Diseases Or Fungal Infections Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Estimated Burden of Serious Fungal Infections in Ghana
Journal of Fungi Article Estimated Burden of Serious Fungal Infections in Ghana Bright K. Ocansey 1, George A. Pesewu 2,*, Francis S. Codjoe 2, Samuel Osei-Djarbeng 3, Patrick K. Feglo 4 and David W. Denning 5 1 Laboratory Unit, New Hope Specialist Hospital, Aflao 00233, Ghana; [email protected] 2 Department of Medical Laboratory Sciences, School of Biomedical and Allied Health Sciences, College of Health Sciences, University of Ghana, P.O. Box KB-143, Korle-Bu, Accra 00233, Ghana; [email protected] 3 Department of Pharmaceutical Sciences, Faculty of Health Sciences, Kumasi Technical University, P.O. Box 854, Kumasi 00233, Ghana; [email protected] 4 Department of Clinical Microbiology, School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi 00233, Ghana; [email protected] 5 National Aspergillosis Centre, Wythenshawe Hospital and the University of Manchester, Manchester M23 9LT, UK; [email protected] * Correspondence: [email protected] or [email protected] or [email protected]; Tel.: +233-277-301-300; Fax: +233-240-190-737 Received: 5 March 2019; Accepted: 14 April 2019; Published: 11 May 2019 Abstract: Fungal infections are increasingly becoming common and yet often neglected in developing countries. Information on the burden of these infections is important for improved patient outcomes. The burden of serious fungal infections in Ghana is unknown. We aimed to estimate this burden. Using local, regional, or global data and estimates of population and at-risk groups, deterministic modelling was employed to estimate national incidence or prevalence. Our study revealed that about 4% of Ghanaians suffer from serious fungal infections yearly, with over 35,000 affected by life-threatening invasive fungal infections. -

Fungal Infections from Human and Animal Contact
Journal of Patient-Centered Research and Reviews Volume 4 Issue 2 Article 4 4-25-2017 Fungal Infections From Human and Animal Contact Dennis J. Baumgardner Follow this and additional works at: https://aurora.org/jpcrr Part of the Bacterial Infections and Mycoses Commons, Infectious Disease Commons, and the Skin and Connective Tissue Diseases Commons Recommended Citation Baumgardner DJ. Fungal infections from human and animal contact. J Patient Cent Res Rev. 2017;4:78-89. doi: 10.17294/2330-0698.1418 Published quarterly by Midwest-based health system Advocate Aurora Health and indexed in PubMed Central, the Journal of Patient-Centered Research and Reviews (JPCRR) is an open access, peer-reviewed medical journal focused on disseminating scholarly works devoted to improving patient-centered care practices, health outcomes, and the patient experience. REVIEW Fungal Infections From Human and Animal Contact Dennis J. Baumgardner, MD Aurora University of Wisconsin Medical Group, Aurora Health Care, Milwaukee, WI; Department of Family Medicine and Community Health, University of Wisconsin School of Medicine and Public Health, Madison, WI; Center for Urban Population Health, Milwaukee, WI Abstract Fungal infections in humans resulting from human or animal contact are relatively uncommon, but they include a significant proportion of dermatophyte infections. Some of the most commonly encountered diseases of the integument are dermatomycoses. Human or animal contact may be the source of all types of tinea infections, occasional candidal infections, and some other types of superficial or deep fungal infections. This narrative review focuses on the epidemiology, clinical features, diagnosis and treatment of anthropophilic dermatophyte infections primarily found in North America. -

