IPG CF Blue Booklet 7Th Edition 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bronchopulmonary Hygiene Protocol
BRONCHOPULMONARY HYGIENE PROTOCOL MD order for Bronchopulmonary Hygiene Protocol Evaluate Indications: 9 Difficulty with secretion clearence with sputum production > 25 ml/day 9 Evidence of retained secretions 9 Mucus plug induced atelectasis 9 Foreign body in airway 9 Diagnosis of cystic fibrosis, bronchiectasis, or cavitating lung disease Yes Does contraindication or potential hazard exist? No Address any immediate need and contact MD/RN Select method based on: 9 Patient preference/comfort/pain avoidance 9 Observation of effectiveness with trial 9 History with documented effectiveness Method may include: 9 Manual chest percussion and positioning 9 External chest wall vibration 9 Intrapulmonary percussion Adminster therapy no less than QID and PRN, supplemented by suctioning for all patients with artificial airways Re-evaluate pt every 24 hours, and 24 hours after discontinued Assess Outcomes: Goals achieved? 9 Optimal hydration with sputum production < 25 ml/day 9 Breath sounds from diminished to adventitious with ronchi cleared by cough 9 Patient subjective impression of less retention and improved clearance 9 Resolution/Improvement in chest X-ray 9 Improvement in vital signs and measures of gas exchange 9 If on ventilator, reduced resistance and improved compliance Care Plan Considerations: Discontinue therapy if improvement is observed and sustained over a 24-hour period. Patients with chronic pulmonary disease who maintain secretion clearance in their home environment should remain on treatment no less than their home frequency. Hyperinflation Protocol should be considered for patients who are at high risk for pulmonary complications as listed in the indications for Hyperinflation Protocol. 5/5/03 (Jan Phillips-Clar, Rick Ford, Judy Tietsort, Jay Peters, David Vines) AARC References for Bronchopulmonary Algorithm 1. -

Respiratory Syncytial Virus Bronchiolitis in Children DUSTIN K
Respiratory Syncytial Virus Bronchiolitis in Children DUSTIN K. SMITH, DO; SAJEEWANE SEALES, MD, MPH; and CAROL BUDZIK, MD Naval Hospital Jacksonville, Jacksonville, Florida Bronchiolitis is a common lower respiratory tract infection in infants and young children, and respiratory syncytial virus (RSV) is the most common cause of this infection. RSV is transmitted through contact with respiratory droplets either directly from an infected person or self-inoculation by contaminated secretions on surfaces. Patients with RSV bronchiolitis usually present with two to four days of upper respiratory tract symptoms such as fever, rhinorrhea, and congestion, followed by lower respiratory tract symptoms such as increasing cough, wheezing, and increased respira- tory effort. In 2014, the American Academy of Pediatrics updated its clinical practice guideline for diagnosis and man- agement of RSV bronchiolitis to minimize unnecessary diagnostic testing and interventions. Bronchiolitis remains a clinical diagnosis, and diagnostic testing is not routinely recommended. Treatment of RSV infection is mainly sup- portive, and modalities such as bronchodilators, epinephrine, corticosteroids, hypertonic saline, and antibiotics are generally not useful. Evidence supports using supplemental oxygen to maintain adequate oxygen saturation; however, continuous pulse oximetry is no longer required. The other mainstay of therapy is intravenous or nasogastric admin- istration of fluids for infants who cannot maintain their hydration status with oral fluid intake. Educating parents on reducing the risk of infection is one of the most important things a physician can do to help prevent RSV infection, especially early in life. Children at risk of severe lower respiratory tract infection should receive immunoprophy- laxis with palivizumab, a humanized monoclonal antibody, in up to five monthly doses. -

Chest Physiotherapy Page 1 of 10
