Supplementation with Fermented Rice Bran Attenuates Muscle Atrophy in a Diabetic Rat Model
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

FBXO32 Promotes Microenvironment Underlying Epithelial-Mesenchymal Transition Via Ctbp1 During Tumour Metastasis and Brain Development
FBXO32 promotes microenvironment underlying epithelial- mesenchymal transition via CtBP1 during tumour metastasis and brain development Sahu, S. K., Tiwari, N., Pataskar, A., Zhuang, Y., Borisova, M., Diken, M., Strand, S., Beli, P., & Tiwari, V. K. (2017). FBXO32 promotes microenvironment underlying epithelial-mesenchymal transition via CtBP1 during tumour metastasis and brain development. Nature Communications, 8(1), [1523]. https://doi.org/10.1038/s41467-017-01366-x Published in: Nature Communications Document Version: Publisher's PDF, also known as Version of record Queen's University Belfast - Research Portal: Link to publication record in Queen's University Belfast Research Portal Publisher rights Copyright 2017 the authors. This is an open access article published under a Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution and reproduction in any medium, provided the author and source are cited. General rights Copyright for the publications made accessible via the Queen's University Belfast Research Portal is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The Research Portal is Queen's institutional repository that provides access to Queen's research output. Every effort has been made to ensure that content in the Research Portal does not infringe any person's rights, or applicable UK laws. If you discover content in the Research Portal that you believe breaches copyright or violates any law, please contact [email protected]. Download date:27. Sep. 2021 ARTICLE DOI: 10.1038/s41467-017-01366-x OPEN FBXO32 promotes microenvironment underlying epithelial-mesenchymal transition via CtBP1 during tumour metastasis and brain development Sanjeeb Kumar Sahu1, Neha Tiwari2, Abhijeet Pataskar1, Yuan Zhuang1, Marina Borisova1, Mustafa Diken3, Susanne Strand4, Petra Beli1 & Vijay K. -

Anti-FBXO32 Antibody (ARG55503)
Product datasheet [email protected] ARG55503 Package: 100 μl anti-FBXO32 antibody Store at: -20°C Summary Product Description Rabbit Polyclonal antibody recognizes FBXO32 Tested Reactivity Ms Predict Reactivity Hu, Rat Tested Application WB Host Rabbit Clonality Polyclonal Isotype IgG Target Name FBXO32 Antigen Species Human Immunogen Recombinant protein of Human FBXO32 Conjugation Un-conjugated Alternate Names Muscle atrophy F-box protein; Atrogin-1; F-box only protein 32; Fbx32; MAFbx Application Instructions Application table Application Dilution WB 1:500 - 1:2000 Application Note * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Positive Control Mouse heart Calculated Mw 42 kDa Properties Form Liquid Purification Affinity purification with immunogen. Buffer PBS (pH 7.3), 0.02% Sodium azide and 50% Glycerol Preservative 0.02% Sodium azide Stabilizer 50% Glycerol Storage instruction For continuous use, store undiluted antibody at 2-8°C for up to a week. For long-term storage, aliquot and store at -20°C. Storage in frost free freezers is not recommended. Avoid repeated freeze/thaw cycles. Suggest spin the vial prior to opening. The antibody solution should be gently mixed before use. Note For laboratory research only, not for drug, diagnostic or other use. www.arigobio.com 1/2 Bioinformation Database links GeneID: 67731 Mouse Swiss-port # Q9CPU7 Mouse Gene Symbol FBXO32 Gene Full Name F-box protein 32 Background This gene encodes a member of the F-box protein family which is characterized by an approximately 40 amino acid motif, the F-box. The F-box proteins constitute one of the four subunits of the ubiquitin protein ligase complex called SCFs (SKP1-cullin-F-box), which function in phosphorylation-dependent ubiquitination. -