Serious Fungal Infections in Peru
Eur J Clin Microbiol Infect Dis DOI 10.1007/s10096-017-2924-9 ORIGINAL ARTICLE Serious fungal infections in Peru B. Bustamante1 & D. W. Denning2 & P. E. Campos3 Received: 21 December 2016 /Accepted: 21 December 2016 # Springer-Verlag Berlin Heidelberg 2017 Abstract Epidemiological data about mycotic diseases are This first attempt to assess the fungal burden in Peru needs limited in Peru and estimation of the fungal burden has not to be refined. We believe the figure obtained is an underesti- been previously attempted. Data were obtained from the mation, because of under diagnosis, non-mandatory reporting Peruvian National Institute of Statistics and Informatics, and lack of a surveillance system and of good data about the UNAIDS and from the Ministry of Health’s publications. size of populations at risk. We also searched the bibliography for Peruvian data on my- cotic diseases, asthma, COPD, cancer and transplants. Incidence or prevalence for each fungal disease were estimat- Introduction ed in specific populations at risk. The Peruvian population for 2015 was 31,151,543. In 2014, the estimated number of HIV/ While candidemia and invasive aspergillosis (IA) are clearly AIDS and pulmonary tuberculosis cases was 88,625, 38,581 recognized as important causes of morbidity and mortality, of them not on ART, and 22,027, respectively. A total of other mycotic agents or different clinical presentations are im- 581,174 cases of fungal diseases were estimated, representing portant in specific regions. Socio-economic and geo- approximately 1.9% of the Peruvian population. This figure ecological characteristics and size of susceptible populations includes 498,606, 17,361 and 4,431 vulvovaginal, oral and are the main determinants of variations on incidence of fungal esophageal candidiasis, respectively, 1,557 candidemia cases, infections across the world. -

Oral Antifungals Month/Year of Review: July 2015 Date of Last
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Class Update with New Drug Evaluation: Oral Antifungals Month/Year of Review: July 2015 Date of Last Review: March 2013 New Drug: isavuconazole (a.k.a. isavunconazonium sulfate) Brand Name (Manufacturer): Cresemba™ (Astellas Pharma US, Inc.) Current Status of PDL Class: See Appendix 1. Dossier Received: Yes1 Research Questions: Is there any new evidence of effectiveness or safety for oral antifungals since the last review that would change current PDL or prior authorization recommendations? Is there evidence of superior clinical cure rates or morbidity rates for invasive aspergillosis and invasive mucormycosis for isavuconazole over currently available oral antifungals? Is there evidence of superior safety or tolerability of isavuconazole over currently available oral antifungals? • Is there evidence of superior effectiveness or safety of isavuconazole for invasive aspergillosis and invasive mucormycosis in specific subpopulations? Conclusions: There is low level evidence that griseofulvin has lower mycological cure rates and higher relapse rates than terbinafine and itraconazole for adult 1 onychomycosis.2 There is high level evidence that terbinafine has more complete cure rates than itraconazole (55% vs. 26%) for adult onychomycosis caused by dermatophyte with similar discontinuation rates for both drugs.2 There is low -

Tinea Capitis 2014 L.C
BJD GUIDELINES British Journal of Dermatology British Association of Dermatologists’ guidelines for the management of tinea capitis 2014 L.C. Fuller,1 R.C. Barton,2 M.F. Mohd Mustapa,3 L.E. Proudfoot,4 S.P. Punjabi5 and E.M. Higgins6 1Department of Dermatology, Chelsea & Westminster Hospital, Fulham Road, London SW10 9NH, U.K. 2Department of Microbiology, Leeds General Infirmary, Leeds LS1 3EX, U.K. 3British Association of Dermatologists, Willan House, 4 Fitzroy Square, London W1T 5HQ, U.K. 4St John’s Institute of Dermatology, Guy’s and St Thomas’ NHS Foundation Trust, St Thomas’ Hospital, Westminster Bridge Road, London SE1 7EH, U.K. 5Department of Dermatology, Hammersmith Hospital, 150 Du Cane Road, London W12 0HS, U.K. 6Department of Dermatology, King’s College Hospital, Denmark Hill, London SE5 9RS, U.K. 1.0 Purpose and scope Correspondence Claire Fuller. The overall objective of this guideline is to provide up-to- E-mail: [email protected] date, evidence-based recommendations for the management of tinea capitis. This document aims to update and expand Accepted for publication on the previous guidelines by (i) offering an appraisal of 8 June 2014 all relevant literature since January 1999, focusing on any key developments; (ii) addressing important, practical clini- Funding sources cal questions relating to the primary guideline objective, i.e. None. accurate diagnosis and identification of cases; suitable treat- ment to minimize duration of disease, discomfort and scar- Conflicts of interest ring; and limiting spread among other members of the L.C.F. has received sponsorship to attend conferences from Almirall, Janssen and LEO Pharma (nonspecific); has acted as a consultant for Alliance Pharma (nonspe- community; (iii) providing guideline recommendations and, cific); and has legal representation for L’Oreal U.K. -

