Airway-Clearance Therapy Guidelines and Implementation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dymedso Frequencer V2xtm Powered Percussor2 K063645
Dymedso Frequencer v2xTM Powered Percussor2 1.510(k) Summary This summary of safety and effectiveness is being submitted in accordance AUG 3 1 2010 with the requirements of SMVDA 1990 and 21 CFR Part 807.92. Date of Submission: August 31, 2010 Submitter: DYMEDSO, Inc. Address: 901A, Boul. Du Cur4 Boivin Boisbriand, Qu6bec J7G 2S8 CANADA Establishment Registration #: 3004365906 Contact: Yvon Robert, President Phone: (450) 437-9601 Fax: (450) 437-2063 Proprietary Device Name: Frequencer TM v2x Common Name of Device: Airway Clearance Device Classification Name: Percussor, Powered-Electric Device Class: 2 Product Code: BYI Predicate Device: K063645 - Frequencer TM 1001 Description: The Frequencer TM v2x provides airway clearance therapy and promotes bronchial drainage by inducing vibration in the chest walls. It induces oscillatory sound waves in the chest by means of an electro-acoustical transducer (hereafter referred to as the "Power Head") which is placed externally on the patient's chest. The Power Head is connected to a frequency generator which is capable of producing frequencies between 20 and 65 Hz. The Power Head induces sound waves in the patient's chest which are effective in loosening mucus deposits. This model is intended for use in hospital and clinic settings only and disposable filters are available for multi-patient use. Indications for Use: The Frequencer TM v2x provides airway clearance therapy and promotes bronchial drainage by inducing vibration in the chest walls. This device is intended to be a component of chest physiotherapy by providing a convenient method of external thorax manipulation. 7 Dymedso Frequencer V2XTM Powered Percussor It is indicated for patients having respiratory ailments which involve defective mucociliary clearance, as is typical in patients suffering from cystic fibrosis as well as chronic bronchitis, bronchiectasis, ciliary dlyskinesia syndromes, asthma, muscular dystrophy, neuromuscular degenerative disorders, post- operative atelectasis and thoracic wall defects. -

Airway Clearance Devices
UnitedHealthcare® Value & Balance Exchange Medical Policy Airway Clearance Devices Policy Number: IEXT0700.04 Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Policy Applicable States ........................................................................... 1 • Durable Medical Equipment, Orthotics, Medical Coverage Rationale ....................................................................... 1 Supplies and Repairs/Replacements Definitions ...................................................................................... 2 Applicable Codes .......................................................................... 2 Description of Services ................................................................. 4 Benefit Considerations .................................................................. 4 Clinical Evidence ........................................................................... 4 U.S. Food and Drug Administration ............................................ 5 References ..................................................................................... 5 Policy History/Revision Information ............................................. 5 Instructions for Use ....................................................................... 5 Applicable States This Medical Policy only applies to the states of Arizona, Maryland, North Carolina, Oklahoma, Tennessee, Virginia, and Washington. Coverage Rationale See Benefit Considerations A two-month rental trial of a high-frequency chest wall oscillation -
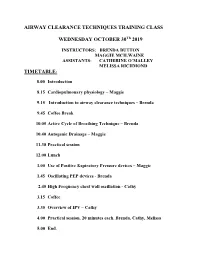
Introduction to Airway Clearance Techniques – Brenda
