A Physiotherapy Approach to the Control of Asthma Symptoms and Anxiety
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bronchopulmonary Hygiene Protocol
BRONCHOPULMONARY HYGIENE PROTOCOL MD order for Bronchopulmonary Hygiene Protocol Evaluate Indications: 9 Difficulty with secretion clearence with sputum production > 25 ml/day 9 Evidence of retained secretions 9 Mucus plug induced atelectasis 9 Foreign body in airway 9 Diagnosis of cystic fibrosis, bronchiectasis, or cavitating lung disease Yes Does contraindication or potential hazard exist? No Address any immediate need and contact MD/RN Select method based on: 9 Patient preference/comfort/pain avoidance 9 Observation of effectiveness with trial 9 History with documented effectiveness Method may include: 9 Manual chest percussion and positioning 9 External chest wall vibration 9 Intrapulmonary percussion Adminster therapy no less than QID and PRN, supplemented by suctioning for all patients with artificial airways Re-evaluate pt every 24 hours, and 24 hours after discontinued Assess Outcomes: Goals achieved? 9 Optimal hydration with sputum production < 25 ml/day 9 Breath sounds from diminished to adventitious with ronchi cleared by cough 9 Patient subjective impression of less retention and improved clearance 9 Resolution/Improvement in chest X-ray 9 Improvement in vital signs and measures of gas exchange 9 If on ventilator, reduced resistance and improved compliance Care Plan Considerations: Discontinue therapy if improvement is observed and sustained over a 24-hour period. Patients with chronic pulmonary disease who maintain secretion clearance in their home environment should remain on treatment no less than their home frequency. Hyperinflation Protocol should be considered for patients who are at high risk for pulmonary complications as listed in the indications for Hyperinflation Protocol. 5/5/03 (Jan Phillips-Clar, Rick Ford, Judy Tietsort, Jay Peters, David Vines) AARC References for Bronchopulmonary Algorithm 1. -

Respiratory Syncytial Virus Bronchiolitis in Children DUSTIN K
Respiratory Syncytial Virus Bronchiolitis in Children DUSTIN K. SMITH, DO; SAJEEWANE SEALES, MD, MPH; and CAROL BUDZIK, MD Naval Hospital Jacksonville, Jacksonville, Florida Bronchiolitis is a common lower respiratory tract infection in infants and young children, and respiratory syncytial virus (RSV) is the most common cause of this infection. RSV is transmitted through contact with respiratory droplets either directly from an infected person or self-inoculation by contaminated secretions on surfaces. Patients with RSV bronchiolitis usually present with two to four days of upper respiratory tract symptoms such as fever, rhinorrhea, and congestion, followed by lower respiratory tract symptoms such as increasing cough, wheezing, and increased respira- tory effort. In 2014, the American Academy of Pediatrics updated its clinical practice guideline for diagnosis and man- agement of RSV bronchiolitis to minimize unnecessary diagnostic testing and interventions. Bronchiolitis remains a clinical diagnosis, and diagnostic testing is not routinely recommended. Treatment of RSV infection is mainly sup- portive, and modalities such as bronchodilators, epinephrine, corticosteroids, hypertonic saline, and antibiotics are generally not useful. Evidence supports using supplemental oxygen to maintain adequate oxygen saturation; however, continuous pulse oximetry is no longer required. The other mainstay of therapy is intravenous or nasogastric admin- istration of fluids for infants who cannot maintain their hydration status with oral fluid intake. Educating parents on reducing the risk of infection is one of the most important things a physician can do to help prevent RSV infection, especially early in life. Children at risk of severe lower respiratory tract infection should receive immunoprophy- laxis with palivizumab, a humanized monoclonal antibody, in up to five monthly doses. -

