Gastrectomy). Timed Collections of Urine and Ileostomy Discharge Were
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Marathon Championship
CLUB KIWIFRUIT FUND RAISING PICK As reported in Ramblings newsletter, 6th June, 1992. The annual Shallcross kiwifruit pick was once again offered to Tauranga Ramblers to give our funds a much needed boost so that we can subsidise club days, Bar-B-Q’s, Pinto, buses, newsletters and travel to major events. All in all club members receive more than their subscriptions cover, therefore we need full support from all participants for our fund-raising efforts. The club is very appreciative of the chances to earn this money and a special thanks go to Bill and Marge Shallcross for this fruit picking opportunity. It certainly beats selling raffle tickets and gives us the chance to do something other than one’s usual job or studies. It is quite an education especially the way different people see the hairy berries – their shapes and sizes I’ll leave to your imagination. Colin Clifton commented that it was a change from working alone. Teresa Coston was certainly the noisiest and Kristin McLoughlin one of the quietest, but it was good to see everyone turn out. Some brought their spouses, or sons and daughters. Robyn Bint did a great job removing all the kiwifruit stalks. Marge did a great job of keeping the team fed, while Nigel Hines had done an absolutely fantastic job chasing along all members he could find. Over the two days we picked 162 bins compared to 166 last year. Unfortunately we couldn’t quite finish but Ramblers received $1400.00 for the two day’s work. Once again special thanks to Bill, Marge, Debbie, Russell, Rob Shallcross and his in-laws and to Nigel and Sheryl Hines for their organisation. -

For Runners Aiming 55 to 75 & 80 to 100 Miles/Week
For runners aiming 55 to 75 & 80 to 100 miles/Week PrePared by mike gratton, 1983 london marathon Winner hese schedules are aimed at runners who have so that marathon endurance is established before specific already reached a high level of training background speed work brings you to a peak. Maximum mileage will Tand have been regularly training at up to 50 miles thus be reached 2 months before the Marathon; once or above per week for the last 6 months to 1 year. Many this is achieved the aim is then to make you faster while will probably have run a marathon already, but not maintaining the endurance base. For explanation on necessarily. The aim is to establish long runs fairly early on terminology used see Notes for 2:09 Events training Plans Week 1 55-75 Miles per Week 80-100 Miles per Week WEDNESDAY 1 hr 30mins steady Am: 45mins easy/ Pm: 1 hr 30mins SUNDAY 2 hrs steady 2 hrs steady THURSDAY 1 hr steady Am: 45mins easy/ Pm: 1 hr steady MONDAY Tempo – 45mins @ marathon pace Am: 45mins easy/ Pm: 1 hr steady FRIDAY 45mins easy Am: 45mins easy/ Pm: 45mins easy TUESDAY Am: 30mins easy/ Pm: 20 x 300m/100m jog rec Am: 45mins easy/ Pm: 5 sets of 5 x 300m/100 jog – SATURDAY 1 hr steady Am: 1 hr steady/ Pm: 1 hr steady @ 10km pace 5 mins between sets @ 5 km pace Week 8 55-75 Miles per Week 80-100 Miles per Week WEDNESDAY 1 hr 20mins steady Am: 45mins easy/ Pm: 1 hr 30mins steady SUNDAY 2 hrs 30mins steady Am: 2 hrs 30mins steady/ Pm: 30mins easy THURSDAY Am: 30mins easy/ Pm: 30mins @ threshold pace + 8 Am: 40mins easy/ Pm: 30mins @ threshold -

Moulsham Junior School Past Pupils' Newsletter
Moulsham Junior School Past Pupils’ Newsletter Autumn 2015 Vol 17 no 2 In this issue page Welcome to the Autumn Newsletter 2 From Head Teacher Mrs Marie Staley 3 Date of the 2016 Open Afternoon 4 School website 4 Deliveries of the printed Newsletter 4 Open Afternoon 2015 5 Ray Sewell 1939 9 From the 1950s: Chelmsford Carnival photo from Jennifer Bailey (Rayner); 11 News from David Buckle, 1950s Photos of Mrs Balaam / Brooks’ classes in the 1970s and 80s 12 Peter Turrall’s talk on Old Chelmsford, 4 June 2015, with pictures 13 More about Chelmsford cinemas: Maureen Rignall ( Bidwell) 1941; 16 Jennifer Bailey (Rayner) 1943; Peter C Smith 1938; and Doug Fawcett 1938 Mrs Linda Hughes: Memories of teaching sport 19 Les Kemp: Sweet rationing 20 From the 1960s: Paul Matthams 21 News in brief: Mick Ford, 1940s, David Tarbun, 1940 22 Hazel Richards (Offord), 1951, Alex Hassell Obituaries: 23 Mrs Jean Roberts, Mrs Pat Sturgeon (Purdie), Jean Allen (Sprawling), Tony Woollett, Maureen Biggins (Little), Anne Tenneson (Rowse), Mary Allan (Calver), Eric Hayward Data protection legislation 28 1 Welcome to the Autumn Newsletter Welcome to the Autumn 2015 Newsletter, and thank you to all those who have sent in recollections, photos and news for this issue. As usual, we have an interesting blend of articles from past pupils and staff. In addition, on page 3, the present Headteacher Mrs Marie Staley updates us on current school news, including the building of an extension to accommodate more pupils as the city of Chelmsford continues to expand. She has included seven photos of the building work at different stages. -