AIRWAY CLEARANCE TECHNIQUES TRAINING CLASS WEDNESDAY OCTOBER 30Th 2019 INSTRUCTORS: BRENDA BUTTON MAGGIE MCILWAINE ASSISTANTS: CATHERINE O’MALLEY MELISSA RICHMOND TIMETABLE: 8.00 Introduction 8.15 Cardiopulmonary physiology – Maggie 9.15 Introduction to airway clearance techniques – Brenda 9.45 Coffee Break 10.05 Active Cycle of Breathing Technique – Brenda 10.40 Autogenic Drainage – Maggie 11.30 Practical session 12.00 Lunch 1.00 Use of Positive Expiratory Pressure devices – Maggie 1.45 Oscillating PEP devices - Brenda 2.45 High Frequency chest wall oscillation - Cathy 3.15 Coffee 3.35 Overview of IPV – Cathy 4.00 Practical session. 20 minutes each. Brenda, Cathy, Melissa 5.00 End. 8/1/2019 Airway Clearance Techniques Training class Dr Maggie McIlwaine and Dr Brenda Button Catherine O’Malley Melissa Richmond Objectives • Explain the physiology, and theory behind airway clearance techniques currently used in the treatment of cystic fibrosis. • Demonstrate the airway clearance techniques of Active cycle of breathing techniques, autogenic drainage, PEP, oscillating PEP, HFCWO and IPV. • Compose the scientific evidence supporting the use of each of these techniques. Timetable • 8.00 Introduction: Maggie • 8.15 Cardiopulmonary physiology – Maggie • 9.15 Introduction to airway clearance and breathing techniques – Brenda • 9.45 Coffee break • 10.05 The Active Cycle of Breathing Techniques - Brenda • 10.40 Autogenic Drainage Maggie • 11.30 Practical session • 12.00 Lunch M. McIlwaine 1 8/1/2019 Timetable • 1.00 Use of Positive Expiratory Pressure Devices – Maggie • 1.45 Oscillating PEP Devices – Brenda • 2.45 C High Frequency Chest wall Oscillation (HFCWO) therapy-Coffee • 3.15 Coffee • 3.35 Overview of IPV – Cathy • 4.00 Practical session. -
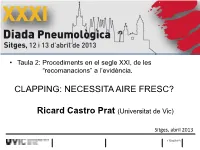
Clapping: Necessita Aire Fresc?
XXXI Diada Peumològica • Taula 2: Procediments en el segle XXI, de les “recomanacions” a l’evidència. CLAPPING: NECESSITA AIRE FRESC? Ricard Castro Prat (Universitat de Vic) Sitges, abril 2013 17/04/2013 CLAPPING: NECESSITA AIRE FRESC? “The evidence for passive techniques such as postural drainage and percussion is low.” 17/04/2013 2 CLAPPING: NECESSITA AIRE FRESC? “… routine use […] is not indicated in the treatment of stable outpatients with COPD and moderate amounts of sputm production.” “It seems […] alone is insufficient to evacuate excess mucus.” “Therapists should consider active mucus evacuation techniques instead.” 17/04/2013 3 CLAPPING: NECESSITA AIRE FRESC? “Studies that provide solid evidence of the effectiveness of different airway clearance techniques in patients with COPD are rather scarce” 17/04/2013 4 CLAPPING: NECESSITA AIRE FRESC? 17/04/2013 5 CLAPPING: NECESSITA AIRE FRESC? 17/04/2013 6 CLAPPING: NECESSITA AIRE FRESC? Les percussions thoraciques manuelles (PTM) “Les vibrations appliquées au thorax, et les percussions communément nommées clapping occupent une place anecdotique. Ces techniques ne font pas l'unanimité ....” “Les PTM n'ont fait l'objet d'aucun travail de validation en utilisation isolée alors qu'elles sont largement utilisées et diffusées dans les pays anglo-saxons où elles sont associées avec d'autres techniques sous le vocable de chest physiotherapy, dans la rubrique de la physiothérapie conventionnelle. “… elles ont toutefois des contre-indications locales et générales àrespecter . “ “Si action il y a, les PTM seraient plus efficaces chez les patients ayant des sécrétions volumineuses, proximales.” “Elles semblent également utiles comme moyen de stimuler la toux.“ “…ne peuvent être envisagées comme seul moyen de drainage bronchique. -

AARC Clinical Practice Guideline: Effectiveness of Nonpharmacologic Airway Clearance Therapies in Hospitalized Patients
AARC Clinical Practice Guideline: Effectiveness of Nonpharmacologic Airway Clearance Therapies in Hospitalized Patients Shawna L Strickland PhD RRT-NPS AE-C FAARC, Bruce K Rubin MD MEngr MBA FAARC, Gail S Drescher MA RRT, Carl F Haas MLS RRT FAARC, Catherine A O’Malley RRT-NPS, Teresa A Volsko MHHS RRT FAARC, Richard D Branson MSc RRT FAARC, and Dean R Hess PhD RRT FAARC Airway clearance therapy (ACT) is used in a variety of settings for a variety of ailments. These guidelines were developed from a systematic review with the purpose of determining whether the use of nonpharmacologic ACT improves oxygenation, reduces length of time on the ventilator, reduces stay in the ICU, resolves atelectasis/consolidation, and/or improves respiratory mechanics, versus usual care in 3 populations. For hospitalized, adult and pediatric patients without cystic fibrosis, 1) chest physiotherapy (CPT) is not recommended for the routine treatment of uncompli- cated pneumonia; 2) ACT is not recommended for routine use in patients with COPD; 3) ACT may