UTMB RESPIRATORY CARE SERVICES Policy 7.3.9 PROCEDURE - Chest Physiotherapy Page 1 of 10 Chest Physiotherapy Effective: 10/12/94 Revised: 04/05/18 Formulated: 11/78 Chest Physiotherapy Purpose To standardize the use of chest physiotherapy as a form of therapy using one or more techniques to optimize the effects of gravity and external manipulation of the thorax by postural drainage, percussion, vibration and cough. A mechanical percussor may also be used to transmit vibrations to lung tissues. Policy Respiratory Care Services provides skilled practitioners to administer chest physiotherapy to the patient according to physician’s orders. Accountability/Training • Chest Physiotherapy is administered by a Licensed Respiratory Care Practitioner trained in the procedure(s). • Training must be equivalent to the minimal entry level in the Respiratory Care Service with the understanding of age specific requirements of the patient population treated. Physician's A written order by a physician is required specifying: Order Frequency of therapy. Lung, lobes and segments to be drained. Any physical or physiological difficulties in positioning patient. Cough stimulation as necessary. Type of supplemental oxygen, and/or adjunct therapy to be used. Indications This therapy is indicated as an adjunct in any patient whose cough alone (voluntary or induced) cannot provide adequate lung clearance or the mucociliary escalator malfunctions. This is particularly true of patients with voluminous secretions, thick tenacious secretions, and patients with neuro- muscular disorders. Drainage positions should be specific for involved segments unless contraindicated or if modification is necessary. Drainage usually in conjunction with breathing exercises, techniques of percussion, vibration and/or suctioning must have physician's order. -
A Physiotherapy Approach to the Control of Asthma Symptoms and Anxiety
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Biblioteca Digital da Produção Intelectual da Universidade de São Paulo (BDPI/USP) Universidade de São Paulo Biblioteca Digital da Produção Intelectual - BDPI Sem comunidade WoS 2012 Respiratory rehabilitation: a physiotherapy approach to the control of asthma symptoms and anxiety CLINICS, SAO PAULO, v. 67, n. 11, supl. 1, Part 1, pp. 1291-1297, FEB, 2012 http://www.producao.usp.br/handle/BDPI/34492 Downloaded from: Biblioteca Digital da Produção Intelectual - BDPI, Universidade de São Paulo CLINICS 2012;67(11):1291-1297 DOI:10.6061/clinics/2012(11)12 CLINICAL SCIENCE Respiratory rehabilitation: a physiotherapy approach to the control of asthma symptoms and anxiety Renata Andre´ Laurino (in memoriam),I Viviane Barnabe´,I Beatriz M. Saraiva-Romanholo,I Rafael Stelmach,II Alberto Cukier,II Maria do Patrocı´nio T. NunesI I Faculdade de Medicina da Universidade de Sa˜ o Paulo, Department of Medicine, Sa˜ o Paulo/SP, Brazil. II Pulmonary Division, Heart Institute (InCor), Hospital das Clı´nicas da Universidade de Sa˜ o Paulo, Sa˜ o Paulo/SP, Brazil. OBJECTIVES: The objectives of this study were to verify the degree of anxiety, respiratory distress, and health-related quality of life in a group of asthmatic patients who have experienced previous panic attacks. Additionally, we evaluated if a respiratory physiotherapy program (breathing retraining) improved both asthma and panic disorder symptoms, resulting in an improvement in the health-related quality of life of asthmatics. METHODS: Asthmatic individuals were assigned to a chest physiotherapy group that included a breathing retraining program held once a week for three months or a paired control group that included a Subtle Touch program. -

Dymedso Frequencer V2xtm Powered Percussor2 K063645
Dymedso Frequencer v2xTM Powered Percussor2 1.510(k) Summary This summary of safety and effectiveness is being submitted in accordance AUG 3 1 2010 with the requirements of SMVDA 1990 and 21 CFR Part 807.92. Date of Submission: August 31, 2010 Submitter: DYMEDSO, Inc. Address: 901A, Boul. Du Cur4 Boivin Boisbriand, Qu6bec J7G 2S8 CANADA Establishment Registration #: 3004365906 Contact: Yvon Robert, President Phone: (450) 437-9601 Fax: (450) 437-2063 Proprietary Device Name: Frequencer TM v2x Common Name of Device: Airway Clearance Device Classification Name: Percussor, Powered-Electric Device Class: 2 Product Code: BYI Predicate Device: K063645 - Frequencer TM 1001 Description: The Frequencer TM v2x provides airway clearance therapy and promotes bronchial drainage by inducing vibration in the chest walls. It induces oscillatory sound waves in the chest by means of an electro-acoustical transducer (hereafter referred to as the "Power Head") which is placed externally on the patient's chest. The Power Head is connected to a frequency generator which is capable of producing frequencies between 20 and 65 Hz. The Power Head induces sound waves in the patient's chest which are effective in loosening mucus deposits. This model is intended for use in hospital and clinic settings only and disposable filters are available for multi-patient use. Indications for Use: The Frequencer TM v2x provides airway clearance therapy and promotes bronchial drainage by inducing vibration in the chest walls. This device is intended to be a component of chest physiotherapy by providing a convenient method of external thorax manipulation. 