An Introduction to the Legal Structures of the NHS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

South Warwickshire NHS Foundation Trust Annual Report and Accounts
South Warwickshire NHS Foundation Trust Annual Report and Accounts for 2014/15 South Warwickshire NHS Foundation Trust Annual Report and Accounts for 2014/15 Presented to Parliament pursuant to Schedule 7, paragraph 25 (4) (a) of the National Health Service Act 2006 2 Content Introduction: pages 3-5 Section 2: Directors’ Report pages 69-90 Chief Executive’s message Chairman’s message - Directors’ Statement - Appointments and Roles Section 1: Strategic Report pages 6-68 - Board Profiles and Register of Interest - About the Trust - Executive Leadership Structure - Trust Structure - Disclosure of Corporate Governance Arrangements - Service Profile / Principal - Board Statements Activities - Board Committees - Strategy - Board and Committee - 2014/15 objectives Membership - Business Review - Directors’ Remuneration and Review of 2014/15 Pension Benefits objectives Trust performance Section 3: Council of Governors and against national Membership pages 91-112 targets Quality - Council of Governors Structure - Governor Profiles Key Developments in - Map of Constituencies 2013/14 - Meetings of the Council of Financial Performance Governors Review - Sub-committees of the Council of - Risks and Uncertainties Governors - Trends and Factors affecting the - Trust Membership Trust - Partnerships, Stakeholders and Section 4: Quality Report pages 113- Key Strategic Relationships 218 - Corporate Activity Data Part 1: Statement on Quality Part 2: Priorities for Improvement and Serious Untoward Assurance Statements Incidents Part 3: Review of Quality Performance Information Governance Section 5: Statement of Accounting Patient Experience Officers’ Responsibilities and Annual Workforce Governance Statement pages 219- Social, Community and 233 Human Rights Current Developments Section 6: Summary of Financial Environmental and Statements & Auditor’s Statement Sustainability pages 234-242 3 Chief Executive’s Message The end of another financial year provides an opportunity to reflect and to re- focus. -

Burton Role Name Brief Biography Panel Chair Ruth May Dr
Burton Role Name Brief Biography Panel Chair Ruth May Dr Ruth May is NHS England Regional Director of Nursing for Midlands and East. Her previous roles include Chief Nurse for NHS Midlands and East and Chief Nurse for NHS East of England. Ruth has a theatre nursing background and more than 20 years experience of working in the NHS. Patient/Public Representative Norma Armston Norma Armston has a wide range of experience as a patient/carer representative at both local and national level. She has been involved in reviewing cancer services and was a lay assessor in the Clinical Commissioning Group authorisation process. Patient/Public Representative Alan Keys Alan Keys is Lay Member for PPI on the board of High Weald Lewes Havens CCG. He is also a member of various other groups including the British Heart Foundation Prevention and Care Reference. Patient/Public Representative Leon Pollock Leon Pollock is a management consultant with over 30 years experience during which he has assisted more than 250 organisations, including 20 NHS trusts. He is Lay Adviser for Health Education West Midlands and Lay Assessor for the NHS Commissioning Board. Doctor Balraj Appedou Balraj Appedou is a consultant in anaesthesia and intensive care medicine at the Peterborough and Stamford Hospitals NHS Foundation Trust. Balraj is currently Lead for Clinical Governance in the Theatres Anaesthesia and Critical Care Medicine Directorate. Balraj has also been the Patient Safety Champion in the Trust. Doctor Mike Lambert Mr. Mike Lambert is a consultant at Norfolk and Norwich University Hospital and Honorary Senior Lecturer at Norwich Medical School. -

NHS Foundation Trusts 29 APRIL 2003 in the Health and Social Care (Community Health and Standards) Bill Bill 70 of 2002-3
RESEARCH PAPER 03/38 NHS Foundation Trusts 29 APRIL 2003 in the Health and Social Care (Community Health and Standards) Bill Bill 70 of 2002-3 Part I of the Bill makes provision for a new type of NHS organisation in England, to be known as an NHS Foundation Trust. The Bill provides for these bodies to be regulated by a new non-ministerial department, to be called the Independent Regulator for NHS Foundation Trusts, and to have a new sort of constitution that would include a directly elected board of governors. Other Parts of the Bill will be covered in separate Library publications. Jo Roll SOCIAL POLICY SECTION HOUSE OF COMMONS LIBRARY Recent Library Research Papers include: 03/21 The Northern Ireland Assembly Elections Bill [Bill 74 of 2002-03] 13.03.03 03/22 Iraq: developments since UN Security Council Resolution 1441 13.03.03 03/23 The Convention on the Future of Europe: proposals for a 18.03.03 European Constitution 03/24 The Female Genital Mutilation Bill [Bill 21 of 2002-03] 19.03.03 03/25 The Waste and Emissions Trading Bill [Bill 66 of 2002-03] 19.03.03 03/26 Unemployment by Constituency, February 2003-03-20 19.03.03 03/27 The Licensing Bill [HL] [Bill 73 of 2002-03] 20.03.03 03/28 Ballistic Missile Defence 26.03.03 03/29 The Sustainable Energy Bill [Bill 20 of 2002-03] 26.03.03 03/30 The Crime (International Cooperation) Bill [HL] 28.03.03 [Bill 78 of 2002-03] 03/31 The Crime (International Cooperation) Bill [HL]: 'Hot Surveillance' 28.03.03 [Bill 78 of 2002-03] 03/32 Parliamentary Questions, Debate Contributions and Participation -