Satellite Cell Senescence Underlies Myopathy in a Mouse Model of Limb-Girdle Muscular Dystrophy 2H Elena Kudryashova, Irina Kramerova, and Melissa J
Research article Satellite cell senescence underlies myopathy in a mouse model of limb-girdle muscular dystrophy 2H Elena Kudryashova, Irina Kramerova, and Melissa J. Spencer Department of Neurology, Center for Duchenne Muscular Dystrophy at UCLA, David Geffen School of Medicine at UCLA, Los Angeles, California, USA. Mutations in the E3 ubiquitin ligase tripartite motif-containing 32 (TRIM32) are responsible for the disease limb-girdle muscular dystrophy 2H (LGMD2H). Previously, we generated Trim32 knockout mice (Trim32–/– mice) and showed that they display a myopathic phenotype accompanied by neurogenic features. Here, we used these mice to investigate the muscle-specific defects arising from the absence of TRIM32, which underlie the myopathic phenotype. Using 2 models of induced atrophy, we showed that TRIM32 is dispensable for muscle atrophy. Conversely, TRIM32 was necessary for muscle regrowth after atrophy. Furthermore, TRIM32-defi- cient primary myoblasts underwent premature senescence and impaired myogenesis due to accumulation of PIAS4, an E3 SUMO ligase and TRIM32 substrate that was previously shown to be associated with senescence. Premature senescence of myoblasts was also observed in vivo in an atrophy/regrowth model. Trim32–/– muscles had substantially fewer activated satellite cells, increased PIAS4 levels, and growth failure compared with wild- type muscles. Moreover, Trim32–/– muscles exhibited features of premature sarcopenia, such as selective type II fast fiber atrophy. These results imply that premature senescence of muscle satellite cells is an underlying pathogenic feature of LGMD2H and reveal what we believe to be a new mechanism of muscular dystrophy associated with reductions in available satellite cells and premature sarcopenia. Introduction and are primarily characterized by proximal muscle weakness and Tripartite motif-containing 32 (TRIM32) is a member of the tri- wasting. -

Full Text (PDF)
Published OnlineFirst August 29, 2012; DOI: 10.1158/1078-0432.CCR-12-0873 Clinical Cancer Cancer Therapy: Preclinical Research Superior Efficacy of a Combined Epigenetic Therapy against Human Mantle Cell Lymphoma Cells Warren Fiskus1, Rekha Rao1, Ramesh Balusu1, Siddhartha Ganguly1, Jianguo Tao2, Eduardo Sotomayor2, Uma Mudunuru1, Jacqueline E. Smith1, Stacey L. Hembruff1, Peter Atadja3, Victor E. Marquez4, and Kapil Bhalla1 Abstract Purpose: A deregulated epigenome contributes to the transformed phenotype of mantle cell lymphoma (MCL). This involves activity of the polycomb repressive complex (PRC) 2, containing three core proteins, EZH2, SUZ12, and EED, in which the SET domain of EZH2 mediates the histone methyltransferase activity. We determined the effects of 3-deazaneplanocin A (DZNep), an S-adeno- sylhomocysteine hydrolase inhibitor, and/or pan-histone deacetylase inhibitor panobinostat (PS) on cultured and primary MCL cells. Experimental Design: Following treatment with DZNep and/or PS, apoptosis and the levels and activity of EZH2 and PRC2 proteins in cultured and primary MCL cells were determined. Results: Treatment with DZNep depleted EZH2, SUZ12, and 3MeK27H3 in the cultured human MCL cells. DZNep also increased expression of p21, p27, and FBXO32, whereas it depleted Cyclin D1 and Cyclin E1 levels in MCL cells. In addition, DZNep treatment induced cell-cycle arrest and apoptosis in cultured and primary MCL cells. Furthermore, as compared with treatment with each agent alone, cotreatment with DZNep and PS caused greater depletion of EZH2, SUZ12, 3MeK27H3, and Cyclin D1 levels, whereas it induced greater expression of FBXO32, p16, p21, and p27. Combined treatment with DZNep and PS synergistically induced apoptosis of cultured and primary MCL cells while relatively sparing normal CD34 þ cells. -