7 Dymedso Frequencer V2XTM Powered Percussor It is indicated for patients having respiratory ailments which involve defective mucociliary clearance, as is typical in patients suffering from cystic fibrosis as well as chronic bronchitis, bronchiectasis, ciliary dlyskinesia syndromes, asthma, muscular dystrophy, neuromuscular degenerative disorders, post- operative atelectasis and thoracic wall defects. -

Evaluation of an Alternative Chest Physiotherapy Method in Infants with Respiratory Syncytial Virus Bronchiolitis
Evaluation of an Alternative Chest Physiotherapy Method in Infants With Respiratory Syncytial Virus Bronchiolitis Guy Postiaux PT, Jacques Louis MD, Henri C Labasse MD, Julien Gerroldt PT, Anne-Claire Kotik PT, Amandine Lemuhot PT, and Caroline Patte PT BACKGROUND: We proposed a new chest physiotherapy (CPT) secretion clearance method to treat respiratory syncytial virus bronchiolitis in infants. Our new CPT method consists of 15 pro- longed slow expirations, then 5 provoked cough maneuvers. METHODS: We randomized 20 infants (mean age 4.2 months) into 2 groups: 8 patients received 27 sessions of nebulization of hypertonic saline; 12 patients received 31 sessions of nebulization of hypertonic saline followed by our new CPT method. We used the Wang clinical severity scoring system (which assesses wheezing, respiratory rate, retractions, and general condition) and measured S and heart rate before each CPT session pO2 (T0), immediately after the 30-min session (T30), and 120 min after the session (T150). RESULTS: Within the groups: in the first group, Wang score was significantly lower at T150 than at T0: 4.6 vs In the new-method-CPT group, Wang score was significantly lower at T30 (3.6 vs .(008. ؍ P) 5.0 Wheezing score was significantly lower at T150 .(002. ؍ and at T150 (3.7 vs 4.3, P (001. ؍ P ,4.3 in the first group, and in the new-method-CPT group at T30 than (02. ؍ than at T0 (1.1 vs 1.2, P Between the groups: at .(001. ؍ and at T150 than at T0 (0.9 vs 1.3, P (001. ؍ at T0 (0.8 vs 1.3, P T30 the improvement was significantly better in the new-method-CPT group for overall Wang score and heart rate (P < .001). -

Chest Physiotherapy in Cystic Fibrosis: Improved Tolerance with Nasal Pressure Support Ventilation
Chest Physiotherapy in Cystic Fibrosis: Improved Tolerance With Nasal Pressure Support Ventilation Brigitte Fauroux, MD*; Miche`le Boule´, MD, PhD‡; Fre´de´ric Lofaso, MD, PhD§; Franc¸oise Ze´rah, MD§; Annick Cle´ment, MD, PhD*; Alain Harf, MD, PhD§; and Daniel Isabey, PhD§ ABSTRACT. Objective. Chest physiotherapy (CPT) is pared with the control session. SpO2 decreases after FET an integral part of the treatment of patients with cystic were significantly larger during the control session (na- fibrosis (CF). CPT imposes additional respiratory work dir: 91.8 6 0.7%) than during the PSV session (93.8 6 that may carry a risk of respiratory muscle fatigue. In- 0.6%). Maximal pressures decreased during the control 6 6 spiratory pressure support ventilation (PSV) is a new session (from 71.9 6.1 to 60.9 5.3 cmH2O, and from 6 6 mode of ventilatory assistance designed to maintain a 85.3 7.9 to 77.5 4.8 cmH2O, for PImax and PEmax, constant preset positive airway pressure during sponta- respectively) and increased during the PSV session (from 6 6 6 neous inspiration with the goal of decreasing the pa- 71.6 8.6 to 83.9 8.7 cmH2O, and from 80.4 7.8 to 88.0 6 tient’s inspiratory work. The aim of our study was 1) to 7.4 cmH2O, for PImax and PEmax, respectively). The evaluate respiratory muscle fatigue and oxygen desatu- decrease in PEmax was significantly correlated with the ration during CPT and 2) to determine whether noninva- severity of bronchial obstruction as evaluated based on sive PSV can relieve these potential adverse effects of baseline FEV1 (% predicted). -

Randomized Controlled Trial a Fisioterapia Respiratória É Eficaz Na Redução De Escore Clínico Na Bronquiolite: Ensaio Controlado Randomizado
