138 Cataract Surgery in Children: Controversies and Practices
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accommodation in the Holmes-Adie Syndrome by G
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.21.4.290 on 1 November 1958. Downloaded from J. Neurol. Neurosurg. Psychiat., 1958, 21, 290. ACCOMMODATION IN THE HOLMES-ADIE SYNDROME BY G. F. M. RUSSELL From the Neurological Research Unit, the National Hospital, Queen Square, London In 1936, Bramwell suggested that the title response to near and far vision respectively. But it "Holmes-Adie syndrome" be given to the clinical has also been noted that the reaction to convergence complex of a slowly reacting pupil and absent tendon may be remarkably wide in its range, considering reflexes in recognition of the descriptions by Holmes that it often follows a stage of complete paralysis (1931) and Adie (1932). Both authors had empha- (Strasburger, 1902). Not only is the reaction to sized the chief clinical features-dilatation of the convergence well preserved when compared to the pupil, apparent loss of the reaction to light, slow reaction to light, but it may in fact be excessive constriction and relaxation in response to near and (Alajouanine and Morax, 1938; Heersema and distant vision, and partial loss of the tendon reflexes. Moersch, 1939). In assessing the degree of tonicity Although the syndrome had been recognized wholly there are, therefore, two criteria: slowness ofguest. Protected by copyright. or in part many years previously (Strasburger, 1902; pupillary movement and preservation of the range Saenger, 1902; Nonne, 1902; Markus, 1906; Weill of movement. and Reys, 1926), credit must go to Adie for stressing Adler and Scheie (1940) showed that the tonic the benign nature of the disorder and distinguishing pupil constricts after the conjunctival instillation it clearly from neurosyphilis. -

A Patient & Parent Guide to Strabismus Surgery
A Patient & Parent Guide to Strabismus Surgery By George R. Beauchamp, M.D. Paul R. Mitchell, M.D. Table of Contents: Part I: Background Information 1. Basic Anatomy and Functions of the Extra-ocular Muscles 2. What is Strabismus? 3. What Causes Strabismus? 4. What are the Signs and Symptoms of Strabismus? 5. Why is Strabismus Surgery Performed? Part II: Making a Decision 6. What are the Options in Strabismus Treatment? 7. The Preoperative Consultation 8. Choosing Your Surgeon 9. Risks, Benefits, Limitations and Alternatives to Surgery 10. How is Strabismus Surgery Performed? 11. Timing of Surgery Part III: What to Expect Around the Time of Surgery 12. Before Surgery 13. During Surgery 14. After Surgery 15. What are the Potential Complications? 16. Myths About Strabismus Surgery Part IV: Additional Matters to Consider 17. About Children and Strabismus Surgery 18. About Adults and Strabismus Surgery 19. Why if May be Important to a Person to Have Strabismus Surgery (and How Much) Part V: A Parent’s Perspective on Strabismus Surgery 20. My Son’s Diagnosis and Treatment 21. Growing Up with Strabismus 22. Increasing Signs that Surgery Was Needed 23. Making the Decision to Proceed with Surgery 24. Explaining Eye Surgery to My Son 25. After Surgery Appendix Part I: Background Information Chapter 1: Basic Anatomy and Actions of the Extra-ocular Muscles The muscles that move the eye are called the extra-ocular muscles. There are six of them on each eye. They work together in pairs—complementary (or yoke) muscles pulling the eyes in the same direction(s), and opposites (or antagonists) pulling the eyes in opposite directions. -

Pediatric Ophthalmology/Strabismus 2017-2019
Academy MOC Essentials® Practicing Ophthalmologists Curriculum 2017–2019 Pediatric Ophthalmology/Strabismus *** Pediatric Ophthalmology/Strabismus 2 © AAO 2017-2019 Practicing Ophthalmologists Curriculum Disclaimer and Limitation of Liability As a service to its members and American Board of Ophthalmology (ABO) diplomates, the American Academy of Ophthalmology has developed the Practicing Ophthalmologists Curriculum (POC) as a tool for members to prepare for the Maintenance of Certification (MOC) -related examinations. The Academy provides this material for educational purposes only. The POC should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably directed at obtaining the best results. The physician must make the ultimate judgment about the propriety of the care of a particular patient in light of all the circumstances presented by that patient. The Academy specifically disclaims any and all liability for injury or other damages of any kind, from negligence or otherwise, for any and all claims that may arise out of the use of any information contained herein. References to certain drugs, instruments, and other products in the POC are made for illustrative purposes only and are not intended to constitute an endorsement of such. Such material may include information on applications that are not considered community standard, that reflect indications not included in approved FDA labeling, or that are approved for use only in restricted research settings. The FDA has stated that it is the responsibility of the physician to determine the FDA status of each drug or device he or she wishes to use, and to use them with appropriate patient consent in compliance with applicable law. -