A Substitution Mutation in Cardiac Ubiquitin Ligase, FBXO32, Is Associated with an Autosomal Recessive Form of Dilated Cardiomyopathy Zuhair N
Al-Hassnan et al. BMC Medical Genetics (2016) 17:3 DOI 10.1186/s12881-016-0267-5 RESEARCH ARTICLE Open Access A substitution mutation in cardiac ubiquitin ligase, FBXO32, is associated with an autosomal recessive form of dilated cardiomyopathy Zuhair N. Al-Hassnan1,2,7,8*, Zarghuna MA. Shinwari1, Salma M. Wakil3, Sahar Tulbah1, Shamayel Mohammed4, Zuhair Rahbeeni2, Mohammed Alghamdi4, Monther Rababh1, Dilek Colak5, Namik Kaya3, Majid Al-Fayyadh1,6 and Jehad Alburaiki6 Abstract Background: Familial dilated cardiomyopathy (DCM) is genetically heterogeneous. Mutations in more than 40 genes have been identified in familial cases, mostly inherited in an autosomal dominant pattern. DCM due to recessive mutations is rarely observed. In consanguineous families, homozygosity mapping and whole exome sequencing (WES) can be utilized to identify the genetic defects in recessively inherited DCM. Methods: In a consanguineous family with four affected siblings with severe DCM, we combined homozygosity mapping, linkage analysis and WES, to uncover the genetic defect. Results: A region of homozygosity (ROH) on chromosome 8q24.13–24.23 was found to be shared by all of the four affected siblings. WES detected ~47,000 variants that were filtered to a homozygous mutation (p.Gly243Arg) in the FBXO32 gene, located within the identified ROH. The mutation segregated with the phenotype, replaced a highly- conserved amino acid, and was not detected in 1986 ethnically-matched chromosomes. FBXO32, which encodes a muscle-specific ubiquitin ligase, has been implicated in the pathogenesis of cardiomyopathy through the ubiquitin proteasome system (UPS). In addition, FBXO32-knockout mice manifest with cardiomyopathy. Screening the index patient for all of the WES variants in 48 genes known to be implicated in hypertrophic and dilated cardiomyopathy was negative. -

Polyphagia Ellen N
W0117-Section I (31-50).qxd 4/23/04 7:26 PM Page 124 CHAPTER • 34 Polyphagia Ellen N. Behrend olyphagia is the consumption of food in excess of and liver disease) lead to polyphagia by unknown mecha- normal caloric intake. Hunger and satiety and, conse- nisms. Secondary polyphagia can also be caused by certain P quently, feeding behavior are primarily controlled by drugs. certain regions in the central nervous system (CNS), but many factors affect the function of these areas. Thus polypha- gia can be classified as primary (i.e., a CNS abnormality) or HISTORY secondary (i.e., a systemic problem affecting the CNS). Secondary polyphagia is by far more common and usually is Any change in body weight is an important differentiating accompanied by clinical signs of the underlying disease. feature of the various causes of polyphagia (Figure 34-1). Determining whether weight gain or loss has occurred should Primary or drug-induced polyphagia typically results in weight be the first step in formulating a list of differential diagnoses gain, because nutrients are adequate and feeding is inappro- and a diagnostic plan. priately increased. Pathologic secondary polyphagia is more commonly associated with weight loss, because the nutrient supply usually does not meet physiologic demands. However, PHYSIOLOGY some causes, such as acromegaly, hypoglycemia caused by an insulinoma, sudden acquired retinal degeneration syndrome Food intake is controlled by a variety of factors, including gas- (SARDS), and hyperadrenocorticism (HAC), lead to weight trointestinal, environmental, and CNS phenomena. The CNS, gain. Physiologic polyphagia can result in weight gain (e.g., mainly the hypothalamus, controls eating behavior.The lateral pregnancy, growth) or maintenance of weight (e.g., lactation, hypothalamic nuclei represent the “feeding center”; their cold environment, increased exercise). -

