agency Mission The mission of the Texas Higher Education Coordinating Board (THECB) is to provide leadership and coordination for Texas higher education and to promote access, affordability, quality, success, and cost efficiency through 60x30TX, resulting in a globally competitive workforce that positions Texas as an international leader. Agency Vision The THECB will be recognized as an international leader in developing and implementing innovative higher education policy to accomplish our mission. Agency Philosophy The THECB will promote access to and success in quality higher education across the state with the conviction that access and success without quality is mediocrity and that quality without access and success is unacceptable. The THECB’s core values are: Accountability: We hold ourselves responsible for our actions and welcome every opportunity to educate stakeholders about our policies, decisions, and aspirations. Efficiency: We accomplish our work using resources in the most effective manner. -

2020-2021 Mcgovern Medical School
2020-2021 Catalog Cover Page This catalog is a general information publication only. It is not intended to nor does it contain all regulations that relate to students. Applicants, students, and faculty are referred to The University of Texas Health Science Center at Houston General Catalog. The provisions of this catalog and/or the General Catalog do not constitute a contract, express or implied, between any applicant, student or faculty member and McGovern Medical School or The University of Texas System. The McGovern Medical School reserves the right to withdraw courses at any time, to change fees or tuition, calendar, curriculum, degree requirements, graduation procedures, and any other requirements affecting students. Changes will become effective whenever the proper authorities so determine and will apply to both prospective students and those already enrolled. Accreditation The University of Texas Health Science Center at Houston is accredited by the Southern Association of Colleges and Schools Commission on Colleges to award certificate, baccalaureate, masters, doctorate and special professional degrees. Contact the Commission on Colleges at 1866 Southern Lane, Decatur, Georgia 30033-4097 or call 404-679- 4500 for questions about the accreditation of The University of Texas Health Science Center at Houston. The McGovern Medical School is accredited by the Liaison Committee on Medical Education located at: 655 K Street, NW, Suite 100, Washington, DC 20001. Telephone: 202.828.0596. To the extent provided by applicable law, no person shall be excluded from participation in, denied the benefits of, or be subject to discrimination under any program or activity sponsored or conducted by UTHealth on the basis of race, color, national origin, religion, sex, sexual orientation, gender expression or gender identity, age, veteran status, genetic information, disability or any other basis prohibited by law.