Chest Physiotherapy Page 1 of 10
UTMB RESPIRATORY CARE SERVICES Policy 7.3.9 PROCEDURE - Chest Physiotherapy Page 1 of 10 Chest Physiotherapy Effective: 10/12/94 Revised: 04/05/18 Formulated: 11/78 Chest Physiotherapy Purpose To standardize the use of chest physiotherapy as a form of therapy using one or more techniques to optimize the effects of gravity and external manipulation of the thorax by postural drainage, percussion, vibration and cough. A mechanical percussor may also be used to transmit vibrations to lung tissues. Policy Respiratory Care Services provides skilled practitioners to administer chest physiotherapy to the patient according to physician’s orders. Accountability/Training • Chest Physiotherapy is administered by a Licensed Respiratory Care Practitioner trained in the procedure(s). • Training must be equivalent to the minimal entry level in the Respiratory Care Service with the understanding of age specific requirements of the patient population treated. Physician's A written order by a physician is required specifying: Order Frequency of therapy. Lung, lobes and segments to be drained. Any physical or physiological difficulties in positioning patient. Cough stimulation as necessary. Type of supplemental oxygen, and/or adjunct therapy to be used. Indications This therapy is indicated as an adjunct in any patient whose cough alone (voluntary or induced) cannot provide adequate lung clearance or the mucociliary escalator malfunctions. This is particularly true of patients with voluminous secretions, thick tenacious secretions, and patients with neuro- muscular disorders. Drainage positions should be specific for involved segments unless contraindicated or if modification is necessary. Drainage usually in conjunction with breathing exercises, techniques of percussion, vibration and/or suctioning must have physician's order. -

Evaluation of an Alternative Chest Physiotherapy Method in Infants with Respiratory Syncytial Virus Bronchiolitis
Evaluation of an Alternative Chest Physiotherapy Method in Infants With Respiratory Syncytial Virus Bronchiolitis Guy Postiaux PT, Jacques Louis MD, Henri C Labasse MD, Julien Gerroldt PT, Anne-Claire Kotik PT, Amandine Lemuhot PT, and Caroline Patte PT BACKGROUND: We proposed a new chest physiotherapy (CPT) secretion clearance method to treat respiratory syncytial virus bronchiolitis in infants. Our new CPT method consists of 15 pro- longed slow expirations, then 5 provoked cough maneuvers. METHODS: We randomized 20 infants (mean age 4.2 months) into 2 groups: 8 patients received 27 sessions of nebulization of hypertonic saline; 12 patients received 31 sessions of nebulization of hypertonic saline followed by our new CPT method. We used the Wang clinical severity scoring system (which assesses wheezing, respiratory rate, retractions, and general condition) and measured S and heart rate before each CPT session pO2 (T0), immediately after the 30-min session (T30), and 120 min after the session (T150). RESULTS: Within the groups: in the first group, Wang score was significantly lower at T150 than at T0: 4.6 vs In the new-method-CPT group, Wang score was significantly lower at T30 (3.6 vs .(008. ؍ P) 5.0 Wheezing score was significantly lower at T150 .(002. ؍ and at T150 (3.7 vs 4.3, P (001. ؍ P ,4.3 in the first group, and in the new-method-CPT group at T30 than (02. ؍ than at T0 (1.1 vs 1.2, P Between the groups: at .(001. ؍ and at T150 than at T0 (0.9 vs 1.3, P (001. ؍ at T0 (0.8 vs 1.3, P T30 the improvement was significantly better in the new-method-CPT group for overall Wang score and heart rate (P < .001). -

Chest Physiotherapy in Cystic Fibrosis: Improved Tolerance with Nasal Pressure Support Ventilation
Chest Physiotherapy in Cystic Fibrosis: Improved Tolerance With Nasal Pressure Support Ventilation Brigitte Fauroux, MD*; Miche`le Boule´, MD, PhD‡; Fre´de´ric Lofaso, MD, PhD§; Franc¸oise Ze´rah, MD§; Annick Cle´ment, MD, PhD*; Alain Harf, MD, PhD§; and Daniel Isabey, PhD§ ABSTRACT. Objective. Chest physiotherapy (CPT) is pared with the control session. SpO2 decreases after FET an integral part of the treatment of patients with cystic were significantly larger during the control session (na- fibrosis (CF). CPT imposes additional respiratory work dir: 91.8 6 0.7%) than during the PSV session (93.8 6 that may carry a risk of respiratory muscle fatigue. In- 0.6%). Maximal pressures decreased during the control 6 6 spiratory pressure support ventilation (PSV) is a new session (from 71.9 6.1 to 60.9 5.3 cmH2O, and from 6 6 mode of ventilatory assistance designed to maintain a 85.3 7.9 to 77.5 4.8 cmH2O, for PImax and PEmax, constant preset positive airway pressure during sponta- respectively) and increased during the PSV session (from 6 6 6 neous inspiration with the goal of decreasing the pa- 71.6 8.6 to 83.9 8.7 cmH2O, and from 80.4 7.8 to 88.0 6 tient’s inspiratory work. The aim of our study was 1) to 7.4 cmH2O, for PImax and PEmax, respectively). The evaluate respiratory muscle fatigue and oxygen desatu- decrease in PEmax was significantly correlated with the ration during CPT and 2) to determine whether noninva- severity of bronchial obstruction as evaluated based on sive PSV can relieve these potential adverse effects of baseline FEV1 (% predicted). -