Victorian Marathon Club Newsletter
VMC ROAD RUNNERS SEPTEMBER 1984 NEWSLETTER PRICE $1.00 BARBARA FAY Sub 3 hour Veteran Marathoner and regular V.M.C.R.R. pace setter enjoying pre-race atmosphere around Melbourne’s “Tan” circuit. Registered by Australia Post Publication No. VBH 0488 VoMoCoNEWSLETTER SPRING 1 ^ 8 4 SEPTEMBER VOL.16 No. 2 THE VMC ROAD RUNNERS NEWSLETTER is published for the information of members of the VMC ROAD RUNNERS CLUB and is covered by p a y m e n t of the Annual Membership Pee. It is issued four times a year* SPRING (September) SUMMER (December) AUTUMN (March) WINTER (June). All athletes, irrespective of age or sex, are invited to contribute letters, results, comments, criticisms, etc0, to the Editor, 1 Golding St, CANTERBURY, Vic. 3126. PLEASE NOTE that material submitted for publication should be on single-spaced, typed A4 sheets, irrespective of length, to facilitate layout. Articles should not eatceed one and a half pages of A4 , preferably half that. Articles for publication MUST BE accompanied by the name and address of the contributor, together with his or her signature. The author of the article shall retain full responsibility for the content of such article. DEADLINE FOR COPY is the 10th day of the month preceding the month of publication, we ask controbutors to aim for the 1 st day of that month to make editing less rushed. ★******************************************** INTERSTATE LINES OF COMMUNICATION : AAU* Rick PANNELL, Olympic Park No.1, Swan St, MELBOURNE 3002 429 50 77 NSW AAA: Clive LEE, PO Box N101, Grosvenor Stf SYDNEY 2001 241 -
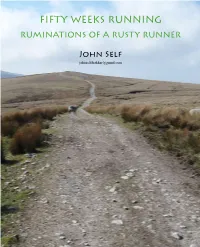
Fifty Weeks Running Ruminations of a Rusty Runner
FIFTY WEEKS RUNNING RUMINATIONS OF A RUSTY RUNNER John Self [email protected] THE RUN-UP January 1st 2011 hy? Why do we ask ‘Why?’? Arctic terns fly over One thing that I do know about running is that W 40,000 miles a year; the Dracunculus vulgaris no runners run all day, every day. Even for the most plant smells of rotting flesh; North American cicadas fanatical runner, running can occupy only a small have a life cycle of 13 or 17 years. But they do not ask fraction of a runner’s time. For the large majority of ‘Why?’. We ask ‘Why?’ of them. runners, their non-running activities are much more We also ask ‘Why?’ of each other, if we come important than their running. The answer to my across some apparently strange behaviour: Why does conundrum lies, perhaps, in the relationship between he wear a bow-tie every day? Why does she sing running and the rest of life. We shall see, perhaps. arias while gardening? Why does he collect Bulgarian I plan to write a thousand words or so each week stamps? If we feel bold, we might even ask the person about my running, with no doubt a few detours and directly. Rather more puzzlingly, we also ask ‘Why?’ of perhaps hiatuses along the way, as there are with my ourselves. Why do I continue to support Norwich City running. In the past I have always found it better to Football Club, despite decades of little achievement write an introduction such as this after I have written (that is, the football club, not me)? You would think that, what needs to be introduced (I have a slightly better if someone did something of their own volition, they idea what it’s about by then). -

The Daily Egyptian, October 24, 1984
Southern Illinois University Carbondale OpenSIUC October 1984 Daily Egyptian 1984 10-24-1984 The aiD ly Egyptian, October 24, 1984 Daily Egyptian Staff Follow this and additional works at: https://opensiuc.lib.siu.edu/de_October1984 Volume 70, Issue 48 Recommended Citation , . "The aiD ly Egyptian, October 24, 1984." (Oct 1984). This Article is brought to you for free and open access by the Daily Egyptian 1984 at OpenSIUC. It has been accepted for inclusion in October 1984 by an authorized administrator of OpenSIUC. For more information, please contact [email protected]. CIA orders recall of all copies of rebel manual WASHINGTON ' AP ) - The CIA offl c.ab Monday nigh!. A tradi tiona l guidelines of war. were made from the origi nal references to such Violent acts CI A has ordered a "full rpcall" ' com mitt ee sou rce said the ('IA The committ ee source, who manual produced last October, "some way ". got out day. n of Its ('ontro\'crsla) manual for also mention\.'<i the r('Call of all Insisted on anonymity. said tht' but that a ll editions - including there .. ~Icarasua n rel>t"l!' and IS asking cf'pi es during a three·hour agency was trying to recover o ne a p proved a t CIA Ihat its content s , mclud ing briefing of the panel earlier s. c\lcralthousand prin ted copies headqua rters - conta ined Reagan sa.d the origina l ad\'lcc on "se)ectl\'(' usc of Monda\, . of three' versions of the ma nu al. references to using violence to man ual wa s the work of a CIA nolencc" to " neul raliz(''' Leah'" said the CIA. -

