Comparative Indicators of Population Health and Health Care Use for Manitoba’S Regional Health Authorities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Lands Envrironment Action Fund Toolkit
Lands Environmental Action Fund (LEAF) Manitoba First Nations ENVIRONMENT ECONOMY EMPLOYMENT 2014 CREATING OPPORTUNITIES Creating Environmental Economic Opportunities 2014 Produced by: David Lane, DMCL Environmental Anupam Sharma, Director of Operations, DOTC Robert Daniels, CEO, DOTC This project would not have been possible without generous support and guidance from the Dakota Ojibway Tribal Council, the members of the DOTC Council of Chiefs, and key individuals in their respective communities (Birdtail Sioux First Nation, Dakota Tipi First Nation, Long Plain First Nation, Roseau River Anishinabe First Nation, Sandy Bay Ojibway First Nation, Swan Lake First Nation, and Waywaysecappo First Nation). The information contained within this toolkit is collected from and considered to be part of the public domain. Dakota Ojibway Tribal Council offers this guide without any warranty of any kind, either express or implied. Nor does Dakota Ojibway Tribal Council assume any liability for any damages arising from the use of this product. Dakota Ojibway Tribal Council Head Office Long Plain Reserve #6, Band #287 Room 230, 2nd Floor 5010 Crescent Road West Portage la Prairie, MB Mailing Address: P.O. Box 338 Portage la Prairie, MB R1N 3B7 Website: www.dotc.mb.ca Aboriginal Affairs and Northern Development Canada, through the Lands Environmental Action Fund (LEAF), provided funding for this project. March 2014 Lands Environmental Action Fund (LEAF) 2 Creating Environmental Economic Opportunities 2014 CONTENTS: INTRODUCTION .......................................................................................................... -
Assembly of First Nations Mitigating Climate Change
Assembly of First Nations Mitigating Climate Change Community Success in Developing Energy Efficiency and Renewable Energy Projects Assembly of First Nations Table of Contents Acknowledgements........................................................................................................... 3 Introduction....................................................................................................................... 4 Hupacasath First Nation Micro-hydro Plant..................................................................... 6 Taku River Tlingit Power Station..................................................................................... 8 Nacho Nyak Dun Government House ............................................................................ 10 Xeni Gwet'in First Nation Solar Power Project.............................................................. 11 Rolling River Health Centre CBIP Project..................................................................... 14 Rolling River First Nation Wind-Monitoring Project..................................................... 15 Skownan Home Energy Efficiency Workshop Project................................................... 16 Swan Lake Community Energy Baseline Project........................................................... 17 Swan Lake First Nation Wind-Monitoring Project......................................................... 18 Chakastapaysin and Peter Chapman First Nations Independent Power Production....... 19 Black Lake Denesuline Nation Hydro Project............................................................... -

