SFY2002 OHCA Annual Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fresh Thoughts on Why Kevin Stitt Is (Still) Right About the Compact
Print News for the Heart of our City. Volume 57, Issue 9 September 2019 Read us daily at www.city-sentinel.com Ten Cents Page 3 Page 4 Page 5 Page 7 Free elected National Committeewoman A quality inspection is key The Genoveses: Elizabeth and Eugene, Back in the News OKC Zoo’s Art Gone Wild exhibit AN EDITORIAL Fresh Thoughts on Why Kevin Stitt is (still) right about the Compact The City Sentinel Editorial of the Oklahoma definition of slot machines (still considered Governor Kevin Stitt appar- the old-style wooden tumbler ently remains determined to machines that ran here long renegotiate gaming compacts ago). in Oklahoma. Because that is In truth, sweetheart deals the case, leaders of the large between the Big Tribe “play- tribes – fashioned into a co- ers” – operating with virtual alition that benefits only the monopolistic powers after de- haves, and in no instance the cades of dubious federal Trust have-nots – announced recent- decisions – and their middle ly they would rebuff Stitt’s re- men machine vendor pals ben- newed calls for a meeting to efit only … the Big Tribes and discuss this serious matter in a their well connected buddies serious manner. – who have skimmed hundred The powerful supporters of millions from the market of the status quo in Oklaho- Gov. Kevin Stitt through exclusive deals with ma tribal gaming are rejecting taking place in Las Vegas. Vegas machine manufactur- real talks about real issues be- In short, there is plenty of ers by attaching themselves to OCU School of Law Dean Jim Roth (far left) brought his own furry friends, Boo (left) and Brody (right), to meet the students of the 2019 Animal Law class. -

Amicus Curiae the Chickasaw Nation Counsel for Amicus Curiae the Choctaw Nation of FRANK S
No. 18-9526 IN THE Supreme Court of the United States ———— JIMCY MCGIRT, Petitioner, v. STATE OF OKLAHOMA, Respondent. ———— On Writ of Certiorari to the Court of Criminal Appeals of the State of Oklahoma ———— BRIEF OF AMICI CURIAE TOM COLE, BRAD HENRY, GLENN COFFEE, MIKE TURPEN, NEAL MCCALEB, DANNY HILLIARD, MICHAEL STEELE, DANIEL BOREN, T.W. SHANNON, LISA JOHNSON BILLY, THE CHICKASAW NATION, AND THE CHOCTAW NATION OF OKLAHOMA IN SUPPORT OF PETITIONER ———— MICHAEL BURRAGE ROBERT H. HENRY WHITTEN BURRAGE Counsel of Record 512 N. Broadway Avenue ROBERT H. HENRY LAW FIRM Suite 300 512 N. Broadway Avenue Oklahoma City, OK 73102 Suite 230 Oklahoma City, OK 73102 (405) 516-7824 [email protected] Counsel for Amici Curiae [Additional Counsel Listed On Inside Cover] February 11, 2020 WILSON-EPES PRINTING CO., INC. – (202) 789-0096 – WASHINGTON, D. C. 20002 STEPHEN H. GREETHAM BRAD MALLETT Senior Counsel Associate General Counsel CHICKASAW NATION CHOCTAW NATION OF 2929 Lonnie Abbott Blvd. OKLAHOMA Ada, OK 74820 P.O. Box 1210 Durant, OK 74702 Counsel for Amicus Curiae the Chickasaw Nation Counsel for Amicus Curiae the Choctaw Nation of FRANK S. HOLLEMAN, IV Oklahoma DOUGLAS B. ENDRESON SONOSKY, CHAMBERS, SACHSE, ENDRESON & PERRY, LLP 1425 K St., NW Suite 600 Washington, DC 20005 (202) 682-0240 Counsel for Amici Curiae the Chickasaw Nation and the Choctaw Nation of Oklahoma TABLE OF CONTENTS Page TABLE OF AUTHORITIES ................................ ii INTEREST OF AMICI CURIAE ........................ 1 SUMMARY OF ARGUMENT ............................. 5 ARGUMENT ........................................................ 5 I. OKLAHOMA’S AND THE NATIONS’ NEGOTIATED APPROACH TO SET- TLING JURISDICTIONAL ISSUES ON THEIR RESERVATIONS BENEFITS ALL OKLAHOMANS .............................. -