Asymmetries of Dark and Bright Negative Afterimages Are Paralleled by Subcortical on and OFF Poststimulus Responses
1984 • The Journal of Neuroscience, February 22, 2017 • 37(8):1984–1996 Systems/Circuits Asymmetries of Dark and Bright Negative Afterimages Are Paralleled by Subcortical ON and OFF Poststimulus Responses X Hui Li,1,2 X Xu Liu,1,2 X Ian M. Andolina,1 Xiaohong Li,1 Yiliang Lu,1 Lothar Spillmann,3 and Wei Wang1 1Institute of Neuroscience, State Key Laboratory of Neuroscience, Key Laboratory of Primate Neurobiology, Center for Excellence in Brain Science and Intelligence Technology, Chinese Academy of Sciences, Shanghai 200031, China, 2University of Chinese Academy of Sciences, Shanghai 200031, China, and 3Department of Neurology, University of Freiburg, 79085 Freiburg, Germany Humans are more sensitive to luminance decrements than increments, as evidenced by lower thresholds and shorter latencies for dark stimuli. This asymmetry is consistent with results of neurophysiological recordings in dorsal lateral geniculate nucleus (dLGN) and primary visual cortex (V1) of cat and monkey. Specifically, V1 population responses demonstrate that darks elicit higher levels of activation than brights, and the latency of OFF responses in dLGN and V1 is shorter than that of ON responses. The removal of a dark or bright disc often generates the perception of a negative afterimage, and here we ask whether there also exist asymmetries for negative afterimages elicited by dark and bright discs. If so, do the poststimulus responses of subcortical ON and OFF cells parallel such afterimage asymmetries? To test these hypotheses, we performed psychophysical experiments in humans and single-cell/S-potential recordings in cat dLGN. Psychophysically, we found that bright afterimages elicited by luminance decrements are stronger and last longer than dark afterimages elicited by luminance increments of equal sizes. -

Cone Contributions to Signals for Accommodation and the Relationship to Refractive Error
Vision Research 46 (2006) 3079–3089 www.elsevier.com/locate/visres Cone contributions to signals for accommodation and the relationship to refractive error Frances J. Rucker ¤, Philip B. Kruger Schnurmacher Institute for Vision Research, State University of New York, State College of Optometry, 33 West 42nd Street, New York, NY 10036, USA Received 18 February 2005; received in revised form 7 April 2006 Abstract The accommodation response is sensitive to the chromatic properties of the stimulus, a sensitivity presumed to be related to making use of the longitudinal chromatic aberration of the eye to decode the sign of the defocus. Thus, the relative sensitivity to the long- (L) and middle-wavelength (M) cones may inXuence accommodation and may also be related to an individual’s refractive error. Accommodation was measured continuously while subjects viewed a sine wave grating (2.2 c/d) that had diVerent cone contrast ratios. Seven conditions tested loci that form a circle with equal vector length (0.27) at 0, 22.5, 45, 67.5, 90, 120, 145 deg. An eighth condition produced an empty Weld stimulus (CIE (x,y) co-ordinates (0.4554, 0.3835)). Each of the gratings moved at 0.2 Hz sinusoidally between 1.00 D and 3.00 D for 40 s, while the eVects of longitudinal chromatic aberration were neutralized with an achromatizing lens. Both the mean level of accommo- dation and the gain of the accommodative response, to sinusoidal movements of the stimulus, depended on the relative L and M cone sen- sitivity: Individuals more sensitive to L-cone stimulation showed a higher level of accommodation (p D 0.01; F D 12.05; ANOVA) and dynamic gain was higher for gratings with relatively more L-cone contrast. -