Since 1985, Stars Has Flown More Than 45,000 Missions Across Western Canada
2019/20 Missions SINCE 1985, STARS HAS FLOWN MORE THAN 45,000 MISSIONS ACROSS WESTERN CANADA. Below are 760 STARS missions carried out during 2019/20 from our base in Winnipeg. MANITOBA 760 Alonsa 2 Altona 14 Amaranth 2 Anola 2 Arborg 4 Ashern 15 Austin 2 Bacon Ridge 2 Balsam Harbour 1 Beausejour 14 Benito 1 Beulah 1 Birds Hill 2 Black River First Nation 2 Bloodvein First Nation 6 Blumenort 1 Boissevain 3 Bowsman 1 Brandon 16 Brereton Lake 3 Brokenhead Ojibway Nation 1 Brunkild 2 Caddy Lake 1 Carberry 1 Carman 4 Cartwright 1 Clandeboye 1 Cracknell 1 Crane River 1 Crystal City 6 Dacotah 3 Dakota Plains First Nation 1 Dauphin 23 Dog Creek 4 Douglas 1 Dufresne 2 East Selkirk 1 Ebb and Flow First Nation 2 Edrans 1 Elphinstone 1 Eriksdale 9 Fairford 2 Falcon Lake 1 Fannystelle 1 Fisher Branch 1 Fisher River Cree Nation 4 Fort Alexander 3 Fortier 1 Foxwarren 1 Fraserwood 2 Garson 1 Gilbert Plains 1 Gimli 15 Giroux 1 Gladstone 1 Glenboro 2 Grand Marais 2 Grandview 1 Grosse Isle 1 Grunthal 5 Gypsumville 3 Hadashville 3 Hartney 1 Hazelridge 1 Headingley 5 Hilbre 1 Hodgson 21 Hollow Water First Nation 3 Ile des Chênes 3 Jackhead 1 Keeseekoowenin Ojibway First Nation 1 Kelwood 1 Kenton 1 Killarney 8 Kirkness 1 Kleefeld 1 La Rivière 1 La Salle 1 Lac du Bonnet 3 Landmark 3 Langruth 1 Lenore 1 Libau 1 Little Grand Rapids 3 Little Saskatchewan First Nation 7 Lockport 2 Long Plain First Nation 5 Lorette 3 Lowe Farm 1 Lundar 3 MacGregor 1 Manigotagan 2 Manitou 3 Marchand 2 Mariapolis 1 McCreary 1 Middlebro 5 Milner Ridge 2 Minnedosa 4 Minto 1 Mitchell -

Download Keymap
Nabel Nueltin Lake Lake COLVIN LAKE NUELTIN LAKE CARIBOU RIVER PROVINCIAL PARK Nejanilini Shannon PARK RESERVE HUDSON Lake PROVINCIAL PARK Lake Cochrane R North Seal River Seal Churchill Nicklin River L Shethanei BAY Lake Lac Brochet Tadoule Lake Whiskey Jack Lake River North WAPUSK Knife Seal Lake Churchill River NATIONAL NUMAYKOOS SAND LAKESSouth PROVINCIAL P ARK PROVINCIAL PARK PARK Big Reindeer Sand Lake Lake Northern Southern Indian Lake Thorsteinson Churchill Lake Fidler River Indian Lake Port Nelson Vandekerckhove Goldsand Gauer Barrington Lake Lake Lake Lake Lake River Opachuanau Lake AMISK PARK RESERVE Waskaiowaka River River River Baldock Lake Stephens Lake Lake Rat Gods Leaf Rapids Granville Nelson Russell Lake Split Lake River Rat Mynarski Lake Lakes Lake Hayes Highrock Lake Churchill THOMPSON PAINT LAKE PROVINCIAL PARK EAST PAINT LAKE PARK RESERVE River Sipiwesk Knee Lake River Lake Oxford River Edmund Snow Lake Lake Lake Cross Gods Wekusko Grass FLIN FLON Lake Walker Grass Sucker Lake Lake GRASS RIVER PROVINCIAL PARK Lake Sharpe Lake Red Red Sucker Lake Molson Lake R North Moose CLEARWATER Lake LAKE Nelson PROVINCIAL PARK Island Playgreen L Lake THE PAS LITTLE LIMESTONE LAKE PROVINCIAL PARK Cedar WALTER COOK UPLANDS CAVES ECOLOGICAL LAKE RESERVE TOWN OF Lake GRAND RAPIDS WINNIPEG L A C L W A K I E N W N I I GRAND ISLAND N P RED DEER N PARK RESERVE E I SOUTHERN MANITOBA MUNICIPAL P G GOOSE ISLANDS PEMICAN ISLAND E O PARK RESERVE PARK RESERVE G S O I MOUNTAIN S S (NORTH) I S Swan KEY MAP BIRCH ISLAND R Lake CHITEK LAKE PARK RESERVE PROVINCIAL PARK SWAN Berens LAKE Bowsman MINITONAS- River DUCK Fishing SWAN BOWSMAN BAY VALLEY Swan River L Minitonas WESTSwan KINWOW BAY PARK RESERVE LAKE Benito WATERHEN ST MARTIN MOUNTAIN STURGEON BAY (SOUTH) HOMEBROOK- PARK RESERVE ATIKAKI PEONAN POINT GRAHAMDALE FISHER BAY DUCK MOUNTAIN Lake PARK PROVINCIAL PARK Winnipegosis PROVINCIAL RESERVE LAKE ETHELBERT St. -