Tinea Capitis: Unusual Chronic Presentation in an Elderly Woman
ISSN: 2474-3658 Salazar et al. J Infect Dis Epidemiol 2018, 4:048 DOI: 10.23937/2474-3658/1510048 Volume 4 | Issue 1 Journal of Open Access Infectious Diseases and Epidemiology CASE REPORT Tinea Capitis: Unusual Chronic Presentation in an Elderly Woman Elizabeth Salazar1*, Daniel Asz-Sigall2, Diana Vega3 and Roberto Arenas4 1Dermato-Oncologist, Private Practice, Mexico City, Mexico 2 Check for Dermatologist, Dermato-Oncology and Trichology Clinic, National University of Mexico, Mexico City, Mexico updates 3Mycologist, Mycology Section, Hospital General “Dr. Manuel Gea González”, Mexico City, Mexico 4Dermatologist and Mycologist, Mycology Section, General Hospital “Dr. Manuel Gea González”, Mexico City, Mexico *Corresponding authors: Elizabeth Salazar, Dermato-Oncologist, Private Practice, Mexico City, Mexico, E-mail: dra. [email protected] The non-inflammatory clinical presentation can be Abstract found in 90% of affected children. It is more frequent in Tinea capitis is a superficial fungal infection of the scalp tropical regions with low socioeconomic conditions and and hair caused by dermatophytes such as Trichophyton and Microsporum. Tinea capitis is very rare in adults, and affects almost exclusively children (98%). The inflamma- may affect those with immunosuppressive diseases or tory form is observed only in 10% and most commonly menopausal elderly women. Clinical manifestations along seen in prepubescent children. Tinea capitis is caused with trichoscopy and Wood’s light, can help the clinician to by dermatophytes that use keratin as a nutrient source. determine the correct diagnosis, in order to reduce irrevers- Scalp erythema, scaling, and crusting are typical signs of ible sequelae and decrease multiple contagion. KOH direct exam and culture confirm diagnosis and aetiology. -

Mucormycosis: a Review on Environmental Fungal Spores and Seasonal Variation of Human Disease
Advances in Infectious Diseases, 2012, 2, 76-81 http://dx.doi.org/10.4236/aid.2012.23012 Published Online September 2012 (http://www.SciRP.org/journal/aid) Mucormycosis: A Review on Environmental Fungal Spores and Seasonal Variation of Human Disease Rima I. El-Herte, Tania A. Baban, Souha S. Kanj* Division of Infectious Diseases, Department of Internal Medicine, American University of Beirut Medical Center, Beirut, Lebanon. Email: *[email protected] Received May 1st, 2012; revised June 3rd, 2012; accepted July 5th, 2012 ABSTRACT Mucormycosis is on the rise especially among patients with immunosuppressive conditions. There seems to be more cases seen at the end of summer and towards early autumn. Several studies have attempted to look at the seasonal varia- tions of fungal pathogens in variou indoor and outdoor settings. Only two reports, both from the Middle East, have ad- dressed the relationship of mucormycosis in human disease with climate conditions. In this paper we review, the rela- tionship of indoor and outdoor fungal particulates to the weather conditions and the reported seasonal variation of hu- man cases. Keywords: Mucormycosis; Seasonal Variation; Fungal Air Particulate Concentration; Mucor; Rhizopus; Rhinocerebral 1. Introduction bread, decaying fruits, vegetable matters, crop debris, soil, compost piles, animal excreta, and on excavation and con- Mucormycosis refers to infections caused by molds be- struction sites. Sporangiospores are easily aerosolized, and longing to the order of Mucorales. Members of the fam- are readily dispersed throughout the environment making ily Mucoraceae are the most common cause of mucor- inhalation the major mode of transmission. Published data mycosis in humans. -