Care of the Patient with Accommodative and Vergence Dysfunction
OPTOMETRIC CLINICAL PRACTICE GUIDELINE Care of the Patient with Accommodative and Vergence Dysfunction OPTOMETRY: THE PRIMARY EYE CARE PROFESSION Doctors of optometry are independent primary health care providers who examine, diagnose, treat, and manage diseases and disorders of the visual system, the eye, and associated structures as well as diagnose related systemic conditions. Optometrists provide more than two-thirds of the primary eye care services in the United States. They are more widely distributed geographically than other eye care providers and are readily accessible for the delivery of eye and vision care services. There are approximately 36,000 full-time-equivalent doctors of optometry currently in practice in the United States. Optometrists practice in more than 6,500 communities across the United States, serving as the sole primary eye care providers in more than 3,500 communities. The mission of the profession of optometry is to fulfill the vision and eye care needs of the public through clinical care, research, and education, all of which enhance the quality of life. OPTOMETRIC CLINICAL PRACTICE GUIDELINE CARE OF THE PATIENT WITH ACCOMMODATIVE AND VERGENCE DYSFUNCTION Reference Guide for Clinicians Prepared by the American Optometric Association Consensus Panel on Care of the Patient with Accommodative and Vergence Dysfunction: Jeffrey S. Cooper, M.S., O.D., Principal Author Carole R. Burns, O.D. Susan A. Cotter, O.D. Kent M. Daum, O.D., Ph.D. John R. Griffin, M.S., O.D. Mitchell M. Scheiman, O.D. Revised by: Jeffrey S. Cooper, M.S., O.D. December 2010 Reviewed by the AOA Clinical Guidelines Coordinating Committee: David A. -