be considered in patients with COPD with symptomatic secretion retention, guided by patient preference, toleration, and effectiveness of therapy; 4) ACT is not recommended if the patient is able to mobilize secretions with cough, but instruction in effective cough technique may be useful. For adult and pediatric patients with neuromuscular disease, respiratory muscle weakness, or impaired cough, 1) cough assist techniques should be used in patients with neuromuscular disease, particularly when peak cough flow is < 270 L/min; CPT, positive expiratory pressure, intrapul- monary percussive ventilation, and high-frequency chest wall compression cannot be recommended, due to insufficient evidence. -

Is It More Than Copd? 2
INTERNATIONAL BIOPHYSICS CORPORATION Over a quarter of a century legacy of unwavering commitment to creating innovative and disruptive medical devices and technologies that improve treatment therapies and patient outcomes. For more information, please visit afflovest.com REFERENCES 1. Volsko, T. Airway Clearance Therapy: Finding the Evidence. Respiratory Care. 2013; 58(10):1669-78. IS IT MORE THAN COPD? 2. Papaiwannou, A. et al. Asthma-Chronic Obstructive Pulmonary Disease Overlap Syndrome (ACOS): Current Literature Review. J Thorac Dis. 2014; 6(S1):S146-S151 3 Aksamit, T. et al. Bronchiectasis and Chronic Airway Disease: It Is Not Just About Asthma and COPD. CHEST. 2018; 154(4):737-739. 4. Ramos, F. et al. Clinical Issues of Mucus Accumulation in COPD. Int J Chron Obstruct Pulmon Dis. 2014; 9:139-150. 5. Kosmos, E. et al. Bronchiectasis in Patients with COPD: An Irrelevant Imaging Finding or a Clinically Important Phenotype? CHEST. 2016; 150(4):894A. LEARN HOW AIRWAY CLEARANCE 6. Weycker, D. et al. Prevalence and Incidence of Non-cystic Fibrosis BE Among US Adults in 2013. Chron Respir Dis 2017; 14(4):377-384. THERAPY IS A PREVENTATIVE 7. Gagnon, P. et al. Pathogenesis of Hyperinflation in Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2014; 9:187-201. TREATMENT OPTION THAT CAN HELP 8. McCool, F. et al. Dysfunction of the Diaphragm. N Engl J Med. 2012; 366(10):932-942. AT-RISK PULMONARY PATIENTS International Biophysics Corporation | 2101 E. St. Elmo Rd. Ste 275 | Austin, TX 78744 (T) 888-711-1145 | (F) 888-793-2319 | [email protected] | © Copyright 2020. -
The Vest® Airway Clearance System Clinical Dossier
THE VEST ® AIRWAY CLEARANCE SYSTEM Clinical Dossier To Support Medical Policy Review for Expanded Coverage of Neuromuscular Diseases September 2019 The Vest® Airway Clearance System Clinical Dossier Table of Contents EXECUTIVE SUMMARY 3 Clinical benefits 3 1.1 Spinal Muscular Atrophy 3 1.2 Cerebral Palsy 4 1.3 Amyotrophic Lateral Sclerosis 4 1.4 Muscular Dystrophy 4 Economic benefits 5 Conclusion 9 Product description 11 2.1 The Vest® Airway Clearance System 11 2.2 The Monarch® Airway Clearance System 11 Disease description 13 3.1 Introduction 13 3.2 Airway clearance and lung defense mechanism 13 3.3 Respiratory complications in NMD 13 3.4 Clinical and economic implications of respiratory complications and airway clearance therapy in NMD patients 14 Study summaries 15 LIST OF REVIEW ARTICLES 20 REFERENCES 21 2 The Vest® Airway Clearance System Clinical Dossier Executive Summary CLINICAL BENEFITS The safety and efficacy of High Frequency Chest Wall Oscillation (HFCWO) as an airway clearance modality has been demonstrated in numerous studies in patients with neuromuscular diseases including spinal muscular atrophy, amyotrophic lateral sclerosis (ALS), cerebral palsy (CP), multiple sclerosis (MS) and spinal cord injuries. A trend towards fewer hospitalizations, reduced incidence of pneumonia and reduced intravenous antibiotic use for respiratory infections have been shown. A 2010 randomized controlled trial by Yuan et al. compared clinical outcomes, including duration of acute infections, adverse events, polysomnogram results, chest radiograph findings, and body mass index in a group of Neuromuscular Disease (NMD) and CP patients who were treated with standard chest physiotherapy and another group who received HFCWO over five months. -

“Clean Nebulizer & Airway Clearance Equipment
