IFPA Program 2015 Brisbane 7 Sept
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RSC 2018 Seminar Bios
Royal Society of Canada Eastern Ontario Regional Seminar Saturday, April 14, 2018, Queen’s University Club, 168 Stuart St, Kingston, ON All Presentations are Free and Open to the Public 10:00 am: Peter Milliken: The Role of the Speaker of the House of Commons Peter Milliken was born in Kingston and after high school he attended Queen’s University beginning in 1964 studying Politics and Economics. He graduated in 1968 and went to Oxford University to study law where he earned a B.A. in 1970 then went to Dalhousie University to get an LL.B. in 1971. He practiced law in Kingston after his call to the Bar in 1973 until 1988 when he was elected M.P. for Kingston and the Islands. He served in the House of Commons until 2011 as M.P. and was Deputy Speaker from 1996 until 2000 and was elected Speaker in 2001 and reelected in 2004, 2006 and 2008 and served until his retirement in 2011. Milliken also has the unique distinction of being the first Speaker to preside over four Parliaments. His legacy includes his landmark rulings on Parliament’s right to information, which are key elements of parliamentary precedent both in Canada and throughout the Commonwealth. He currently resides in Kingston enjoying retirement. 11:00 am: Stéphanie Bélanger: War Trauma, Culture of War and Soldier Identity Dr. Bélanger is the Associate Scientific Director of the Canadian Institute for Military and Veteran Health Research, a unique consortium of 43 Canadian universities dedicated to researching the health needs of military personnel, Veterans and their families. -

BIOM 6070 – Pregnancy, Birth and Perinatal Adaptation Spring/Summer 2016 University of Guelph (Seminar Course Only)
Page 1 of 3 PREGNANCY: Graduate Course 2016 BMED 829 – Pregnancy, Queen’s University (Seminar and Laboratory Course) Meeting in Videoconference Room 155 at the School of Medicine (SoM) or as announced BIOM 6070 – Pregnancy, Birth and Perinatal Adaptation Spring/Summer 2016 University of Guelph (Seminar Course only). Meeting in videoconference room-location to be announced Course Coordinators Queen’s University: Dr. Anne Croy, DVM, PhD. ([email protected])-seminars B924 Dr. Chandra Tayade, DVM, PhD. ([email protected])-laboratory B860 University of Guelph: Dr. Jon LaMarre, DVM, PhD. ([email protected])-seminars OVC 3606 Dr. Rami Kridli, DVM, PhD. ([email protected]) OVC 2602 Clinical Participants: Dr. Graeme Smith, Department of Obstetrics and Gynecology, [email protected] Dr. Michael Flavin, Department of Pediatrics, [email protected] University of Guelph Scheduler: Ms. Kim Best, Secretary, Dept. Biomedical Sciences [email protected] Videoconference Support: Queens: [email protected] U. Guelph: Jim Hare [email protected] or [email protected] Part I of the Course: A Literature Review and Discussion Based Component Tuesday May 3 First Class Meeting – 9.30 – 10.30 – Videoconferene Room 155 SoM, Queen’s Guelph & Queen’s University linked with Ontario Veterinary College PATH4838 Reading List Topic #1 assigned. Discuss grant writing elective topic task, value of memberships in learned societies. Thursday, May 5 Queen’s Grand Rounds, Obstetrics and Gynecology with Reproduction Research Group. ONLY. Room to be announced. 7:30-8:30 AM. Guest Dr. Kelle Moley, James P. Crane Professor of Obstetrics and Gynecology; Director of the Division of Basic Science Research, Department of Obstetrics and Gynecology, Washington University, St. -

DBMS Graduate Program Proposal