Manitoba Regional Health Authority (RHA) DISTRICTS MCHP Area Definitions for the Period 2002 to 2012
Manitoba Regional Health Authority (RHA) DISTRICTS MCHP Area Definitions for the period 2002 to 2012 The following list identifies the RHAs and RHA Districts in Manitoba between the period 2002 and 2012. The 11 RHAs are listed using major headings with numbers and include the MCHP - Manitoba Health codes that identify them. RHA Districts are listed under the RHA heading and include the Municipal codes that identify them. Changes / modifications to these definitions and the use of postal codes in definitions are noted where relevant. 1. CENTRAL (A - 40) Note: In the fall of 2002, Central changed their districts, going from 8 to 9 districts. The changes are noted below, beside the appropriate district area. Seven Regions (A1S) (* 2002 changed code from A8 to A1S *) '063' - Lakeview RM '166' - Westbourne RM '167' - Gladstone Town '206' - Alonsa RM 'A18' - Sandy Bay FN Cartier/SFX (A1C) (* 2002 changed name from MacDonald/Cartier, and code from A4 to A1C *) '021' - Cartier RM '321' - Headingley RM '127' - St. Francois Xavier RM Portage (A1P) (* 2002 changed code from A7 to A1P *) '090' - Macgregor Village '089' - North Norfolk RM (* 2002 added area from Seven Regions district *) '098' - Portage La Prairie RM '099' - Portage La Prairie City 'A33' - Dakota Tipi FN 'A05' - Dakota Plains FN 'A04' - Long Plain FN Carman (A2C) (* 2002 changed code from A2 to A2C *) '034' - Carman Town '033' - Dufferin RM '053' - Grey RM '112' - Roland RM '195' - St. Claude Village '158' - Thompson RM 1 Manitoba Regional Health Authority (RHA) DISTRICTS MCHP Area -

Aboriginal Organizations and with Manitoba Education, Citizenship and Youth
ABORIGINAL ORGANIZATIONS IN MANITOBA A Directory of Groups and Programs Organized by or for First Nations, Inuit and Metis People 2011/2013 ABORIGINAL ORGANIZATIONS IN MANITOBA A Directory of Groups and Programs Organized by or for First Nations, Inuit and Métis People 2011 / 2013 ________________________________________________________________ Compiled and edited by Aboriginal Education Directorate and Aboriginal Friendship Committee Fort Garry United Church Winnipeg, Manitoba Printed by Aboriginal Education Directorate Manitoba Education, Manitoba Advanced Education and Literacy and Aboriginal Affairs Secretariat Manitoba Aboriginal and Northern Affairs INTRODUCTION The directory of Aboriginal organizations is designed as a useful reference and resource book to assist people to locate the appropriate organizations and services. The directory also serves as a means of improving communications among people. The idea for the directory arose from the desire to make information about Aboriginal organizations more available to the public. This directory was first published in 1975 and has grown considerably since its initial edition, which had 16 pages compared to the 100 pages of the present edition. The directory reflects the vitality and diversity of Aboriginal cultural traditions, organizations, and enterprises. The editorial committee has made every effort to present in this directory an accurate and up-to-date listing. Fax numbers, Email addresses and Websites have been included whenever available. Inevitably, errors and omissions will have occurred in the revising and updating of this Directory, and the committee would greatly appreciate receiving information about such oversights, as well as changes and new information to be included in a future revision. Please call, fax or write to the Aboriginal Friendship Committee, Fort Garry United Church, using the information on the next page. -