Sudden Death in Eating Disorders
Vascular Health and Risk Management Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Sudden death in eating disorders Beatriz Jáuregui-Garrido1 Abstract: Eating disorders are usually associated with an increased risk of premature death Ignacio Jáuregui-Lobera2,3 with a wide range of rates and causes of mortality. “Sudden death” has been defined as the abrupt and unexpected occurrence of fatality for which no satisfactory explanation of the 1Department of Cardiology, University Hospital Virgen del Rocío, 2Behavioral cause can be ascertained. In many cases of sudden death, autopsies do not clarify the main Sciences Institute, 3Pablo de Olavide cause. Cardiovascular complications are usually involved in these deaths. The purpose of University, Seville, Spain this review was to report an update of the existing literature data on the main findings with respect to sudden death in eating disorders by means of a search conducted in PubMed. The most relevant conclusion of this review seems to be that the main causes of sudden death in eating disorders are those related to cardiovascular complications. The predictive value of the For personal use only. increased QT interval dispersion as a marker of sudden acute ventricular arrhythmia and death has been demonstrated. Eating disorder patients with severe cardiovascular symptoms should be hospitalized. In general, with respect to sudden death in eating disorders, some findings (eg, long-term eating disorders, chronic hypokalemia, chronically low plasma albumin, and QT intervals .600 milliseconds) must be taken into account, and it must be highlighted that during refeeding, the adverse effects of hypophosphatemia include cardiac failure. -
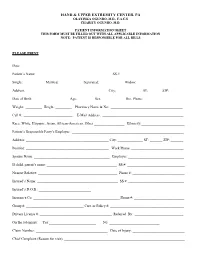
Patient Information Sheet This Form Must Be Filled out with All Applicable Information Note: Patient Is Responsible for All Bills
HAND & UPPER EXTREMITY CENTER, PA OLAYINKA OGUNRO, M.D., F.A.C.S CHARITY OGUNRO, M.D. PATIENT INFORMATION SHEET THIS FORM MUST BE FILLED OUT WITH ALL APPLICABLE INFORMATION NOTE: PATIENT IS RESPONSIBLE FOR ALL BILLS PLEASE PRINT Date: ________________________________________ Patient’s Name: _________________________________________ SS #: __________________________________ Single: __________ Married: ___________ Separated: ___________ Widow: ____________ Address: _____________________________________________ City: _____________ ST: ______ ZIP:________ Date of Birth: ___________________ Age:_________ Sex: ____________ Hm. Phone: ______________________ Weight: _________ Height: _________ Pharmacy Name & No: ________________________________________ Cell #: ___________________________ E-Mail Address: _____________________________________________ Race: White, Hispanic, Asian, African-American, Other _________________ Ethnicity:________________________ Patient’s Responsible Party’s Employer: ______________________________________________________________ Address: ______________________________________________ City: ______________ ST: _______ ZIP: _______ Position: ______________________________________________ Work Phone: _____________________________ Spouse Name: __________________________________________ Employer: _______________________________ If child, parent’s name: _______________________________________ SS #: ________________________________ Nearest Relative: ____________________________________________ Phone #: _____________________________ -

Unusual Case of Necrotizing Pneumonia Rajapriya Manickam*, Kabir Oladipo Olaniran and Raghu Loganathan
Manickam et al. Int J Respir Pulm Med 2015, 2:2 International Journal of ISSN: 2378-3516 Respiratory and Pulmonary Medicine Case Report : Open Access Unusual Case of Necrotizing Pneumonia Rajapriya Manickam*, Kabir Oladipo Olaniran and Raghu Loganathan Division of Pulmonary and Critical care Medicine, Lincoln Medical and Mental Health Center, USA *Corresponding author: Rajapriya Manickam, Division of Pulmonary and Critical care Medicine, Lincoln Medical and Mental Health Center, Bronx, New York, USA, Tel: 917-375-5626; E-mail: [email protected] Abstract Coccidioidomycosis is caused by inhalation of Coccidoides spores which is endemic in south western parts of USA and an uncommon cause of pneumonia in non-endemic areas. We report a young Hispanic man who lives in New York presenting with diabetic ketoacidosis and severe pulmonary Coccidioidomycosis. Through this case report and review we want to familiarize clinicians from non-endemic area to this unusual cause for necrotizing pneumonia, its association with diabetes mellitus, other risk factors for dissemination and the management strategy. Introduction Pulmonary Coccidioidomycosis is an uncommon cause of necrotizing pneumonia in non-endemic areas. We report a case of severe pulmonary Coccidioidomycosis in a young immigrant who lives in New York and discuss the association with diabetes mellitus. Hospital Course A young 32 year old Hispanic man presented with 4-weeks history of polyuria, polyphagia and weight loss and 2-weeks history Figure 1: Chest radiograph showing right upper lobe consolidation and of hemoptysis and shortness of breath. He denied fever, chills, night retraction of horizntal fissure. sweats, sick contacts, skin rash, glandular swelling or recent travel. -

Pharmacovigilance - Post
PHARMACOVIGILANCE - POST MARKETING SURVEILLANCE NEWS Vol. 7 No. 3: Third Quarter Newsletter 2014 Editor’s Note I wish to thank all our numerous stakeholders who have been working tirelessly with the National Pharmacovigilance Centre (NPC) to ensure the safe use of medicines in Nigeria. The NPC is committed to sending quarterly newsletter to its stakeholders. The objectives of the Newsletter are to disseminate information on pharmacovigilance activities nationally and globally, to educate stakeholders on medicine safety issues, to promote rational use of drugs and to promote spontaneous reporting. This third quarter Newsletter focuses on Pharmacovigilance of Antidiabetic Drugs. We encourage all Health Care Professionals, Marketing Authorization Holders and other stakeholders to continue to report all adverse drug reactions. Your valued comments and acknowledgement of receipt of this issue through our email addresses ([email protected]; pharmacovigilance@nafdac,gov.ng ) would be most appreciated. Pharm. (Mrs.) Osakwe Director/NationalCoordinator, National Pharmacovigilance Centre (NPC) National Agency for Food and Drug Administration and Control (NAFDAC) Plot 2032 Olusegun Obasanjo Way Wuse Zone 7 Abuja PMB 5032 Wuse Abuja. Telephone 07098211221, 08086899571 E-mail: [email protected]; [email protected]; [email protected]; Website :www.nafdac.gov.ng Text any DRUG RELATED PROBLEM to SHORT CODE 20543 (for free on MTN, GLO and Etisalat) for action by the Pharmacovigilance Centre 1 PHARMACOVIGILANCE OF ANTIDIABETIC DRUGS Diabetes is one of the major causes of illnesses and deaths globally, and it affects many regardless of age or race. This disease can contribute to other health complications such as heart disease, kidney disease and blindness if not properly treated. -