NEW GRADUATE PROGRAM PROPOSAL Submission Form This template is to be used when seeking approval for new Graduate programs of study leading to a degree. New program submissions must receive the approval of the Graduate Studies Executive Council (GSEC) prior to being externally reviewed. The submission, external review, and the internal response to the review will, as a package, be submitted by GSEC to the Senate Office for referral to the Senate Committee on Academic Development (SCAD) which will then make their recommendations to Senate. Academic Units are strongly advised to contact the Director of the Office of the Vice-Provost and Dean SGS or the appropriate Associate Dean in the SGS with any questions that arise during this proposal development. Refer also to the QUQAP website at: http://www.queensu.ca/provost/responsibilities/qualityassurance.html. NOTE: the textboxes in this template will expand as needed. Part A – General Summary Name of Proposed Programs: Graduate Programs in Biomedical and Molecular Sciences [MSc (Anatomical Sciences), MSc and PhD] Unit(s): Department of Biomedical and Molecular Sciences (DBMS) Proposed Start Date: September 2014 Contact Information (1) Contact Information (2) Name: Louise Winn Name: Anne Tobin Title: Professor Title: DBMS Program Coordinator Associate Head DBMS, Post Graduate Education Unit: DBMS Unit: DBMS E-mail: [email protected] E-mail: [email protected] GRAD New DBMS Program Proposal 19Nov2012.doc Page 1 of 81 Executive Summary (1 page maximum suggested) Briefly summarize the rationale for introducing the new Programs and how they fit with the academic goals of the Faculty/School and University (i.e. -

Engraftment of Bone Marrow from Severe Combined Immunodeficient
Published January 19, 1998 Engraftment of Bone Marrow from Severe Combined Immunodeficient (SCID) Mice Reverses the Reproductive Deficits in Natural Killer Cell–deficient tge26 Mice By Marie-Josée Guimond,* Baoping Wang,‡ and B. Anne Croy* From the *Department of Biomedical Sciences, Ontario Veterinary College, University of Guelph, Guelph, Ontario, Canada N1G 2W1; and the ‡Division of Immunology, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts 02215 Summary A large, transient population of natural killer (NK) cells appears in the murine uterine mesome- trial triangle during pregnancy. Depletion of uterine (u) NK cells, recently achieved using gene-ablated and transgenic mice, results in pathology. Pregnancies from matings of homozy- gous NK and T cell–deficient tge26 mice have ,1% of normal uNK cell frequency, no devel- opment of an implantation site–associated metrial gland, and an edematous decidua with vascu- lar pathology that includes abnormally high vessel walls/lumens ratios. Fetal loss of 64% occurs midgestation and placentae are small. None of these features are seen in pregnant T cell–defi- Downloaded from cient mice. To confirm the role of the NK cell deficiency in these reproductive deficits, trans- plantation of tge26 females was undertaken using bone marrow from B and T cell–deficient scid/scid donors. Engrafted pregnant females have restoration of the uNK cell population, in- duced metrial gland differentiation, reduced anomalies in the decidua and decidual blood ves- sels, increased placental sizes, and restoration of fetal viability at all gestational days studied (days 10, 12, and 14). Thus, uNK cells appear to have critical functions in pregnancy that promote decidual health, the appropriate vascularization of implantation sites, and placental size. -
Program, We Have Added a Few New Themes to the Program, Increasing the Number of These Concurrent Sessions to 12 in 2017
Co-Hosted by : WELCOME DELEGATES Welcome to the 4th Annual Canadian National Perinatal Research Meeting (CNPRM). We are delighted that you have all decided to join us for exciting and novel science and great fun at the Fairmont Montebello, Quebec! As you may know, although the CNPRM is only in its fourth year, Canadian perinatal researchers have been meeting yearly for nearly 40 years as Western and Eastern groups, and in February 2014 we came together to form a Canadian National meeting that was held in Banff. It was so successful that this new national annual format was adopted for the 2015 (Montebello) and 2016 (Banff) meetings and has formed the basis for the 2017 meeting as well. The 2017 meeting has achieved record numbers of registrants and trainees, which is evidence of Canada’s vibrant and growing perinatal research community, and our immense contribution to perinatal research and our role in the global effort of supporting and maintaining maternal and child health and policy. This year we have 384 registered delegates and 275 submitted abstracts (65 oral and 210 poster trainee presentations - A big thank you to all the members of the Thematic Committees who judged the submission). We also have three world-class international Plenary speakers, and for this year’s scientific program, we have added a few new themes to the program, increasing the number of these concurrent sessions to 12 in 2017. As in previous years, the meeting in 2017 will host two evening poster sessions; as well, for the first time this year, eight special interest workshop sessions will be included, with topics ranging from how to secure that first faculty position to topics such as neonatal feeding and improving neonatal care with the help of veteran parents. -