Randomized Controlled Trial a Fisioterapia Respiratória É Eficaz Na Redução De Escore Clínico Na Bronquiolite: Ensaio Controlado Randomizado
ISSN 1413-3555 Rev Bras Fisioter, São Carlos, v. 16, n. 3, p. 241-7, May/June 2012 ORIGINAL ARTICLE ©Revista Brasileira de Fisioterapia Chest physical therapy is effective in reducing the clinical score in bronchiolitis: randomized controlled trial A fisioterapia respiratória é eficaz na redução de escore clínico na bronquiolite: ensaio controlado randomizado Évelim L. F. D. Gomes1, Guy Postiaux2, Denise R. L. Medeiros3, Kadma K. D. S. Monteiro4, Luciana M. M. Sampaio5, Dirceu Costa5 Abstract Objective: To evaluate the effectiveness of chest physical therapy (CP) in reducing the clinical score in infants with acute viral bronchiolitis (AVB). Methods: Randomized controlled trial of 30 previously healthy infants (mean age 4.08 SD 3.0 months) with AVB and positive for respiratory syncytial virus (RSV), evaluated at three moments: at admission, then at 48 and 72 hours after admission. The procedures were conducted by blinded assessors to each of three groups: G1 - new Chest Physical therapy- nCPT (Prolonged slow expiration - PSE and Clearance rhinopharyngeal retrograde - CRR), G2 - conventional Chest Physical therapy- cCPT (modified postural drainage, expiratory compression, vibration and percussion) and G3 - aspiration of the upper airways. The outcomes of interest were the Wang’s clinical score (CS) and its components: Retractions (RE), Respiratory Rate (RR), Wheezing (WH) and General Conditions (GC). Results: The CS on admission was reduced in G1 (7.0-4.0) and G2 (7.5-5.5) but was unchanged in G3 (7.5-7.0). We observed a change 48 hours after hospitalization in G1 (5.5-3.0) and G2 (4.0-2.0) and in 72 hours, there was a change in G1 (2.0-1.0). -