ISSN 1413-3555 Rev Bras Fisioter, São Carlos, v. 16, n. 3, p. 241-7, May/June 2012 ORIGINAL ARTICLE ©Revista Brasileira de Fisioterapia Chest physical therapy is effective in reducing the clinical score in bronchiolitis: randomized controlled trial A fisioterapia respiratória é eficaz na redução de escore clínico na bronquiolite: ensaio controlado randomizado Évelim L. F. D. Gomes1, Guy Postiaux2, Denise R. L. Medeiros3, Kadma K. D. S. Monteiro4, Luciana M. M. Sampaio5, Dirceu Costa5 Abstract Objective: To evaluate the effectiveness of chest physical therapy (CP) in reducing the clinical score in infants with acute viral bronchiolitis (AVB). Methods: Randomized controlled trial of 30 previously healthy infants (mean age 4.08 SD 3.0 months) with AVB and positive for respiratory syncytial virus (RSV), evaluated at three moments: at admission, then at 48 and 72 hours after admission. The procedures were conducted by blinded assessors to each of three groups: G1 - new Chest Physical therapy- nCPT (Prolonged slow expiration - PSE and Clearance rhinopharyngeal retrograde - CRR), G2 - conventional Chest Physical therapy- cCPT (modified postural drainage, expiratory compression, vibration and percussion) and G3 - aspiration of the upper airways. The outcomes of interest were the Wang’s clinical score (CS) and its components: Retractions (RE), Respiratory Rate (RR), Wheezing (WH) and General Conditions (GC). Results: The CS on admission was reduced in G1 (7.0-4.0) and G2 (7.5-5.5) but was unchanged in G3 (7.5-7.0). We observed a change 48 hours after hospitalization in G1 (5.5-3.0) and G2 (4.0-2.0) and in 72 hours, there was a change in G1 (2.0-1.0). -

Airway Clearance Devices
UnitedHealthcare® Value & Balance Exchange Medical Policy Airway Clearance Devices Policy Number: IEXT0700.04 Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Related Policy Applicable States ........................................................................... 1 • Durable Medical Equipment, Orthotics, Medical Coverage Rationale ....................................................................... 1 Supplies and Repairs/Replacements Definitions ...................................................................................... 2 Applicable Codes .......................................................................... 2 Description of Services ................................................................. 4 Benefit Considerations .................................................................. 4 Clinical Evidence ........................................................................... 4 U.S. Food and Drug Administration ............................................ 5 References ..................................................................................... 5 Policy History/Revision Information ............................................. 5 Instructions for Use ....................................................................... 5 Applicable States This Medical Policy only applies to the states of Arizona, Maryland, North Carolina, Oklahoma, Tennessee, Virginia, and Washington. Coverage Rationale See Benefit Considerations A two-month rental trial of a high-frequency chest wall oscillation -

Evidence Based Chest Physiotherapy for Cystic Fibrosis
Short Communication ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2019.15.002673 Evidence Based Chest Physiotherapy for Cystic Fibrosis Mohammad Habibur Rahman* Lecturer (Physiotherapy), School of Science and Technology, Bangladesh Open University, Gazipur-1705, Bangladesh *Corresponding author: Mohammad Habibur Rahman, Lecturer (Physiotherapy), School of Science and Technology, Bangladesh Open University, Gazipur-1705, Bangladesh ARTICLE INFO abstract Received: Published: of bronchial sections. In addition to medicine different physiotherapy treatment techniques February 14, 2019 Cystic fibrosis (CF) is a genetically predisposed disease causing difficulties in clearance February 27, 2019 clear bronchial sections and lessen the work of breathing. Absolute indication and dose Citation: Mohammad Habibur Rah- basedfor instance chest physiotherapypostural drainage, is mandatory percussion, and chest evidence shaking, based huffing physiotherapy and coughing practice helps is es to- man. Evidence Based Chest Physio- J Sci & Tech Res 15(2)-2019. BJSTR. sentialAbbreviations: for livelihood of a CF patient. MS.ID.002673.therapy for Cystic Fibrosis. Biomed - CF: Cystic Fibrosis; PEP: Positive Expiratory Pressure; HPEP: High pressure