Pediatric Cataracts: a Retrospective Study of 12 Years (2004
Pediatric Cataracts: A Retrospective Study of 12 Years (2004 - 2016) Cataratas em Idade Pediátrica: Estudo Retrospetivo de 12 ARTIGO ORIGINAL Anos (2004 - 2016) Jorge MOREIRA1, Isabel RIBEIRO1, Ágata MOTA1, Rita GONÇALVES1, Pedro COELHO1, Tiago MAIO1, Paula TENEDÓRIO1 Acta Med Port 2017 Mar;30(3):169-174 ▪ https://doi.org/10.20344/amp.8223 ABSTRACT Introduction: Cataracts are a major cause of preventable childhood blindness. Visual prognosis of these patients depends on a prompt therapeutic approach. Understanding pediatric cataracts epidemiology is of great importance for the implementation of programs of primary prevention and early diagnosis. Material and Methods: We reviewed the clinical cases of pediatric cataracts diagnosed in the last 12 years at Hospital Pedro Hispano, in Porto. Results: We identified 42 cases of pediatric cataracts with an equal gender distribution. The mean age at diagnosis was 6 years and 64.3% of patients had bilateral disease. Decreased visual acuity was the commonest presenting sign (36.8%) followed by leucocoria (26.3%). The etiology was unknown in 59.5% of cases and there was a slight predominance of nuclear type cataract (32.5%). Cataract was associated with systemic diseases in 23.8% of cases and with ocular abnormalities in 33.3% of cases. 47.6% of patients were treated surgically. Postoperative complications occurred in 35% of cases and posterior capsular opacification was the most common (25%). Discussion: The report of 42 cases is probably the result of the low prevalence of cataracts in this age. Although the limitations of our study include small sample size, the profile of children with cataracts in our hospital has characteristics relatively similar to those described in the literature. -
Pupils and Near Vision
PUPILS AND NEAR VISION Akilesh Gokul PhD Research Fellow Department of Ophthalmology Iris Anatomy Two muscles: • Radially oriented dilator (actually a myo-epithelium) - like the spokes of a wagon wheel • Sphincter/constrictor Pupillary Reflex • Size of pupil determined by balance between parasympathetic and sympathetic input • Parasympathetic constricts the pupil via sphincter muscle • Sympathetic dilates the pupil via dilator muscle • Response to light mediated by parasympathetic; • Increased innervation = pupil constriction • Decreased innervation = pupil dilation Parasympathetic Pathway 1. Three major divisions of neurons: • Afferent division 2. • Interneuron division • Efferent division Near response: • Convergence 3. • Accommodation • Pupillary constriction Pupil Light Parasympathetic – Afferent Pathway 1. • Retinal ganglion cells travel via the optic nerve leaving the optic tracts 2. before the LGB, and synapse in the pre-tectal nucleus. 3. Pupil Light Parasympathetic – Efferent Pathway 1. • Pre-tectal nucleus nerve fibres partially decussate to innervate both Edinger- 2. Westphal (EW) nuclei. • E-W nucleus to ipsilateral ciliary ganglion. Fibres travel via inferior division of III cranial nerve to ciliary ganglion via nerve to inferior oblique muscle. 3. • Ciliary ganglion via short ciliary nerves to innervate sphincter pupillae muscle. Near response: 1. Increased accommodation Pupil 2. Convergence 3. Pupillary constriction Sympathetic pathway • From hypothalamus uncrossed fibres 1. down brainstem to terminate in ciliospinal centre -
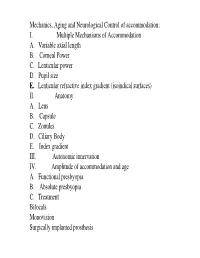
I. Multiple Mechanisms of Accommodation A. Variable Axial Length B
Mechanics, Aging and Neurological Control of accommodation: I. Multiple Mechanisms of Accommodation A. Variable axial length B. Corneal Power C. Lenticular power D. Pupil size E. Lenticular refractive index gradient (isoindical surfaces) II. Anatomy A. Lens B. Capsule C. Zonules D. Ciliary Body E. Index gradient III. Autonomic innervation IV. Amplitude of accommodation and age A. Functional presbyopia B. Absolute presbyopia C. Treatment Bifocals Monovision Surgically implanted prosthesis Course title - (VS217) Oculomotor functions and neurology Instructor - Clifton Schor GSI: James O’Shea, Michael Oliver & Aleks Polosukhina Schedule of lectures, exams and laboratories : Lecture hours 10-11:30 Tu Th; 5 min break at 11:00 Labs Friday the first 3 weeks Examination Schedule : Quizes: January 29; February 28 Midterm: February 14: Final March 13 Power point lecture slides are available on a CD Resources: text books, reader , website, handouts Class Website: Reader. Website http://schorlab.berkeley.edu Click courses 117 class page name VS117 password Hering,1 First Week: read chapters 16-18 See lecture outline in syllabus Labs begin this Friday, January 25 Course Goals Near Response - Current developments in optometry Myopia control – environmental, surgical, pharmaceutical and genetic Presbyopia treatment – amelioration and prosthetic treatment Developmental disorders (amblyopia and strabismus) Reading disorders Ergonomics- computers and sports vision Virtual reality and personal computer eye-ware Neurology screening- Primary care gate keeper neurology, systemic, endocrines, metabolic, muscular skeletal systems. Mechanics, Aging and Neurological Control of accommodation : I. Five Mechanisms of Accommodation A. Variable axial length B. Corneal Power and astigmatism C. Lenticular power D. Pupil size & Aberrations E. Lenticular refractive index gradient (isoindical surfaces) II. -

Pediatric Glaucoma
CLINICAL STRATEGIES Pediatric Glaucoma Advice on diagnosing and managing a rare but potentially devastating group of diseases. BY SHARON F. FREEDMAN, MD hildhood glaucomas are infrequently encoun- try between the corneas of the infant’s eyes. Rapid corneal tered by many eye care providers and can there- stretching may lead to breaks in Descemet’s membrane fore be challenging to diagnose. Because this het- called Haab’s striae, which will leave permanent scars Cerogeneous group of diseases can cause a rapid (Figure 1). Oftentimes, the affected infant is photophobic loss of vision or even blindness, however, the timely recog- (Figure 2) and may have tearing that the clinician must dis- nition and optimal treatment of pediatric glaucoma is criti- tinguish from nasolacrimal duct obstruction.1,2 cal. Fortunately, ophthalmologists often have at their dis- Newborns with healthy eyes have a corneal diameter of posal the tools needed to diagnose and begin to manage approximately 9.5 to 10.0 mm. A corneal diameter of these children. Usually, the ideal care of patients with pedi- greater than 12.0 mm in any infant younger than 1 year is atric glaucoma involves the efforts of more than one oph- therefore suspicious for glaucoma.3 The IOP usually thalmologist, unless a pediatric glaucoma specialist is locat- ranges from 10 to 15 mm Hg in newborns, whereas the ed near the child’s home. IOP in children of school age resembles that of adults. Most children with glaucoma will have an IOP that is BACKGROUND higher than 22 mm Hg. The most common form of pediatric glaucoma, primary Although infants and children under the age of 2 often congenital glaucoma, occurs in approximately one in present with signs and symptoms related to rapid ocular 10,000 individuals.1 As with adult forms of the disease, expansion under high IOP, older children without an acute- pediatric glaucoma may be primary or secondary. -