Evidence Based Chest Physiotherapy for Cystic Fibrosis
Short Communication ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2019.15.002673 Evidence Based Chest Physiotherapy for Cystic Fibrosis Mohammad Habibur Rahman* Lecturer (Physiotherapy), School of Science and Technology, Bangladesh Open University, Gazipur-1705, Bangladesh *Corresponding author: Mohammad Habibur Rahman, Lecturer (Physiotherapy), School of Science and Technology, Bangladesh Open University, Gazipur-1705, Bangladesh ARTICLE INFO abstract Received: Published: of bronchial sections. In addition to medicine different physiotherapy treatment techniques February 14, 2019 Cystic fibrosis (CF) is a genetically predisposed disease causing difficulties in clearance February 27, 2019 clear bronchial sections and lessen the work of breathing. Absolute indication and dose Citation: Mohammad Habibur Rah- basedfor instance chest physiotherapypostural drainage, is mandatory percussion, and chest evidence shaking, based huffing physiotherapy and coughing practice helps is es to- man. Evidence Based Chest Physio- J Sci & Tech Res 15(2)-2019. BJSTR. sentialAbbreviations: for livelihood of a CF patient. MS.ID.002673.therapy for Cystic Fibrosis. Biomed - CF: Cystic Fibrosis; PEP: Positive Expiratory Pressure; HPEP: High pressure PEP; P&PD: Percussion and Postural Drainage; OPEP: Oscillatory PEP; HFCC: High Frequen cy Chest Compressions; AD: Autogenic Drainage. Introduction Pulmonary diseases regarded as one of the main sources Among the eight crosses over studies, six experiments focused of limitation in daily livelihood. These limitations are highly on single treatment approaches in which four experiments comprising of 28 participants was found a huge amount of of breathlessness and decrease exercise tolerance [1]. Chest expelled secretions after application of chest physiotherapy when influenced by difficulties to clear bronchial secretions, symptoms compared to no treatment option. One experiment was conducted on 18 participants and found similarities of sputum weight when disease like cystic fibrosis (CF) exhibited similar features described compared to control group. -
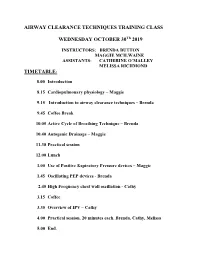
Introduction to Airway Clearance Techniques – Brenda
AIRWAY CLEARANCE TECHNIQUES TRAINING CLASS WEDNESDAY OCTOBER 30Th 2019 INSTRUCTORS: BRENDA BUTTON MAGGIE MCILWAINE ASSISTANTS: CATHERINE O’MALLEY MELISSA RICHMOND TIMETABLE: 8.00 Introduction 8.15 Cardiopulmonary physiology – Maggie 9.15 Introduction to airway clearance techniques – Brenda 9.45 Coffee Break 10.05 Active Cycle of Breathing Technique – Brenda 10.40 Autogenic Drainage – Maggie 11.30 Practical session 12.00 Lunch 1.00 Use of Positive Expiratory Pressure devices – Maggie 1.45 Oscillating PEP devices - Brenda 2.45 High Frequency chest wall oscillation - Cathy 3.15 Coffee 3.35 Overview of IPV – Cathy 4.00 Practical session. 20 minutes each. Brenda, Cathy, Melissa 5.00 End. 8/1/2019 Airway Clearance Techniques Training class Dr Maggie McIlwaine and Dr Brenda Button Catherine O’Malley Melissa Richmond Objectives • Explain the physiology, and theory behind airway clearance techniques currently used in the treatment of cystic fibrosis. • Demonstrate the airway clearance techniques of Active cycle of breathing techniques, autogenic drainage, PEP, oscillating PEP, HFCWO and IPV. • Compose the scientific evidence supporting the use of each of these techniques. Timetable • 8.00 Introduction: Maggie • 8.15 Cardiopulmonary physiology – Maggie • 9.15 Introduction to airway clearance and breathing techniques – Brenda • 9.45 Coffee break • 10.05 The Active Cycle of Breathing Techniques - Brenda • 10.40 Autogenic Drainage Maggie • 11.30 Practical session • 12.00 Lunch M. McIlwaine 1 8/1/2019 Timetable • 1.00 Use of Positive Expiratory Pressure Devices – Maggie • 1.45 Oscillating PEP Devices – Brenda • 2.45 C High Frequency Chest wall Oscillation (HFCWO) therapy-Coffee • 3.15 Coffee • 3.35 Overview of IPV – Cathy • 4.00 Practical session. -
Treating Bronchiectasis
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES Treating Bronchiectasis Bronchiectasis (bron-kee-eck-tuh-sis) is a lung condition that causes cough, sputum production, and recurrent respiratory infections. (Also see “What is Bronchiectasis?” at www.thoracic.org/patients). Because bronchiectasis is a condition that develops over many years and worsens with repeated infections, the main treatment goal is to reduce stagnant secretions (mucus, sputum) in the airways and germs contained in those secretions. Your healthcare provider will help you figure out the ■ chest physiotherapy involves chest clapping in best treatment plan for you. There are two important various positions to move mucus up to the windpipe parts of bronchiectasis treatment: so that you can cough it out. ■ Maintenance: What you do every day. This usually ■ handheld positive expiratory pressure (PEP) devices includes airway clearance, changes in your lifestyle, are used to loosen mucus by creating vibration while and other actions you can take to prevent infections and lung damage. breathing through the device. ■ Exacerbations (eg-zass-er-bay-shuns): What you do ■ percussion devices which can include mechanical when you get sick and have a change in symptoms. percussors and percussive vests (high frequency This usually includes increasing airway clearance and chest wall oscilliation) are used to loosen mucus and CLIP AND COPY AND CLIP taking antibiotics to treat infection. move it to the windpipe to cough out. What are airway clearance techniques? All forms of airway clearance depend on good coughs Depending on how severe your bronchiectasis is and how much mucus is produced in your airways, your to move loose mucus out. -

Conventional Chest Physical Therapy for Obstructive Lung Disease
Conventional Chest Physical Therapy for Obstructive Lung Disease Cees P van der Schans PT PhD Introduction Conventional Chest Physical Therapy Directed Cough and Forced Expirations Postural Drainage Chest Percussion Other Airway Clearance Techniques High-Frequency Chest Wall Compression Positive Expiratory Pressure Therapy Autogenic Drainage Exercise Vibratory PEP Therapy Identifying Patients Who Will Benefit From CPT Selecting and Applying CPT Components Promoting Patient Adherence to CPT Risks and Adverse Effects of CPT Summary Chest physical therapy (CPT) is a widely used intervention for patients with airway diseases. The main goal is to facilitate secretion transport and thereby decrease secretion retention in the airways. Histor- ically, conventional CPT has consisted of a combination of forced expirations (directed cough or huff), postural drainage, percussion, and/or shaking. CPT improves mucus transport, but it is not entirely clear which groups of patients benefit from which CPT modalities. In general, the patients who benefit most from CPT are those with airways disease and objective signs of secretion retention (eg, persistent rhonchi or decreased breath sounds) or subjective signs of difficulty expectorating sputum, and with progression of disease that might be due to secretion retention (eg, recurrent exacerbations, infections, or a fast decline in pulmonary function). The most effective and important part of conventional CPT is directed cough. The other components of conventional CPT add little if any benefit and should not be used routinely. Alternative airway clearance modalities (eg, high-frequency chest wall compression, vibratory positive expiratory pressure, and exercise) are not proven to be more effective than conven- tional CPT and usually add little benefit to conventional CPT. -