The Basics of Pharmacology
THE BASICS OF PHARMACOLOGY Endocrine, Musculoskeletal, Genitourinary, Ear And Eye Systems Jassin M. Jouria, MD Dr. Jassin M. Jouria is a practicing Emergency Medicine physician, professor of academic medicine, and medical author. He graduated from Ross University School of Medicine and has completed his clinical clerkship training in various teaching hospitals throughout New York, including King’s County Hospital Center and Brookdale Medical Center, among others. Dr. Jouria has passed all USMLE medical board exams, and has served as a test prep tutor and instructor for Kaplan. He has developed several medical courses and curricula for a variety of educational institutions. Dr. Jouria has also served on multiple levels in the academic field including faculty member and Department Chair. Dr. Jouria continues to serve as a Subject Matter Expert for several continuing education organizations covering multiple basic medical sciences. He has also developed several continuing medical education courses covering various topics in clinical medicine. Recently, Dr. Jouria has been contracted by the University of Miami/Jackson Memorial Hospital’s Department of Surgery to develop an e- module training series for trauma patient management. Dr. Jouria is currently authoring an academic textbook on Human Anatomy & Physiology. ABSTRACT The science of pharmacology and the responsibility relationship building with patients are important elements of a health professional’s clinical knowledge and skills to provide safe and appropriate pharmacotherapeutic regimens in everyday practice. Interdisciplinary members of the health team are required to continually interpret specific patient health data to implement and evaluate outcomes of medication treatment. All health clinicians are increasingly relying on practice guidelines and the applied specialized training of health team members when obtaining the patient health history to improve therapeutic medication regimens, avoid adverse effects, and to safely and effectively treat a disease state. -

Partial Target Organ Resistance to Thyroid Hormone
Partial Target Organ Resistance to Thyroid Hormone Hans Henning Bode, … , Farahe Maloof, John D. Crawford J Clin Invest. 1973;52(4):776-782. https://doi.org/10.1172/JCI107240. Research Article An 8-year old boy with a small goiter, normal basal metabolic rate (BMR), and elevated serum thyroid hormone levels (thyroxine [T4] 19.5 μg per 100 ml, free T4 4 ng per 100 ml, triiodothyronine [T3] 505 ng per 100 ml) was studied. He had measurable serum thyroid-stimulating hormone (TSH) levels (average 5.5 μU per ml), and the thyroxine-binding proteins, hearing, and epiphyseal structures were normal. There was no parental consanguinity nor were there thyroid abnormalities either in the parents or six siblings. Methimazole, 50 mg daily, depressed thyroxine synthesis (T4 10.5, free T4 2.5) and caused a rise in TSH to 11 μU per ml. After discontinuation of treatment, TSH declined to 4.2 μU per ml and chemical hyperthyroidism returned (T4 21.0 μg per 100 ml, free T4 4.2, and total T3 475 ng per 100 ml, radioactive iodine [RAI] uptake 68%), but studies of BMR and insensible water loss showed the patient to be clinically euthyroid. Thyrotropin-releasing hormone (TRH), 200 μg i.v., caused a brisk rise in TSH to 28 μU per ml, with T4 rising to 28 μg per 100 ml, free T4 to 5.6, and T3 to 730 ng per 100 ml, thus indicating that the pituitary-thyroid system was intact and that the patient's TSH was biologically active. The unusual sensitivity of the pituitary cells to TRH […] Find the latest version: https://jci.me/107240/pdf Partial Target Organ Resistance to Thyroid Hormone HANS HENNING BODE, MARco DANON, BRUCE D.