PEP; P&PD: Percussion and Postural Drainage; OPEP: Oscillatory PEP; HFCC: High Frequen cy Chest Compressions; AD: Autogenic Drainage. Introduction Pulmonary diseases regarded as one of the main sources Among the eight crosses over studies, six experiments focused of limitation in daily livelihood. These limitations are highly on single treatment approaches in which four experiments comprising of 28 participants was found a huge amount of of breathlessness and decrease exercise tolerance [1]. Chest expelled secretions after application of chest physiotherapy when influenced by difficulties to clear bronchial secretions, symptoms compared to no treatment option. One experiment was conducted on 18 participants and found similarities of sputum weight when disease like cystic fibrosis (CF) exhibited similar features described compared to control group. -
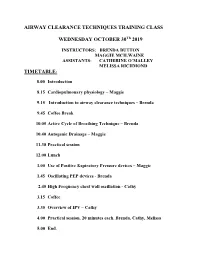
Introduction to Airway Clearance Techniques – Brenda
AIRWAY CLEARANCE TECHNIQUES TRAINING CLASS WEDNESDAY OCTOBER 30Th 2019 INSTRUCTORS: BRENDA BUTTON MAGGIE MCILWAINE ASSISTANTS: CATHERINE O’MALLEY MELISSA RICHMOND TIMETABLE: 8.00 Introduction 8.15 Cardiopulmonary physiology – Maggie 9.15 Introduction to airway clearance techniques – Brenda 9.45 Coffee Break 10.05 Active Cycle of Breathing Technique – Brenda 10.40 Autogenic Drainage – Maggie 11.30 Practical session 12.00 Lunch 1.00 Use of Positive Expiratory Pressure devices – Maggie 1.45 Oscillating PEP devices - Brenda 2.45 High Frequency chest wall oscillation - Cathy 3.15 Coffee 3.35 Overview of IPV – Cathy 4.00 Practical session. 20 minutes each. Brenda, Cathy, Melissa 5.00 End. 8/1/2019 Airway Clearance Techniques Training class Dr Maggie McIlwaine and Dr Brenda Button Catherine O’Malley Melissa Richmond Objectives • Explain the physiology, and theory behind airway clearance techniques currently used in the treatment of cystic fibrosis. • Demonstrate the airway clearance techniques of Active cycle of breathing techniques, autogenic drainage, PEP, oscillating PEP, HFCWO and IPV. • Compose the scientific evidence supporting the use of each of these techniques. Timetable • 8.00 Introduction: Maggie • 8.15 Cardiopulmonary physiology – Maggie • 9.15 Introduction to airway clearance and breathing techniques – Brenda • 9.45 Coffee break • 10.05 The Active Cycle of Breathing Techniques - Brenda • 10.40 Autogenic Drainage Maggie • 11.30 Practical session • 12.00 Lunch M. McIlwaine 1 8/1/2019 Timetable • 1.00 Use of Positive Expiratory Pressure Devices – Maggie • 1.45 Oscillating PEP Devices – Brenda • 2.45 C High Frequency Chest wall Oscillation (HFCWO) therapy-Coffee • 3.15 Coffee • 3.35 Overview of IPV – Cathy • 4.00 Practical session. -
Treating Bronchiectasis
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES Treating Bronchiectasis Bronchiectasis (bron-kee-eck-tuh-sis) is a lung condition that causes cough, sputum production, and recurrent respiratory infections. (Also see “What is Bronchiectasis?” at www.thoracic.org/patients). Because bronchiectasis is a condition that develops over many years and worsens with repeated infections, the main treatment goal is to reduce stagnant secretions (mucus, sputum) in the airways and germs contained in those secretions. Your healthcare provider will help you figure out the ■ chest physiotherapy involves chest clapping in best treatment plan for you. There are two important various positions to move mucus up to the windpipe parts of bronchiectasis treatment: so that you can cough it out. ■ Maintenance: What you do every day. This usually ■ handheld positive expiratory pressure (PEP) devices includes airway clearance, changes in your lifestyle, are used to loosen mucus by creating vibration while and other actions you can take to prevent infections and lung damage. breathing through the device. ■ Exacerbations (eg-zass-er-bay-shuns): What you do ■ percussion devices which can include mechanical when you get sick and have a change in symptoms. percussors and percussive vests (high frequency This usually includes increasing airway clearance and chest wall oscilliation) are used to loosen mucus and CLIP AND COPY AND CLIP taking antibiotics to treat infection. move it to the windpipe to cough out. What are airway clearance techniques? All forms of airway clearance depend on good coughs Depending on how severe your bronchiectasis is and how much mucus is produced in your airways, your to move loose mucus out.