Guelph Conundrum
ISSN 0229-2378 gue p h UNIVERSITY NEWS BULLETIN Volume 29 Number 28 August 1, 1985 The limited awareness of Guelph programs The extends beyond the academic into extra-curricular actitivities as well. Well over 80 per cent of all survey respondents had never heard of such campus events as Guelph College Royal, March Counselling, Guelph Interaction or Summer Orientation. The study also examined the impact of the conundrum Heather Cooper poster and the image it portrays. Recognition of the poster was high among students Although everyone surveyed had heard of and teachers, with most reporting they had seen it in Guelph, knowledge of the programs it offers varied a high school classroom, hallway or guidance office. greatly. Teachers were more aware of the broad Only a few of the parents remembered having seen range of programs available than students and parents the poster before. Although some respondents who — a finding that is understandable, says Wardlaw, had seen it did not remember the sponsoring univer- because much of Guelph's liaison material is directed sity, most made the association. through teachers. Almost everyone agreed that the poster is beauti- Guelph was best known among respondents for ful and memorable. Many teachers said the print is se its agriculture and veterinary medicine programs, but popular, in fact, that it is frequently stolen by stu- there was also strong recognition of its biological dents off school hallway walls. sciences. When asked which of 14 Ontario univer- When asked whether they think Guelph should sities was academically superior in the biological continue to use the poster or find something new, sciences, the largest percentage of the respondents 72 per cent of the students favored continued use of (30 per cent) said Guelph. -
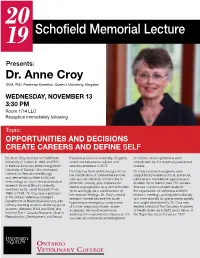
Schofield Memorial Lecture
20 19 Schofield Memorial Lecture Presents: Dr. Anne Croy DVM, PhD. Professor Emeritus, Queen’s University, Kingston WEDNESDAY, NOVEMBER 13 3:30 PM Room 1714 LLC Reception immediately following Topic: OPPORTUNITIES AND DECISIONS CREATE CAREERS AND DEFINE SELF Dr. Anne Croy received her DVM from Function at Queen’s University, Kingston of children whose gestations were University of Guelph in 1969 and PhD where she became an adjunct and complicated by this maternally-presented in Medical Sciences (Immunology) from emeritus professor in 2017. disease. University of Toronto. She developed Dr. Croy has been widely recognized for Dr. Croy’s research programs were interests in Reproductive Biology her identification of uterine Natural Killer supported by numerous local, provincial, and uterine Natural Killer (uNK) cell cells and her definition of their roles in national and international agencies and immunology as a part-time postdoctoral promotion of early, post-implantation enabled her to mentor over 120 trainees. research fellow at Brock University, uterine angiogenesis using animal models She has chaired and participated in mentored by Dr. Janet Rossant. From (mice and pigs). As a consequence of the organization of numerous scientific 1985 to 2004, Dr. Croy was a professor her research findings, Dr. Croy’s central research meetings, participated nationally in the Ontario Veterinary College’s research interest became the acute, and internationally on grants review panels Department of Biomedical Sciences with hypertensive emergency complication and taught internationally. Dr. Croy was primary teaching duties in veterinary gross of human pregnancy known as pre- elected a fellow of the Canadian Academy anatomy. Between 2004 and 2016, she eclampsia. -