Jane Jayroe-Gamble She Overcame Her Fears and Shyness to Win Miss America 1967, Launching Her Career in Media and Government
Jane Jayroe-Gamble She overcame her fears and shyness to win Miss America 1967, launching her career in media and government Chapter 01 – 0:52 Introduction Announcer: As millions of television viewers watch Jane Jayroe crowned Miss America in 1967, and as Bert Parks serenaded her, no one would have thought she was actually a very shy and reluctant winner. Nor would they know that the tears, which flowed, were more of fright than joy. She was nineteen when her whole life was changed in an instant. Jane went on to become a well-known broadcaster, author, and public official. She worked as an anchor in TV news in Oklahoma City and Dallas, Fort Worth. Oklahoma governor, Frank Keating, appointed her to serve as his Secretary of Tourism. But her story along the way was filled with ups and downs. Listen to Jane Jayroe talk about her struggle with shyness, depression, and a failed marriage. And how she overcame it all to lead a happy and successful life, on this oral history website, VoicesofOklahoma.com. Chapter 02 – 8:30 Grandparents John Erling: My name is John Erling. Today’s date is April 3, 2014. Jane, will you state your full name, your date of birth, and your present age. Jane Jayroe: Jane Anne Jayroe-Gamble. Birthday is October 30, 1946. And I have a hard time remembering my age. JE: Why is that? JJ: I don’t know. I have to call my son, he’s better with numbers. I think I’m sixty-seven. JE: Peggy Helmerich, you know from Tulsa? JJ: I know who she is. -

Senate Members and Their Districts
PART II Senate Members and Their Districts Senate Members and Their Districts 79 Senate Members listed by District Number District Senate Page Number Member Party Number Littlefield, Rick (D) 128 2 Taylor, Stratton (D) 164 3 Rozell, Herb (D) 154 4 Dickerson, Larry (D) 'X) 5 Rabon, Jeff (D) 148 6 Mickel, Billy A. (D) 136 7 Stipe, Gene (D) 162 8 Shurden, Frank (D) 156 9 Robinson, Ben H. (D) 152 10 Harrison, J. Berry (D) 108 11 Homer, Maxine (D) 120 12 Fisher, Ted V. (D) 100 13 Wilkerson, Dick (D) 170 14 Roberts, Darryl F. (D) 150 15 Weedn, Trish (D) 166 16 Hobson, Cal (D) 118 17 Hemy ,Brad (D) 114 18 Easley, Kevin Alan (D) % 19 Milacek, Robert V. (R) 138 Xl Muegge, Paul (D) 144 21 Morgan , Mike (D) 142 22 Gustafson, Bill (R) 104 23 Price, Bruce (D) 146 24 Martin , Carol (R) 134 26 Capps, Gilmer N. (D) 88 29 Dunlap, Jim (R) 94 31 Helton, Sam (D) 110 32 Maddox,Jim (D) 132 33 Williams, Penny (D) 172 34 Campbell, Grover (R) 86 35 Williamson, James (R) 174 37 Long, Lewis (D) 130 38 Kerr, Robert M. (D) 122 ?f) Smith, Jerry L. (R) 158 80 The Almanac of Oklahoma Politics District Senate Page Number Member Party Number 40 Douglass, Brooks (R) 92 41 Snyder, Mark (R) lffi 42 Herbert, Dave (D) 116 43 Brown, Ben (D) 82 44 Leftwich, Keith C. (D) 126 45 Wilcoxson , Kathleen (R) 168 46 Cain, Bernest (D) 84 tfl Fair, Mike (R) 98 48 Monson, Angela (D) 140 49 Laughlin, Owen (R) 124 X) Haney, Enoch Kelly (D) 106 51 Ford, Charles R. -

Note: All Results Are for Rogers County
Note: All results are for Rogers County. Some numbers may be pre-provisional and may be off by a few votes, but do not affect the overall results in any significant way. Source: Rogers County Election Board Archive 1994 Election Cycle Voter Turnout for Special Election for County Question – February 9, 1993 6,616 Voted/41,639 Registered = 15.89% County Question Approving the Extension of a 1% Sales Tax for the Maintenance and Construction of County Roads until 1998 – February 9, 1993 Yes No 4,531 2,048 Voter Turnout for Special Election for SQ No. 659 – February 8, 1994 3,762 Voted/36,404 Registered = 10.33% SQ No. 659: Makes Local School Millage Levies Permanent until Repealed by Voters– February 8, 1994 Yes No 2,295 1,330 Voter Turnout for Special Election for SQ No. 658 – May 10, 1994 12,566 Voted/36,754 Registered = 34.19% SQ No. 658: Approval of a State Lottery with Specifics on How Funds Would Be Controlled – May 10, 1994 Yes No 5,291 7,272 Voter Turnout for Democratic Primary Election – August 23, 1994 7,678 Voted/23,936 Registered = 32.08% Oklahoma Gubernatorial Democratic Primary Results – August 23, 1994 Jack Mildren Danny Williams Bernice Shedrick Joe Vickers 3,284 646 3,312 305 Oklahoma Lieutenant Gubernatorial Democratic Primary Results – August 23, 1994 Dave McBride Walt Roberts Nance Diamond Bob Cullison 1,130 426 2,685 3,183 Oklahoma State Auditor and Inspector Democratic Primary Results – August 23, 1994 Clifton H. Scott Allen Greeson 4,989 1,956 Oklahoma Attorney General Democratic Primary Results – August 23, 1994 John B. -