Respiratory Physiotherapy in the Bronchiectasis Guidelines: Is There a Loud Voice We Are Yet to Hear?
EDITORIAL | BRONCHIECTASIS Respiratory physiotherapy in the bronchiectasis guidelines: is there a loud voice we are yet to hear? Arietta Spinou 1 and James D. Chalmers2 Affiliations: 1Population Health Sciences, Life Sciences and Medicine, King’s College London, London, UK. 2School of Medicine, University of Dundee, Dundee, UK. Correspondence: Arietta Spinou, Dept of Population Health Sciences, School of Population Health and Environmental Sciences, 2nd floor, Addison House, Guy’s Campus, King’s College London, London, SE1 1UL, UK. E-mail: [email protected] @ERSpublications A call for action for great awareness and research into airway clearance techniques and pulmonary rehabilitation in bronchiectasis http://bit.ly/2L8F4Va Cite this article as: Spinou A, Chalmers JD. Respiratory physiotherapy in the bronchiectasis guidelines: is there a loud voice we are yet to hear? Eur Respir J 2019; 54: 1901610 [https://doi.org/10.1183/ 13993003.01610-2019]. Bronchiectasis is a chronic respiratory disease of airway dilatation, where patients typically suffer from respiratory infections, fatigue, sputum, cough, dyspnoea and poor quality of life [1, 2]. This condition has received increased interest over the past years, with important developments in establishing national and international patient registries [3–5], randomised controlled trials of new treatments [6–8] and disease-specific health status questionnaires, such as the Bronchiectasis Health Questionnaire and the Quality of Life Questionnaire – Bronchiectasis [9, 10]. A number of new treatment approaches have been proposed including long term antibiotic therapies and immune modulating drugs [6, 7, 11, 12]. Nevertheless the area of bronchiectasis care that has received the least attention during this period is the aspect of management that most healthcare professionals caring for bronchiectasis agree is the most important: airway clearance and exercise [13, 14]. -

AARC Clinical Practice Guideline: Effectiveness of Nonpharmacologic Airway Clearance Therapies in Hospitalized Patients
AARC Clinical Practice Guideline: Effectiveness of Nonpharmacologic Airway Clearance Therapies in Hospitalized Patients Shawna L Strickland PhD RRT-NPS AE-C FAARC, Bruce K Rubin MD MEngr MBA FAARC, Gail S Drescher MA RRT, Carl F Haas MLS RRT FAARC, Catherine A O’Malley RRT-NPS, Teresa A Volsko MHHS RRT FAARC, Richard D Branson MSc RRT FAARC, and Dean R Hess PhD RRT FAARC Airway clearance therapy (ACT) is used in a variety of settings for a variety of ailments. These guidelines were developed from a systematic review with the purpose of determining whether the use of nonpharmacologic ACT improves oxygenation, reduces length of time on the ventilator, reduces stay in the ICU, resolves atelectasis/consolidation, and/or improves respiratory mechanics, versus usual care in 3 populations. For hospitalized, adult and pediatric patients without cystic fibrosis, 1) chest physiotherapy (CPT) is not recommended for the routine treatment of uncompli- cated pneumonia; 2) ACT is not recommended for routine use in patients with COPD; 3) ACT may be considered in patients with COPD with symptomatic secretion retention, guided by patient preference, toleration, and effectiveness of therapy; 4) ACT is not recommended if the patient is able to mobilize secretions with cough, but instruction in effective cough technique may be useful. For adult and pediatric patients with neuromuscular disease, respiratory muscle weakness, or impaired cough, 1) cough assist techniques should be used in patients with neuromuscular disease, particularly when peak cough flow is < 270 L/min; CPT, positive expiratory pressure, intrapul- monary percussive ventilation, and high-frequency chest wall compression cannot be recommended, due to insufficient evidence.