Pregnancy Differentiation and Function During IFN Regulatory
Assessment of Requirements for IL-15 and IFN Regulatory Factors in Uterine NK Cell Differentiation and Function During Pregnancy This information is current as of October 7, 2021. Ali A. Ashkar, Gordon P. Black, Qingxia Wei, Hong He, Luchuan Liang, Judith R. Head and B. Anne Croy J Immunol 2003; 171:2937-2944; ; doi: 10.4049/jimmunol.171.6.2937 http://www.jimmunol.org/content/171/6/2937 Downloaded from References This article cites 42 articles, 12 of which you can access for free at: http://www.jimmunol.org/content/171/6/2937.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on October 7, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2003 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Assessment of Requirements for IL-15 and IFN Regulatory Factors in Uterine NK Cell Differentiation and Function During Pregnancy1 Ali A. Ashkar,2* Gordon P. -

The Biomeder
November, 2019 Vol. 38 THE V O L . 3 6 BIOMEDER The official newsletter of the Department of Biomedical Sciences I N T H I S I S S U E Happy Fall! The Fall semester is in full swing (26 more A BIOMED HALLOWEEN! sleeps till X-mas!). I want to wish you all the best in your teaching and continued productivity ALICIA AT BANTING and success in your research. To give you a greater sense of satisfaction, here are just some CONGRATS KATHERINE! of the numbers to show you where Biomeders are making the greatest impact: ANNE CROY GIVES Our 21 faculty teach 26 courses/semester to: SCHOFILED LECTURE Bio-med Major = 913 students Neuroscience Major = 250 students MARTINO IN MONTREAL! DVM = 483 students Grad student corner Graduate students supervised = 87 (PhD = 26; MSc = 35; MBS = 26) Upcoming events in 4th year research project students = 29 Biomed (We teach over 6,500 students/year in our courses!) . ..and much more! Keep up the great work Biomed!!! Halloween in Biomed A huge "Thank you" to our graduate student representatives for the United Way Campaign, Simran Bhullar and Shahnaza Hamidullah for hosting a departmental Halloween coffee and cake event to raise donations for United Way. A Biomed Halloween... Dr. Alicia Viloria-Petit celebrates her Banting success Dr. Viloria-Petit attended the 2019 Launching Discovery Event of the Banting Research Foundation On Tuesday September 10th, award recipients, volunteers, and friends of The Banting Research Foundation came together to celebrate a successful year at the Foundation. The event took place at the Faculty Club of the University of Toronto. -
![University Photograph Collection 1947-2012 [Non-Inclusive] UA 17](https://docslib.b-cdn.net/cover/8023/university-photograph-collection-1947-2012-non-inclusive-ua-17-7238023.webp)
University Photograph Collection 1947-2012 [Non-Inclusive] UA 17
University Photograph Collection 1947-2012 UA 17 Brock University Archives University Photograph Collection 1947-2012 [non-inclusive] UA 17 Brock University Archives Creator: Brock University and others as noted. Extent: 3246 contact sheets : b&w and col. 4937 bw photographs 15598 col photographs 33050 bw negatives 24933 col negatives 2325 transparencies : b&w and col. 79430 slides : b&w and col. 1374 compact discs with 56337 digital images Abstract: This collection consists of photographs created, collected and compiled by the University photographers, Office of External Relations, and University Marketing & Communications staff and others from the beginnings of the concept of a university for Niagara in 1963 to 2012. Materials: Contact sheets, photographs, negatives, transparencies, slides and compact discs containing digital images. Repository: Brock University Archives Processed by: Edie Williams Finding Aid: Edie Williams Last Updated: April 2018 Terms of Use: University Photograph Collection, 1947-2012, n.d., Brock University are open for research. Use Restrictions: Copyright is retained by Brock University and others as noted. Copyright in other papers in the collection may be held by their authors, or the authors' heirs or assigns. Researchers must obtain the written permission of the holder(s) of copyright and the University Archives before publishing from materials in the collection. Preferred Citation: UA 17, University Photograph Collection, Brock University, 1947- 2012, Brock University Archives. Acquisition Info.: Fonds were transferred to the Archives in 2008 by retiring University photographer Divino Mucciante. Further transfers were made by Marketing and Communications staff in 2014. Further accruals are expected. Administrative History: Mrs. Grover (Flora) Egerter prepared a resolution to the Allanburg Women’s Institute February 6, 1957 meeting. -