Physiotherapy Advisory Group Cleaning Nebulizer and Airway Clearance Equipment at Home To prevent infections caused by contaminated equipment used in the home, it should be cleaned and disinfected regularly. Equipment must be cleaned thoroughly to remove all debris before disinfecting. After cleaning with mild soap and water, disinfect either by immersion in cold disinfectants or by heat, if permissible by the manufacturer. Proper hand hygiene is required prior to all equipment handling. Please follow your CF team recommendations for proper hand washing technique. Review Infection Control plan with your Physiotherapist. _________________________________________________________________________________ “Clean Nebulizer & Airway Clearance Equipment After Each Use” Take the device apart. Wash the pieces in mild dish soap and water. Rinse all the pieces in sterile water* Place the pieces on a clean dry towel and air dry. Store the device in a sealed plastic bag. _________________________________________________________________________________ “Sterilize Nebulizer & Airway Clearance Equipment As Soon As Possible After Each Use” Take the device apart. Wash all the pieces in mild soap and water. Choose heat or cold sterilizing by one of the following methods: Heat sterilizing (if allowed by equipment manufacturer) • Boil for at least 10 minutes OR • Microwave (2.45GHz) for 5 minutes OR • Dishwasher, if temperature is >70°C > 158F, for 30 minutes OR • Electric steam sterilizer OR Cold sterilizing • Soak in 70% isopropyl alcohol for 5 minutes OR Soak in 3% Hydrogen peroxide for 30 minutes OR • Then rinse all the pieces in sterile water* After sterilizing equipment, place the pieces on a clean dry towel to air-dry, then store the device in a sealed plastic bag. -

Airway Clearance: Why, When and How
Airway Clearance: Why, When and How NOTE: PLEASE CONSULT YOUR PHYSICIAN BEFORE TRYING ANY OF THESE TECHNIQUES. NOTE: IF YOU HAVE RECENTLY OR ARE CURRENTLY COUGHING UP ANY BLOOD, DO NOT USE ANY AIRWAY CLEARANCE TECHNIQUES UNLESS DIRECTED TO DO SO BY YOUR DOCTOR. Why? What is Airway Clearance? It is clearance of mucus or sputum from the lungs and/or airways. Respiratory tracts continuously produce mucus that is a part of our immune system. Inhaled particles, including bacteria, get trapped in this mucus and are normally swept up by the beating action of little hairs called cilia. Once pushed though the air sacs, small and large airways, a cough completes the process of expelling mucus and it is this combination that is called airway clearance. The Importance of Airway Clearance Coughing makes breathing easier, opens airways, and rids lungs of infected material. It also gives antibiotics more room to work. If we don’t cough and clear our airways breathing can become more difficult and the normal exchange of oxygen and carbon dioxide may be compromised. You may feel some shortness of breath if the airways and lungs are not cleared of excess mucus. Also, bacteria may be trapped in the lungs with the potential for causing respiratory tract infections. Repeated episodes of infection may result in lung damage. Effective airway clearance, (also referred to as pulmonary or respiratory hygiene or therapy) is often an important part of the overall treatment plan for patients with NTM and especially for those with bronchiectasis. Whether you have a productive cough that produces thick or excessive sputum, or a dry unproductive cough that does not produce sputum, airway clearance techniques can help keep airways clear and open by inflating the airways and helping to prevent mucus from plugging the small airways. -

Measuring Airway Clearance Outcomes in Bronchiectasis: a Review
REVIEW BRONCHIECTASIS Measuring airway clearance outcomes in bronchiectasis: a review Lisa J. Franks1,2, James R. Walsh1,2,3, Kathleen Hall1,4 and Norman R. Morris2,3,5 Affiliations: 1Physiotherapy Dept, The Prince Charles Hospital, Chermside, Australia. 2School of Allied Health Sciences and Menzies Health Institute, Griffith University, Brisbane, Australia. 3Heart Lung Institute, The Prince Charles Hospital, Chermside, Australia. 4Physiotherapy, School of Allied Health, Australian Catholic University, Brisbane, Australia. 