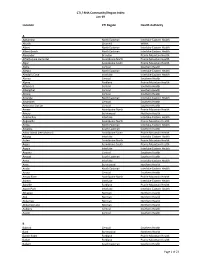
CTI / RHA Community/Region Index Jan-19
CTI / RHA Community/Region Index Jan-19 Location CTI Region Health Authority A Aghaming North Eastman Interlake-Eastern Health Akudik Churchill WRHA Albert North Eastman Interlake-Eastern Health Albert Beach North Eastman Interlake-Eastern Health Alexander Brandon Prairie Mountain Health Alfretta (see Hamiota) Assiniboine North Prairie Mountain Health Algar Assiniboine South Prairie Mountain Health Alpha Central Southern Health Allegra North Eastman Interlake-Eastern Health Almdal's Cove Interlake Interlake-Eastern Health Alonsa Central Southern Health Alpine Parkland Prairie Mountain Health Altamont Central Southern Health Albergthal Central Southern Health Altona Central Southern Health Amanda North Eastman Interlake-Eastern Health Amaranth Central Southern Health Ambroise Station Central Southern Health Ameer Assiniboine North Prairie Mountain Health Amery Burntwood Northern Health Anama Bay Interlake Interlake-Eastern Health Angusville Assiniboine North Prairie Mountain Health Anola North Eastman Interlake-Eastern Health Arbakka South Eastman Southern Health Arbor Island (see Morton) Assiniboine South Prairie Mountain Health Arborg Interlake Interlake-Eastern Health Arden Assiniboine North Prairie Mountain Health Argue Assiniboine South Prairie Mountain Health Argyle Interlake Interlake-Eastern Health Arizona Central Southern Health Amaud South Eastman Southern Health Ames Interlake Interlake-Eastern Health Amot Burntwood Northern Health Anola North Eastman Interlake-Eastern Health Arona Central Southern Health Arrow River Assiniboine -
Market Housing Program
Achieving the Right Balance CANDO’s 24th Annual Conference – October 23, 2017 Fredericton, New Brunswick 1 The Fund’s Vision Every First Nation family has the opportunity to have a home on their own land in a strong community. 2 ©2008 FNMHF 3 ©2008 FNMHF # of First Nation Applications Received by the Fund / Total # of FNs in each Prov./ Territories (as of September 30, 2017) 9/14 2/33 84/202 18/47 16/63 13/75 13/40 65/134 12/35 ©2008 FNMHF First Nations announced for Credit Enhancement as of October 5, 2017 • Miawpukek, NF •Siksika, AB •Neskonlith, BC •Penelakut, BC • Membertou, NS • T’it’q’et, BC • Nipissing, ON • Nooaitch, BC • Lac La Ronge, SK • Eastmain, QC • Mississauga, ON • Skeetchestn, BC • Batchewana, ON • Tsawout, BC • Wemindji, QC • Kwanlin Dün, YT • Onion Lake, SK • Sagamok, ON • Henvey Inlet, ON • Sechelt, BC • Atikameksheng, ON • Seabird Island, BC • Beausoleil, ON •Teslin Tlingit Council, YT Anishnawbek, ON • Tk’emlups, BC • Wahnapitae, ON • Tsartlip First Nation, BC • Whitefish River, ON • Moose Cree, ON • Temagami, ON • Tr'ondëk Hwëch'in, YT • Champagne & • Serpent River, ON • Carcross/Tagish, YT Aishihik, YT • Curve Lake, ON • Penticton, BC • Skidegate, BC • Pic River, ON • Mohawks of the Bay • Aundeck Omni • Quatsino, BC • Lac Seul, ON of Quinte, ON Kaning, ON • Little Shuswap ,BC • Waswanipi, QC • Adams Lake, BC • Long Plain, MB • Mistissini, QC • Flying Dust, SK • Garden River, ON • Skwah, BC •Saugeen, ON • Okanagan, BC • Lower Nicola, BC • Fisher River, MB •Wahta, ON • Chisasibi, QC • Upper Nicola, BC •Alderville, ON •Mattagami, ON • Chippewas of • Hiawatha, ON • Lake Cowichan, BC •Chapleau Cree, ON Nawash, ON • M’Chigeeng, ON •Leq’á:mél, BC •Nuxalk, BC • Simpcw, BC • ʔaq'am (St. -