NHS Vale of York Clinical Commissioning Group Financial Performance Report
NHS Vale of York Clinical Commissioning Group Financial Performance Report Report produced: January 2016 Financial Period: April - December 2015 Summary of Key Financial Measures Year to Date Forecast Outturn Target Actual Variance RAG Target Actual Variance RAG Indicator £000 £000 £000 rating £000 £000 £000 rating Achieve planned surplus 2,959 132 -2,826 A 3,945 -7,351 -11,296 R Programme expenditure does not exceed 329,983 330,428 -445 R 429,695 437,956 -8,261 R programme allocation Running costs expenditure does not exceed running 5,701 5,124 577 G 7,602 6,692 910 G costs allocation Risk adjusted surplus 3,945 -7,351 -11,296 R QIPP delivery (see section 5) Better Payment Practice Code (Value) 95.00% 99.58% 4.58% G 95.00% >95% 0.00% G Better Payment Practice Code (Number) 95.00% 97.19% 2.19% G 95.00% >95% 0.00% G Cash balance at month end is within 1.5% of monthly 464 16 448 G drawdown CCG cash drawdown does not exceed maximum 437,321 437,321 0 G cash drawdown Note – The first 3 metrics correspond to those reported in Note 42 of the Annual Accounts, and represent the statutory duties of the CCG. The full finance dashboard is presented in Appendix 1 Key Messages - The CCG is currently classed as an organisation in turnaround due to the deteriorating financial position. - The CCG is forecasting a year end deficit of £7.35m, which is £11.30m below plan. This position includes several significant variances which are detailed in section 3. -

Board of Directors - Open
Board of Directors - Open Date: 12 August 2020 Item Ref: 05 TITLE OF PAPER Chief Executive’s Report TO BE PRESENTED BY Jan Ditheridge ACTION REQUIRED The Board are asked to consider the impact and opportunity of the letter from Sir Simon Stevens and Amanda Pritchard regarding the third phase of the NHS response to CoVid on our strategic priorities and risks. The Board are asked to approve the recommendation re Executive lead for Inequalities. The Board are asked if there are any other issues that arise from the letter from Sir Simon Stevens and Amanda Pritchard we should consider. The Board are asked to consider the National Guardian Freedom to Speak Up Index Report 2020 and if they feel confident where and how we are addressing the issues it raises for us. The Board are asked to consider the NHS People Plan 2020/21, and where we may want the People Committee to focus attentions as an organisation, given our risks and challenges and as a contributor to our health and care system. The Board are asked to consider the direction of travel of the Accountable Care Partnership; and to understand the key priorities and how they relate to our own transformation programme. The Board are asked to acknowledge the Board role changes, consider any opportunities or risks within the changes and join me in thanking individuals for their contributions and wish them well where they have changed or moved into different roles. OUTCOME To update the Board on key policies, issues and events and to stimulate debate regarding potential impact on our strategy and levels of assurance. -

Clinical Commissioning Group Governing Body Members: Role Outlines, Attributes and Skills
Clinical commissioning group governing body members: Role outlines, attributes and skills October 2012 Clinical commissioning group governing body members: Roles outlines, attributes and skills First published by the NHS Commissioning Board Authority: July 2012 Published by the NHS Commissioning Board: October 2012 This supersedes the version published in July 2012 This version incorporates The National Health Service (Clinical Commissioning Groups) Regulations 2012 S.I. 2012/16311. 1 http://www.legislation.gov.uk/uksi/2012/1631/contents/made 2 [Page left intentionally blank] 3 Contents 1. Introduction .............................................................................................................. 5 2. Core role outline – for all governing body members ................................................. 7 3. Additional information for each specified member.................................................. 10 GP or other healthcare professionals acting on behalf of member practices ............. 12 Chair of the governing body ....................................................................................... 13 Lay member on the governing body – with a lead role in overseeing key elements of financial management and audit ................................................................................ 15 Lay member on the governing body – with a lead role in championing patient and public involvement ..................................................................................................... 17 Clinical member on -