AAPOS – SPOSI Joint Meeting, Jaipur, India, Preliminary Program – Subject to Changes
AAPOS – SPOSI Joint Meeting, Jaipur, India, Preliminary Program – Subject to changes Friday, December 2, 2016 9:00 AM – 9:05 AM Opening Remarks & Welcome Room A and Room B Sean P. Donahue, MD, PhD 9:05 AM – 10:35 AM Childhood Visual Impairment: Detection, Assessment, and Rehabilitation Room A and Room B 9:05 AM – 9:41 AM Blindness and Prevention of Visual Impairment in Children 9:05 AM – 9:06 AM Introduction Sherwin J. Isenberg, MD 9:06 AM – 9:24 AM Childhood Blindness World Wide: Current Status Clare Gilbert, MB ChB, FRCOphth, MD, MSc 9:24 AM – 9:32 AM The NGO’s Role in Treating and Preventing Blindness Marilyn T. Miller, MD Victoria Sheffield, President and CEO, International Eye Foundation 9:32 AM – 9:38 AM Epidemiology of Eye Disease in Children Birth to 3 in a Tertiary Eye Center in India P. Vijayalakshmi, MS, DO 9:38 AM – 9:41 AM Question and Answer Session 9:41 AM – 10:06 AM Early Detection and Assessment of Visual Impairment in Children 9:41 AM – 9:42 AM Introduction Linda Lawrence, MD 9:42 AM – 9:57 AM How the Pediatric Ophthalmologist Diagnoses CVI and Why? Gordon Dutton, MD, FRCS Ed (hon), FRCOphth 9:57 AM – 10:03 AM Early Detection Should Lead to Early Intervention; Rural Initiatives Kalpana Narendran, MBBS, DO, DNB 10:03 AM – 10:06 AM Question and Answer Session 10:06 AM – 10:35 AM Rehabilitation for Children with Visual Impairment 10:06 AM – 10:07 AM Introduction Albert Biglan, MD 10:07 AM – 10:17 AM Interventions from the Ophthalmologist’s Perspective Lea Hyvärinen, MD, PhD 10:17 AM – 10:25 AM Interventions from the Rehabilitation -

Abnormal Red Reflex: Etiologies in a Pediatric Ophthalmology Population
CPJXXX10.1177/0009922820916892Clinical PediatricsLin et al 916892research-article2020 Article Clinical Pediatrics 2020, Vol. 59(8) 760 –765 Abnormal Red Reflex: Etiologies in a © The Author(s) 2020 Article reuse guidelines: sagepub.com/journals-permissions Pediatric Ophthalmology Population DOI:https://doi.org/10.1177/0009922820916892 10.1177/0009922820916892 journals.sagepub.com/home/cpj Sophie Y. Lin, BA1 , Kimberly G. Yen, MD1,2, Huirong Zhu, PhD2, Alexis Moisiuc, BS2, and Madhuri Chilakapati, MD1,2 Abstract Children who present with an abnormal red reflex (ARR) are often referred to ophthalmology due to concern for retinoblastoma. However, an ARR can indicate a wide variety of pathologies, all of which have the potential to develop amblyopia and irreversible vision loss. In this retrospective cohort study, we demonstrate that children who presented with an ARR had a mean age of 22.0 ± 32.5 months and were more frequently referred by their pediatricians (74.5%). The majority of these patients (61.8%) had a normal examination on further evaluation, followed by refractive error (20.4%). Amblyopia was diagnosed in 83.9% of patients with refractive error, with a mean age of 50.3 ± 49.2 months. Because many ARR-associated pathologies require time-sensitive treatment to prevent vision loss, proper screening is critical for diagnosis. Pediatricians play a key role in screening, so education on more common ARR pathologies can better facilitate referrals and improve outcomes. Keywords abnormal red reflex, leukocoria, screening Introduction to any ocular condition that limits visual stimulation to the eye so if amblyopia is not treated early, vision loss Eliciting the red reflex is a useful clinical test used by can be irreversible.