Municipality of Minitonas-Bowsman
MUNICIPALITY OF MINITONAS-BOWSMAN Date: April 4, 2017 Regular Meeting of the members of Council of the Municipality of Minitonas-Bowsman held in Council Chambers, in Minitonas, Manitoba this 4th day of April, 2017 A.D. at 7:00 p.m. Present: Reeve: Clint Eisner Councillors: J. Caruk, C. Densen, L. Hutman, L. Mychalchuk, S. Walmsley, & G. Bartel C.A.O. – K. Chartrand Delegations: 7:30 pm - Bill Jacobs – Utility Bill 7:45 pm – Ken Malley – Minitonas Fire Department Additions to Agenda: 4.17 Sludge Reduction at Lagoon Proposal 4.18 South Shop Quote – Repair Work 4.19 Employee Matters 4.20 Animal Control 4.21 Mutual Aid Request 1. L. Mychalchuk & L. Hutman RESOLVED THAT the Agenda be adopted as amended. Carried. 2. J. Caruk – G. Bartel RESOLVED THAT the members of the Municipality of Minitonas-Bowsman Council do hereby agree to go ‘In Camera’ as a Committee of the Whole in accordance with Subsection 152(3)(b)(ii) of The Municipal Act. Carried. 3. S. Walmsley – L. Mychalchuk RESOLVED THAT we do agree to return to reopen the meeting to the public in accordance with Subsection 152(4) of the Municipal Act. Carried. 4. L. Mychalchuk – S. Walmsley RESOLVED THAT the minutes of the Regular Meeting of Council held on March 21st, 2017 shall be adopted as circulated. Carried. 1 5. L. Mychalchuk – L. Hutman RESOLVED THAT the Financial Statement for the month ending December 31st, 2016 shall be approved as presented. Carried. 6. J. Caruk – C. Densen RESOLVED THAT the Council of the Municipality of Minitonas-Bowsman does hereby approve the Staff Expense Report as submitted. -

Page 1 of 3 MANITOBA FIRST NATIONS POLICE SERVICE
MANITOBA FIRST NATIONS POLICE SERVICE (DAKOTA OJIBWAY POLICE SERVICE) History The original establishment of the Dakota Ojibway Tribal Council Police Department, now known as the Dakota Ojibway Police Service, dated December 1974, was prepared and agreed to by all Chiefs of the D.O.T.C. After three years of negotiations, funding was approved by the different levels of government. In November of 1977, the police department commenced operations with one Chief of Police and nine members. The program was funded by Indian & Northern Affairs Canada from 1977 to 1993. The development of the Police Service was to establish local control and accountability to the First Nation communities. In November of 1993, the Police Service ceased operations due to a lack of funding commitment from the Province of Manitoba. Tripartite negotiations reconvened in 1994 and technical meetings took place as follows: March 10, May 12, May 26 and June 23, 1994. On May 19, 1994, the D.O.T.C. Council of Chiefs and representatives from both levels of Government, Manitoba Justice and Public Safety Canada were able to secure an Interim Policing Service Agreement which saw the restoration of joining policing services (D.O.P.S./R.C.M.P.) to (7) seven of the (8) eight D.O.T.C. Member First Nation communities, with the effective start date of June 1, 1994. On December 31, 1994, a long-term Tripartite Agreement was finalized and on February 1, 1995, the Dakota Ojibway Police Service resumed full-time policing services to (6) six D.O.T.C. First Nation communities: Birdtail Sioux First Nation, Dakota Plains Wahpeton Nation, Long Plain First Nation, Canupawakpa Dakota Nation, Roseau River Anishinabe First Nation and Sioux Valley Dakota Nation. -