Ann Holloway
BIOGRAPHICAL INFORMATION ANN HOLLOWAY Ann Holloway, from Ardmore, Oklahoma, was appointed as an Oklahoma State Regent by Governor Mary Fallin in May 2013 to fill an unexpired term. In May 2015, she was reappointed by Governor Mary Fallin for a nine-year term ending in May 2024. The Oklahoma State Regents for Higher Education is the constitutional coordinating board for the Oklahoma colleges and universities responsible for allocating state funds and setting admission standards and academic policies. Regent Holloway was previously appointed in 2000 by Governor Frank Keating to a nine-year term for the Regional University System of Oklahoma (RUSO) Board of Regents. Governor Keating also appointed Regent Holloway to the Professional Responsibility Tribunal for the Oklahoma Bar Association. Regent Holloway was also appointed to various Boards and Commissions by Governor Henry Bellmon. Regent Holloway has been active in many civic and community organizations, including Ardmore Chamber of Commerce, March of Dimes, United Way, Ardmore Little Theater, OK Jaycee Auxiliary (Past President and lifetime member), Committee for Small Business Owners, and Oklahoma Department of Commerce. Regent Holloway has also held, for over 40 years, various positions with the Oklahoma Republican Party. Previous honors for Regent Holloway include Outstanding Young Women of Oklahoma and Who’s Who of Outstanding Women in America. Regent Holloway received an Associate of Science degree from Murray State College, located in Tishomingo, Oklahoma, and a Bachelor of Science degree from Southeastern Oklahoma State University, located in Durant, Oklahoma. Regent Holloway lives in Ardmore, Oklahoma, where she was involved in oil field equipment manufacturing for 25 years. -

Letter to Governor Frank Keating on Disaster Assistance to Oklahoma
Administration of William J. Clinton, 1995 / Apr. 19 663 and play by the rules. Many more financial under this emergency declaration will be institutions will discover new, profitable lines provided at 100 percent Federal funding. of business. And it doesn't cost taxpayers a The Federal Emergency Management dime. It can create miracles in small towns Agency (FEMA) will coordinate Federal as- and big cities from coast to coast, miracles sistance efforts and designate specific areas like mortgage or business loans for people eligible for such assistance. The Federal Co- who never thought they could own a house ordinating Officer will be Mr. Dell Greer of or business, multifamily housing loans, and FEMA. He will consult with you and assist commercial development loans in low to in the execution of the FEMA-State Agree- moderate income communities. ment governing the expenditure of Federal To maximize the benefits that can accrue funds. to both banks and consumers, the final regu- Sincerely, lation issued today by the Office of the Bill Clinton Comptroller of the Currency, the Office of Thrift Supervision, the Board of Governors NOTE: This letter was attached to a statement by of the Federal Reserve, and the Federal De- Press Secretary Mike McCurry announcing disas- posit Insurance Corporation will place em- ter assistance to Oklahoma City, Oklahoma. phasis on performance, not paperwork. The new regulations will make the act easier for banks to implement and will result in more Letter to Federal Emergency consistent evaluation of their performance. Management Agency Director James With these improved regulations in place, the Lee Witt on Disaster Assistance to statute can reach its full potential to help our Oklahoma City, Oklahoma communities help themselves. -