2015 Nobel Prize in Physics
Issue 1, 2016 The magazine of Queen’s University Kingston, Ontario queensu.ca/alumnireview Queen’ALu Mn IrevIsew The biggest, deepest questions Physicists of Queen’s Life after physics Dr. Arthur McDonald AND THE 2015 Nobel Prize in Physics THE NEUTRINO BREAKTHROUGH The Smart, Seccure & Simple Opporrtunity TToo Invest In Downtown KKingston’s Premier Condominium 5DUHRSSRUWXQLW\ ¿UVW RI LWV NLQG LQ .LQJVWRQ ,QYHVW ZLWK H[FHOOHQW HDUQLQJ SRWHQWLDO • )DEXORXVVXLWHV ZLWK ZDWHUUIIURQW YLHZV H[FHOOHQW DPHQLWLHVXQGHUJURXQG SDUNLQJ DQG SUUHHPLHU ORFDWLRQ • &RQYHQLHQWO\ORFDWHG VWHSV IURP 4XHHQ¶V 8QLYHUUVVLW\ VKRSSLQJDQG WKH ZDWHUUIIURQW 5HVLGHQWV ZLOO KDYH HYHU\WKLQJ WKH\QHHG DW WKHLU ¿QJHUUWWLSV 3URYHQ E\ D ZDON VFRUH +$1'62)),19(670(17 33$$&..$$*( ,1&/8'(' FREE PROPEERTY MANAGEMENT FREE FURNISHING PPACKAGEACKAGE 125,6.RENNTTALALL GUARANTEE 11, 2 and 3 bedroom suites priced from the mmid $200s Call 613-9000-2232 or visit online at the capitolcondos.com IN8DEVELOPMENTS.CA contents Issue w, xvw|, Volume v, Number w Serving the Queen’s community since wx} queensu.ca/alumnireview n Queen’ALu Mn IrevIsew Editor’s notebook o Letters to the editor q From the principal d u o M h a r M r Quid Novi e d N a News from campus x e l a y B o t t o h In memoriam: P 5 1 0 Principal Emeritus 2 B a Ron Watts k a r i a d l e C M d l r e a B mt N o r N mn np e The road to Stockholm B © Cover sTory The biggest, nl The neutrino b]^ men/How to clean deepest questions a neutrino detector breakthrough The questions don’t get any bigger than the Dr. -

BIOGRAPHICAL SKETCH Barbara Anne Croy B Anne Croy Professor and Tier 1 Canada Research Chair in Reproduction, Development and Se
Principal Investigator/Program Director (Last, First, Middle): BIOGRAPHICAL SKETCH Provide the following information for the key personnel and other significant contributors in the order listed on Form Page 2. Follow this format for each person. DO NOT EXCEED FOUR PAGES. NAME POSITION TITLE Barbara Anne Croy Professor and Tier 1 Canada Research Chair in eRA COMMONS USER NAME Reproduction, Development and Sexual Function B_Anne_Croy EDUCATION/TRAINING (Begin with baccalaureate or other initial professional education, such as nursing, and include postdoctoral training.) DEGREE INSTITUTION AND LOCATION YEAR(s) FIELD OF STUDY (if applicable) University of Guelph, Guelph, Ontario Canada DVM 1964-1969 Veterinary Medicine University of Toronto, Institute of Medical PhD 1970-1974 Immunology Sciences Brock University, St. Catharines, Ontario PDF- 1980-1985 Developmental Biology parttime A. Positions and Honors. Positions and Employment 1970-1974 MRC (Canada) Fellow, University of Toronto, Toronto, ON 1975-1997 Partner, Animal Health Services, St. Catharines, ON (private veterinary practice) 1981-1982 Lalor Foundation Research Fellow, Biological Sciences, Brock University, St. Catharines, ON 1985-1990 Associate Professor, Biomedical Sciences, University of Guelph, Guelph, ON 1991-2004 Professor, Biomedical Sciences, University of Guelph, Guelph, ON 1991-2007 Adjunct Prof, Dept of Molecular Immunology, Roswell Park Cancer Institute, Buffalo, NY 2003-present Adjunct Professor, Dept of Obstetrics & Gynecology, McMaster University, Hamilton, ON 2004–present Adjunct Professor, Department of Obstetrics & Gynecology, Queen’s University 2005-present Adjunct Professor, Department of Microbiology & Immunology, Queen’s University 2004-2009 Adjunct Professor, Department of Biomedical Sciences, U. Guelph, Guelph, ON 2004-2010 Adjunct Professor, Dept of Human Biology and Nutritional Sciences, U.