5Allied Health Research Collaborative, Metro North Hospital and Health Service, The Prince Charles Hospital, Chermside, Australia. Correspondence: Lisa J. Franks, Physiotherapy Dept, The Prince Charles Hospital, Rode Road, Chermside, Queensland 4032, Australia. E-mail: [email protected] @ERSpublications For airway clearance research in bronchiectasis, sputum volume, lung function, dyspnoea and health- related and cough-related quality of life are currently the most common clinical and patient-reported measures of airway clearance treatment efficacy. https://bit.ly/2KXRdg8 Cite this article as: Franks LJ, Walsh JR, Hall K, et al. Measuring airway clearance outcomes in bronchiectasis: a review Eur Respir Rev 2020; 29: 190161 [https://doi.org/10.1183/16000617.0161-2019]. ABSTRACT While airway clearance techniques (ACTs) are recommended for individuals with bronchiectasis, many trials have demonstrated inconsistent benefits or failed to reach their primary outcome. This review determined the most common clinical and patient-reported outcome measures used to evaluate the efficacy of ACTs in bronchiectasis. A literature search of five databases using relevant keywords and filtering for studies published in English, up until the end of August 2019, was completed. Studies included randomised controlled trials, using crossover or any other trial design, and abstracts. -

Airway Clearance Devices – Oxford Clinical Policy
UnitedHealthcare® Oxford Clinical Policy Airway Clearance Devices Policy Number: DME 019.31 T2 Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Policy Coverage Rationale ....................................................................... 1 • Durable Medical Equipment, Orthotics, Ostomy Documentation Requirements ...................................................... 1 Supplies, Medical Supplies and Repairs/ Prior Authorization Requirements ................................................ 2 Replacement Definitions ...................................................................................... 2 Applicable Codes .......................................................................... 3 Description of Services ................................................................. 4 Benefit Considerations .................................................................. 5 Clinical Evidence ........................................................................... 5 U.S. Food and Drug Administration ............................................. 5 References ..................................................................................... 6 Policy History/Revision Information ............................................. 6 Instructions for Use ....................................................................... 6 Coverage Rationale See Benefit Considerations A two-month rental trial of a high-frequency chest wall oscillation system is proven and medically necessary in the management of bronchiectasis, -

Airway Clearance Therapy: Finding the Evidence
Airway Clearance Therapy: Finding the Evidence Teresa A Volsko MHHS RRT FAARC Introduction Airway Clearance Therapy: What Is It and Why Is It Needed? Impairment of Secretion Clearance and Pulmonary Disease Neurorespiratory Dysfunction and Secretion Clearance Problems Indications for Airway Clearance Where to Look for Current Evidence Studies Synthesis Systematic Reviews Evidenced-Based Clinical Practice Guidelines Putting Evidence Into Practice Summary Disease processes can impair ciliary function, alter secretion production and mucus rheology, and interfere with the cough reflex. Airway clearance therapy has been a cornerstone of therapy aimed at minimizing the devastating effects of airway obstruction, infection, and inflammation due to mucus stasis on the conducting airways and lung parenchyma. Although challenges to performing clinical studies evaluating the effectiveness of airway clearance therapeutic modalities exist, re- sources are available in the literature. In addition to device evaluations and original clinical re- search, the expert opinion, systematic reviews, and evidence-based practice guidelines can be found. These tools can be used to develop protocols and pathways to guide our practice. Monitoring and reporting patient, process, and financial outcomes are essential steps germane to the implementa- tion of evidence-based care. Key words: airway clearance devices; cough; mucociliary transport; postural drainage; active cycle of breathing; positive expiratory pressure; oscillatory positive expiratory pressure; HFCWO;