Can't Turn Me Around
CAN’T TURN ME AROUND: AN ORAL HISTORY PLAY by Julie Pearson Little Thunder This play is based on interviews conducted by Dr. Tanya Finchum and Juliana Nykolaiszyn for the Oklahoma Oral History Research Program at Oklahoma State University. It includes first person accounts from nine of the forty-six women in the interview series, who served in the Oklahoma Legislature from 2007-2010. Classroom curriculum and specific lessons are also included in the interview collection. To access written transcripts or audio interviews, go to https://library.okstate.edu/search-and-find/collections/digital- collections/wotol/women-legislators/ This is a public domain play. No royalties are required for performances so long as they are given free of charge. However, any public performance must include a program acknowledgement of the playwright. 1 A NOTE ABOUT STYLE This is a presentational play which can be done Reader’s Theater style or as a memorized performance. Posture, voice and various costume elements such as scarves and jackets can be used to indicate the change from actor to character and vice versa. Because this play relies upon these transitions for its theatrical effect, and to emphasize the fact that the women legislators lines are quotes from their interviews, I distinguish between actors and interviewees by listing one or the other first. For example: Actor #3/LAURA BOYD means the actor starts as herself and then presents Boyd. When the notation is reversed, LAURA BOYD/Actor #3, Boyd gets the emphasis. https://library.okstate.edu/search-and-find/collections/digital- collections/wotol/women-legislators/ 2 CAST OF CHARACTERS Bernice Mitchell and Hannah Atkins/Actor #1 (African Americans) Lisa Johnson Billy/Actor #2 (Native American, Chickasaw) Laura Boyd/Actor #3 (white) Audience member/Actor #4 (white) Kathleen Wilcoxson/ Actor #5 (white) Betty Boyd/Actor #6 (white) 3 ACTOR #3 This is how Bernice Mitchell started out in politics. -

Promoting Healthier Tomorrows Through Education and Research Today Dean’S Message
Promoting healthier tomorrows through education and research today Dean’s Message Dear Alumni and Friends There is a saying – “If it’s not broken, don’t fix it.”That advice may work for appliances, but it doesn’t work for health. We are on the verge of a major realization in our country — that we must shift our focus more to promoting health and wellness, and preventing disease, injury and disability, rather than treating illness. It is a shift that moves us from a reactive to a proactive approach for health. It also is a shift that will not only improve health and save lives, it potentially will save our state and nation billions of dollars a year. The OU College of Public Health is proud to play an important role in educating the new generation of public health professionals to lead our nation in this new direction, in advancing research that furthers these goals, and in preparing public health professionals and volunteers for proper emergency response. We are one of only 38 accredited colleges of public health in the country and home to four federally funded centers that focus on protecting and improving the public’s health: the Southwest Center for Public Health Preparedness, the OU Prevention Research Center, the Center for American Indian Health Research and the Center for Biosecurity Research. Public health is important not only in times of emergency, but every day of every year. Clean air, safe food and clean drinking water, immunizing our children, protecting our communities and promoting healthy lifestyles — these all are critical public health issues. -
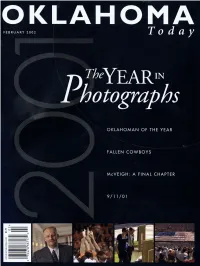
Oklahoma Today February 2002 Volume 52 No. 2: the Year In
OKLAHO FEBRUARY 2002 Today \LAWMAN OF THE YEAR -.. ....__ --- --.__ FALLEN COWBOYS VEIGH: A FINAL CHAPTER Where there's Williams, there's a From building sidewalks in 1908, For nearly a century, to now -building energy pipelines coast-to-coast, our Oklahoma roots building strong relationships every place we call have served us well, home -where there's Williams, there's a way. and helped us serve ourI neighbors and neighborhoods A way to be more than a company- a way to be even better. Though it may sound clichkd, we think a vital part of our community. A way to better our the Williams way of integrity and reliability will be surroundings and ourselves. just as important in our next century. Williams people possessthe powers of ilnaginationand deternrinath, plus a desire to accomplish something significant. That's why we succeed -in our industry and our communities. It's just our way. LeadingEnergy Sdutions, (800)Williams NYSE:WMB williams.com energynewslive.com Route -7 --1 i -- -- -. ,' * I ' The Performance Company Where you will always find good things-- for cars and the people who drive them.TM Q CoWrigM Phillips Petroleum Company, 2MH). 4122-00 THE YEAR IN REVIEW LOUISA MCCUNE Editor in Chicf An Dirmr: STEVEN WALKER, WALKER CREATIVE, INC.; Senior Edimc STEFFIE CORCORAN Auociate EdiMc ANDREA LOPEZ WALKER; Edimdhir*ln&: BROOKE DEMETZ and RYAN MARIE MENDENHW; Editorial Inm: HEATHER SUGRUE;AdvmirngDin&c WALT DISNEY; Account &cutivc~: CHARLOTTE ASHWORTH &KIM RYAN; Advmirng InmSHARON WALKER; hd~cffbnManager: COLLEEN MCINTYRE; Adv&ng GraphicA&: SAND1 WELCH General Manager: MELANIE BREEDEN; Accounrant: LISA BRECKENRIDGE Ofit Manap BECKY ISAAC; @ccAahnt: KATHY FUGATE JOAN HENDERSON Publisher JANE JAYROE, Ewccutiue Dircmr Oklahoma Tourism and Recreation Dqamt Toutinn and Recreation Cmnrnish LT. -