Oversight of NHS-Controlled Providers: Guidance February 2018
Oversight of NHS-controlled providers: guidance February 2018 We support providers to give patients safe, high quality, compassionate care within local health systems that are financially sustainable. Contents 1. Summary ................................................................................... 2 2. Our oversight of NHS-controlled providers ................................ 3 Annex A: NHS-controlled provider licence conditions .................... 7 1 | > Contents 1. Summary The NHS provider licence is a key part of NHS Improvement’s regulatory and oversight system (in this document, references to NHS Improvement are to Monitor and the NHS Trust Development Authority, TDA). Following the Health and Social Care Act 2012 (the Act), Monitor consulted on the first set of provider licence conditions for NHS foundation trusts and independent providers in 2013 and started issuing licences to foundation trusts in April 2013. Independent providers have been required to hold a licence since April 2014. Although NHS trusts are not legally required to hold a licence, in practice NHS Improvement applies the key conditions of the licence to NHS trusts, in line with the principles of the Single Oversight Framework (SOF) for NHS trusts and foundation trusts (collectively referred to as NHS providers). Following consultation between 13 September and 12 October 2017, we are extending our oversight of NHS-controlled providers, as outlined in section 2. 2 | > Oversight of NHS-controlled providers: our policy position 2. Our oversight of NHS- controlled providers 2.1 Why oversee NHS-controlled providers? NHS foundation trusts’ principal purpose is to provide goods and services for the purposes of the NHS in England. They are not-for-profit, public benefit corporations created to devolve decision-making from central government to local organisations and communities. -

UNDERSTANDING the NEW NHS a Guide for Everyone Working and Training Within the NHS 2 Contents 3
England UNDERSTANDING THE NEW NHS A guide for everyone working and training within the NHS 2 Contents 3 NHS ENGLAND INFORMATION READER BOX Introduction 4 Directorate ◆ The NHS belongs to us all Medical Operations Patients and information Nursing Policy Commissioning development Foreword (Sir Bruce Keogh) 5 Finance Human resources NHS values 6 Publications Gateway Reference: 01486 ◆ NHS values and the NHS Constitution Document purpose Resources ◆ An overview of the Health and Social Care Act 2012 Document name Understanding The New NHS Structure of the NHS in England 8 Author NHS England ◆ The structure of the NHS in England Publication date 26 June 2014 ◆ Finance in the NHS: your questions answered Target audience Running the NHS 12 ◆ Commissioning in the NHS Additional circulation Clinicians working and training within the NHS, allied ◆ Delivering NHS services list health professionals, GPs ◆ Health and wellbeing in the NHS Description An updated guide on the structure and function of Monitoring the NHS 17 the NHS, taking into account the changes of the Health and Social Care Act 2012 ◆ Lessons learned and taking responsibility ◆ Regulation and monitoring in the NHS Action required None Contact details for Dr Felicity Taylor Working in the NHS 20 further information National Medical Director's Clinical ◆ Better training, better care Fellow, Medical Directorate Skipton House NHS leadership 21 80 London Road SE1 6LH ◆ Leading healthcare excellence www.england.nhs.uk/nhsguide/ Quality and innovation in the NHS 22 ◆ High-quality care for all Document status This is a controlled document. While this document may be printed, the The NHS in the United Kingdom 24 electronic version posted on the intranet is the controlled copy. -

NHS Long Term Plan (Pdf)
Long-Term Plan Long-Term Plan Long-Term The NHS Long Term Plan Plan Long-Term Plan #NHSLongTermPlan www.longtermplan.nhs.uk [email protected] www.longtermplan.nhs.uk #NHSLongTermPlan January 2019 The NHS Long Term Plan 3 Contents THE NHS LONG TERM PLAN – OVERVIEW AND SUMMARY 6 CHAPTER 1: A NEW SERVICE MODEL FOR THE 21ST CENTURY 11 1. We will boost ‘out-of-hospital’ care, and finally dissolve the historic divide 13 between primary and community health services A new NHS offer of urgent community response and recovery support 14 Primary care networks of local GP practices and community teams 14 Guaranteed NHS support to people living in care homes 15 Supporting people to age well 16 2. The NHS will reduce pressure on emergency hospital services 18 Pre-hospital urgent care 19 Reforms to hospital emergency care – Same Day Emergency Care 21 Cutting delays in patients being able to go home 23 3. People will get more control over their own health and more personalised 24 care when they need it 4. Digitally-enabled primary and outpatient care will go mainstream 25 across the NHS 5. Local NHS organisations will increasingly focus on population health – 29 moving to Integrated Care Systems everywhere CHAPTER 2: MORE NHS ACTION ON PREVENTION AND HEALTH INEQUALITIES 33 Smoking 34 Obesity 36 Alcohol 38 Air pollution 38 Antimicrobial resistance 39 Stronger NHS action on health inequalities 39 CHAPTER 3: FURTHER PROGRESS ON CARE QUALITY AND OUTCOMES 44 A strong start in life for children and young people 45 Maternity and neonatal services 46 Children -