Detection of Histoplasma DNA from Tissue Blocks by a Specific
Journal of Fungi Article Detection of Histoplasma DNA from Tissue Blocks by a Specific and a Broad-Range Real-Time PCR: Tools to Elucidate the Epidemiology of Histoplasmosis Dunja Wilmes 1,*, Ilka McCormick-Smith 1, Charlotte Lempp 2 , Ursula Mayer 2 , Arik Bernard Schulze 3 , Dirk Theegarten 4, Sylvia Hartmann 5 and Volker Rickerts 1 1 Reference Laboratory for Cryptococcosis and Uncommon Invasive Fungal Infections, Division for Mycotic and Parasitic Agents and Mycobacteria, Robert Koch Institute, 13353 Berlin, Germany; [email protected] (I.M.-S.); [email protected] (V.R.) 2 Vet Med Labor GmbH, Division of IDEXX Laboratories, 71636 Ludwigsburg, Germany; [email protected] (C.L.); [email protected] (U.M.) 3 Department of Medicine A, Hematology, Oncology and Pulmonary Medicine, University Hospital Muenster, 48149 Muenster, Germany; [email protected] 4 Institute of Pathology, University Hospital Essen, University Duisburg-Essen, 45147 Essen, Germany; [email protected] 5 Senckenberg Institute for Pathology, Johann Wolfgang Goethe University Frankfurt, 60323 Frankfurt am Main, Germany; [email protected] * Correspondence: [email protected]; Tel.: +49-30-187-542-862 Received: 10 November 2020; Accepted: 25 November 2020; Published: 27 November 2020 Abstract: Lack of sensitive diagnostic tests impairs the understanding of the epidemiology of histoplasmosis, a disease whose burden is estimated to be largely underrated. Broad-range PCRs have been applied to identify fungal agents from pathology blocks, but sensitivity is variable. In this study, we compared the results of a specific Histoplasma qPCR (H. qPCR) with the results of a broad-range qPCR (28S qPCR) on formalin-fixed, paraffin-embedded (FFPE) tissue specimens from patients with proven fungal infections (n = 67), histologically suggestive of histoplasmosis (n = 36) and other mycoses (n = 31). -

Geophilic Dermatophytes and Other Keratinophilic Fungi in the Nests of Wetland Birds
ACTA MyCoLoGICA Vol. 46 (1): 83–107 2011 Geophilic dermatophytes and other keratinophilic fungi in the nests of wetland birds Teresa KoRnIŁŁoWICz-Kowalska1, IGnacy KIToWSKI2 and HELEnA IGLIK1 1Department of Environmental Microbiology, Mycological Laboratory University of Life Sciences in Lublin Leszczyńskiego 7, PL-20-069 Lublin, [email protected] 2Department of zoology, University of Life Sciences in Lublin, Akademicka 13 PL-20-950 Lublin, [email protected] Korniłłowicz-Kowalska T., Kitowski I., Iglik H.: Geophilic dermatophytes and other keratinophilic fungi in the nests of wetland birds. Acta Mycol. 46 (1): 83–107, 2011. The frequency and species diversity of keratinophilic fungi in 38 nests of nine species of wetland birds were examined. nine species of geophilic dermatophytes and 13 Chrysosporium species were recorded. Ch. keratinophilum, which together with its teleomorph (Aphanoascus fulvescens) represented 53% of the keratinolytic mycobiota of the nests, was the most frequently observed species. Chrysosporium tropicum, Trichophyton terrestre and Microsporum gypseum populations were less widespread. The distribution of individual populations was not uniform and depended on physical and chemical properties of the nests (humidity, pH). Key words: Ascomycota, mitosporic fungi, Chrysosporium, occurrence, distribution INTRODUCTION Geophilic dermatophytes and species representing the Chrysosporium group (an arbitrary term) related to them are ecologically classified as keratinophilic fungi. Ke- ratinophilic fungi colonise keratin matter (feathers, hair, etc., animal remains) in the soil, on soil surface and in other natural environments. They are keratinolytic fungi physiologically specialised in decomposing native keratin. They fully solubilise na- tive keratin (chicken feathers) used as the only source of carbon and energy in liquid cultures after 70 to 126 days of growth (20°C) (Korniłłowicz-Kowalska 1997). -