FY-08 Legislative Appropriations
Oklahoma House of Representatives FY‐08 Legislative Appropriations Centennial Edition Fiscal Year 2008 Legislative Appropriations Oklahoma House of Representatives Speaker Lance Cargill Appropriations and Budget Committee Representative Chris Benge, Chairman Representative Ken Miller, Vice Chair July, 2007 Prepared by: House Fiscal Staff Committee and Subcommittee Membership Appropriations and Budget Committee Chris Benge, Chair Ken Miller, Vice Chair John Auffet Guy Liebmann John Carey Bill Nations James Covey Randy Terrill Shane Jett Revenue & Taxation Subcommittee Randy Terrill, Chair Danny Morgan, Vice Chair Dale DeWitt Richard Morrissette Joe Dorman Earl Sears Tad Jones Rules Committee Shane Jett, Chair Bill Nations, Vice Chair James Covey Ryan Kiesel Joe Dorman Greg Piatt Rob Johnson Trebor Worthen Tad Jones Elections & Redistricting Subcommittee Trebor Worthen, Chair Purcy Walker, Vice Chair Dennis Adkins Randy Terrill Ryan McMullen Page i Education Committee Tad Jones, Chair Todd Thomsen, Vice Chair Neil Brannon Sally Kern Ann Coody Ray McCarter Doug Cox Jeannie McDaniel David Dank Eric Proctor Lee Denney Phil Richardson Joe Dorman Jabar Shumate Terry Hyman Dan Sullivan Terry Ingmire Common Education Subcommittee Ann Coody, Chair Neil Brannon, Vice Chair Ed Cannaday Weldon Watson Dale DeWitt Susan Winchester Ray McCarter Higher Education & Career Tech Subcommittee Terry Ingmire, Chair David Derby, Vice Chair Terry Hyman Pam Peterson Charlie Joyner Jabar Shumate Bill Nations Arts & Culture Subcommittee Lee Denney, Chair Ben Sherrer, -

Ally, the Okla- Homa Story, (University of Oklahoma Press 1978), and Oklahoma: a History of Five Centuries (University of Oklahoma Press 1989)
Oklahoma History 750 The following information was excerpted from the work of Arrell Morgan Gibson, specifically, The Okla- homa Story, (University of Oklahoma Press 1978), and Oklahoma: A History of Five Centuries (University of Oklahoma Press 1989). Oklahoma: A History of the Sooner State (University of Oklahoma Press 1964) by Edwin C. McReynolds was also used, along with Muriel Wright’s A Guide to the Indian Tribes of Oklahoma (University of Oklahoma Press 1951), and Don G. Wyckoff’s Oklahoma Archeology: A 1981 Perspective (Uni- versity of Oklahoma, Archeological Survey 1981). • Additional information was provided by Jenk Jones Jr., Tulsa • David Hampton, Tulsa • Office of Archives and Records, Oklahoma Department of Librar- ies • Oklahoma Historical Society. Guide to Oklahoma Museums by David C. Hunt (University of Oklahoma Press, 1981) was used as a reference. 751 A Brief History of Oklahoma The Prehistoric Age Substantial evidence exists to demonstrate the first people were in Oklahoma approximately 11,000 years ago and more than 550 generations of Native Americans have lived here. More than 10,000 prehistoric sites are recorded for the state, and they are estimated to represent about 10 percent of the actual number, according to archaeologist Don G. Wyckoff. Some of these sites pertain to the lives of Oklahoma’s original settlers—the Wichita and Caddo, and perhaps such relative latecomers as the Kiowa Apache, Osage, Kiowa, and Comanche. All of these sites comprise an invaluable resource for learning about Oklahoma’s remarkable and diverse The Clovis people lived Native American heritage. in Oklahoma at the Given the distribution and ages of studies sites, Okla- homa was widely inhabited during prehistory.