South Central Strategic Health Authority 2012-13 Annual Report and Accounts
South Central Strategic Health Authority 2012-13 Annual Report and Accounts You may re-use the text of this document (not including logos) free of charge in any format or medium, under the terms of the Open Government Licence. To view this licence, visit www.nationalarchives.gov.uk/doc/open-government-licence/ © Crown copyright Published to gov.uk, in PDF format only. www.gov.uk/dh 2 South Central Strategic Health Authority 2012-13 Annual Report and Accounts 3 South Central Strategic Health Authority Annual Report 2012/13 The three Strategic Health Authorities (SHAs) in the South of England – South Central, South East Coast and South West – merged to form one SHA for the South of England in October 2011. However, three versions of the annual report have been produced because each individual SHA is a statutory body and therefore required to produce an annual report. Each report should be read in conjunction with the SHA handover documents: ● Maintaining and improving quality during transition: handover document ● Operational Handover and Closedown Report Chairman and Chief Executive’s Foreword This year has been a challenging and busy time for the NHS and the South of England has been no exception. As new NHS structures have emerged, staff have worked hard to set up new systems and develop new working relationships while continuing to deliver the demands of their current roles without interruption. All parts of the NHS across the South of England have worked together to sustain and improve the quality of services delivered and to leave a strong legacy so that all the new Chairman Dr Geoff Harris OBE Clinical Commissioning Groups will start without debt. -
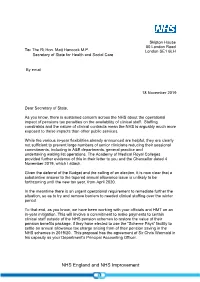
Letter from Simon Stevens to Matt Hancock on 18 November 2019
Skipton House 80 London Road To: The Rt Hon. Matt Hancock M.P. London SE1 6LH Secretary of State for Health and Social Care By email 18 November 2019 Dear Secretary of State, As you know, there is sustained concern across the NHS about the operational impact of pensions tax penalties on the availability of clinical staff. Staffing constraints and the nature of clinical contracts mean the NHS is arguably much more exposed to these impacts than other public services. While the various in-year flexibilities already announced are helpful, they are clearly not sufficient to prevent large numbers of senior clinicians reducing their sessional commitments, including in A&E departments, general practice and undertaking waiting list operations. The Academy of Medical Royal Colleges provided further evidence of this in their letter to you and the Chancellor dated 4 November 2019, which I attach. Given the deferral of the Budget and the calling of an election, it is now clear that a substantive answer to the tapered annual allowance issue is unlikely to be forthcoming until the new tax year, from April 2020. In the meantime there is an urgent operational requirement to remediate further the situation, so as to try and remove barriers to needed clinical staffing over the winter period. To that end, as you know, we have been working with your officials and HMT on an in-year mitigation. This will involve a commitment to make payments to certain clinical staff outside of the NHS pension schemes to restore the value of their pension benefits package, if they have elected to use the “Scheme Pays” facility to settle an annual allowance tax charge arising from of their pension saving in the NHS schemes in 2019/20. -

Novel Coronavirus (COVID-19): Derby and Derbyshire Stakeholder Bulletin #32
View this email in your browser 6 November 2020 Novel Coronavirus (COVID-19): Derby and Derbyshire stakeholder bulletin #32 Dear partners Any doubt as to the seriousness of the situation we now find ourselves in was firmly put to bed on Saturday when the Prime Minister announced plans for a planned four-week lockdown in England from Thursday (5 November) at a Downing Street news conference on Saturday. On Wednesday, MPs overwhelmingly voted to proceed with the second lockdown (516 votes to 38) that is due to end on Wednesday 2 December. NHS Chief Executive, Sir Simon Stevens, also confirmed at a press conference on Wednesday that the NHS in England will be returning to its highest state of alert from midnight on Wednesday to coincide with the start of the second lockdown. The switch to level 4 means the NHS’s response to the resurgence of the pandemic is being handled nationally rather than regionally. The number of people seriously ill with coronavirus who are being treated in hospitals in England has risen from 2,000 at the end of September to almost 11,000. In Derbyshire there were over 200 patients with coronavirus in our hospitals at the end of last week and we are above that now. We’re seeing significant use of Intensive Care Unit beds in Chesterfield which means they can do less of their planned care operating. General practice remains incredibly busy and we are seeing an increase in: NHS 111 use Community nursing and community beds The total number of staff absences related to COVID Our projections tell us that we are approaching April levels for admissions, though lockdown will stem this.