Mycoses and Anti-Fungals – an Update
REVIEW Mycoses and anti-fungals – an update N Schellack, J du Toit, T Mokoena, E Bronkhorst School of Pharmacy, Faculty of Health Sciences, Sefako Makgatho Health Sciences University, South Africa Corresponding author, email: [email protected] Abstract Fungi normally originate from the environment that surrounds us, and appear to be harmless until inhaled or ingestion of spores occur. For many years fungal infections were thought of as superficial diseases or infections such as athlete’s foot, or vulvovaginal candidiasis. Subsequently, when invasive fungal infections were first encountered, amphotericin B was the only treatment for systemic mycoses. However, with the advances in medical technology such as bone marrow transplants, cytotoxic chemotherapy, indwelling catheters as well as with the increased use of broad spectrum antimicrobials in antimicrobial resistance, there has been a marked increase of fungal infections worldwide. Populations at risk of acquiring fungal infections are those living with human immunodeficiency virus (HIV), cancer, patients receiving immunosuppressant therapy, neonates and those of advanced age. The management of superficial fungal infections is mainly topical, with agents including terbinafine, miconazole and ketoconazole. Oral treatment includes griseofulvin and fluconazole. Historically the management of invasive fungal infections involved the use of amphotericin B, however newer agents include the azoles and the echinocandins. This paper provides a general overview of the management of fungus infections. Keywords: invasive fungal diseases, superficial fungal diseases, fungal skin infections © Medpharm S Afr Pharm J 2020;87(1):18-25 Introduction the pathogen, site of growth (either host or laboratory setting), and temperature. Some can be a combination of both, which are Fungi normally originate from the environment that surrounds called dimorphic. -
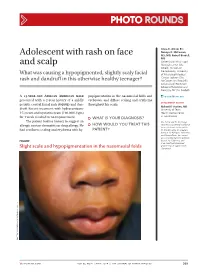
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Advantages of Mold Ige Allergy Test & Mycotox Profile
Advantages of Mold IgE Allergy Test & MycoTOX Profile Comprehensive Analysis of Mold Exposure SIGNIFICANCE OF IGE MOLD ALLERGY TESTING ■ Mold allergy is an abnormal immune reaction to mold spores or mold cell components. People can be exposed to mold spores or byproducts at work, home or outdoors. ■ Certain occupations have potential for high mold exposure: crop and dairy farming, greenhouse plant husbandry, logging, carpentry, millwork, furniture repair and commercial baking. ■ A high exposure in the home can occur in damp areas such as bathrooms, kitchens and basements. ■ In general, working or living in damp buildings with moisture higher than 50% humidity, increases the possibility of mold exposure. ■ Immune reactions to mold can be identified by the level of immunoglobulin E (IgE) antibodies to specific mold species. ■ The Great Plains Laboratory now offers an IgE blood test that measures patient antibodies to most common molds. The IgE antibodies are detected in blood serum using an FDA-approved enzyme-linked immunosorbent assay (ELISA). ■ The most common molds known to cause allergic conditions include Alternaria, Aspergillus, Cladosporium and Penicillium. Use of both tests allow a wider array of molds to be detected. ■ The Mold IgE Allergy panel includes 13 mold allergens, with markers known to be involved in mold-related illnesses. SPECIMEN REQUIREMENTS Mold IgE Allergy Test 2 mL of serum MycoTOX Profile 10 mL of first morning urine COMPARISON OF IGE MOLD AND MYCOTOX PROFILE ■ IgE looks at immune response to mold exposure. ■ MycoTOX Profile looks at mycotoxin levels excreted from the body. ■ Mold allergies and mold mycotoxin toxicity are distinct responses related to mold illness.