Teachersrecruitmentbooklet
SWAN VALLEY SCHOOL DIVISION Educating and Inspiring All Learners WHO WE ARE The Swan Valley School Division is located in the South Western part of Manitoba. The Division Office is located in Swan River. The Division has a total enrollment of about 1,500 students. The Division serves the communities of Benito, Birch River, Bowsman, Minitonas and Swan River. The Division also provides high school programming to Wuskwi Sipihk First Nation. The School Division operates the following schools: Benito School K - 8 Birch River School K - 8 Bowsman School K - 8 Minitonas Early Years School K - 4 Minitonas Middle Years School 5 - 8 Heyes Elementary School K - 6 Taylor Elementary School K - 5 Ecole Swan River South School K - 8 dual track Swan Valley Regional Secondary School 9 - 12 BASIC FACTS Budget 21 million Pupil/Teacher Ratio 11.9 FTE Teachers 118 FTE Educational Assistants 68 SWAN VALLEY SCHOOL DIVISION Enrollment 1,500 Bus Routes 30 Starting Teacher Salary - Class 5 $59,025 – Sept 2017 Educating and Inspiring All Learners Educating and Inspiring All Learners PROFESSIONAL VOCATION PROGRAMS DEVELOPMENT The School Division’s Regional The Division supports educators Secondary School offers a wide by providing ongoing professional variety of Vocational Programs. development. The Division’s PD Many of these programs are ma- Committee is largely comprised of triculated with the University teachers. The PD Committee has College of the North, which oper- significant input into the Division- ates a Satellite Campus next to the al PD initiatives during the year. school. Students can receive Level In addition, teachers can select 1 credit from Apprenticeship and personal PD opportunities both the College for a number of the within the Division or outside of vocational programs. -
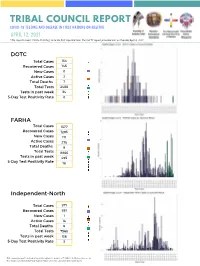
Copy of Green and Teal Simple Grid Elementary School Book Report
TRIBAL COUNCIL REPORT COVID-19 TESTING AND DISEASE IN FIRST NATIONS ON RESERVE APRIL 12, 2021 *The reports covers COVID-19 testing since the first reported case. The last TC report provided was on Tuesday April 6, 2021. DOTC Total Cases 154 Recovered Cases 145 New Cases 0 Active Cases 2 Total Deaths 7 Total Tests 2488 Tests in past week 34 5-Day Test Positivity Rate 0 FARHA Total Cases 1577 Recovered Cases 1293 New Cases 111 Active Cases 275 Total Deaths 9 Total Tests 8866 Tests in past week 495 5-Day Test Positivity Rate 18 Independent-North Total Cases 871 Recovered Cases 851 New Cases 1 Active Cases 14 Total Deaths 6 Total Tests 7568 Tests in past week 136 5-Day Test Positivity Rate 3 This summary report is intended to provide high-level analysis of COVID-19 testing and disease in First Nations on reserve by Tribal Council Region since first case until date noted above. APRIL 12, 2021 Independent- South Total Cases 218 Recovered Cases 214 New Cases 1 Active Cases 2 Total Deaths 2 Total Tests 1932 Tests in past week 30 5-Day Test Positivity Rate 6 IRTC Total Cases 380 Recovered Cases 370 New Cases 0 Active Cases 1 Total Deaths 9 Total Tests 3781 Tests in past week 55 5-Day Test Positivity Rate 0 KTC Total Cases 1011 Recovered Cases 948 New Cases 39 Active Cases 55 Total Deaths 8 Total Tests 7926 Tests in past week 391 5-Day Test Positivity Rate 10 This summary report is intended to provide high-level analysis of COVID-19 testing and disease in First Nations on reserve by Tribal Council Region since first case until date noted above.