Marathon Training Mike Gratton London Marathon Winner 1983 Background
MARATHON TRAINING MIKE GRATTON LONDON MARATHON WINNER 1983 BACKGROUND • 1967: British Forces Schools 800m – 2nd 2:10 / age 13 • 1970: English Schools Inter 1,500m – 7th 4.07 /age 15 • 1974: English Schools Senior 5,000m – 1st 14.35 / age 18 • 1979: First Marathon – Paris – 11th – 2.21 • 1979: Second Marathon – Windsor – 1st - 2.19 • 1980: Olympic Trials Marathon – Milton Keynes – 11th 2.17 • 1981: National Marathon Champs – Rugby – 3rd – 2.16 • 1982: National 20 Miles Champs – 1st – 1.42 • 1982: London Marathon – 3rd – 2.12.30 • 1982: National 10 miles Champs – 1st 47.40 • 1982: Commonwealth Games Brisbane – bronze – 2.12.06 • 1983: London Marathon – 1st – 2.09.43 • 1991: Final Marathon – 7th – Cleveland Ohio – 2.17 In 1982 there was a big improvement WHY WAS THIS • Up to 1979 training was mostly geared towards 10km and Cross Country. Although regularly running 20miles on a Sunday the focus was on Interval Running. • After the Olympic trials in 1980 where I was close to making the GB team I decided to focus more on endurance and increased mileage up to 140 Miles week • In 1981 I was exceptionally fit but running marathons tired – I ran the Kosice Marathon in Czechoslovakia and set out at 2.12 pace but fell apart in the last 5 miles and finished with 2.24 • In winter of 1981 I dropped the mileage to 115 to 120 per week – still a lot but left me with more energy in races What Did a Week Look Like Sun: am: 22 Miles pm: 5 Miles Mon: am: 5 Miles pm: 3 Mile warm up/Hill session/3 Mile warm down Tue: am 5 Miles pm: Track endurance – 20 x 400m/100m -

December 1982
•- ^ HIGHLIGHTS^ THE ATHlFncS —New York Marathon -Avon Half-Marathon —Masters/Women Mythical Meet -V World Games Update I —1982 Postal One-Hour Run -Tulsa 15K —Chile Senior T&FChampionships -TAC Convention Preview —Run Against Crime 15K -North American Masters T&F —Twin Cities Marathon -Photos, letters, profiles it —National 30K -Lynchburg lOK —Skylon Marathon -Eastern Masters X-C —New Age Records -Columns by Tymn, Conley, Miller, m —San Juan T&F Championships -Japan Masters T&FChampionships -1983 T&F Schedule Higdon, Farquharson —U.S. Masters go to China -Nike Capital Challenge I —National Masters 15K —And much more i ^ National Masters News The onlynationalpublication devoted exclusively to track &field and longdistance running for men and women overage 30 52ii(l Issue December, 1982 $1.25 Higdon, Stock Set I5K Marks VILLANUEVA,DALRYMPLE WIN IN NEW YORK } r- Villanueva, Matson 4,406 Masters Among ,i- Take El Paso Titles 14,000 Marathoners by RICHARD LEE SLOTKIN NEW YORK, N.Y., October 24. While the ABC-TV network cameras EL PASO, Texas, October 9. This were focusing on the leaders in the was the second annual running of the 3-hour, nationally televised New York Run Against Crime 15K, but with a Marathon today, some of the finest difference: this year, they went big masters runners in the world were wag time. How big? Well, Frank Shorter ing a duel of their own less than 10 finished 28th, that's how big. minutes back. Midway between men's winner It was billed as an international Alberto Salazar (2:09:29) and women's event, and it filled the bill in every winner Grete Waitz (2:27:14), Mex sense. -

Keep Injury at Bay Expert Advice the Need for Speed
TRAINING GUIDE EXPERT ADVICE KEEP INJURY AT BAY THE NEED FOR SPEED RULES OF HYDRATION FUEL YOUR RECOVERY THE ELITES’ TOP TIPS GET THE MOST OUT OF YOUR RUNNING AW TRAINING GUIDE WELCOME AND CONTENTS @ATHLETICSWEEKLY GETTY IMAGES FOR BRITISH ATHLETICS GETTY IMAGES SHUTTERSTOCK 20 12 CONTENTS A GUIDE TO 6 IT’S TIME TO GO TO ‘PREHAB’ KEEP YOU The exercises which will make you stronger 12 HOW TO POWER ON TRACK YOUR RECOVERY IT’S AROUND this point of the year when you’ll hear the question ‘how’s your training Getting your post-run nutrition going?’ being asked most keenly. right will pay dividends It may be just a few short weeks since the bells brought in 2018 but already there 18 HOW MUCH will be schedules which are going perfectly HYDRATION IS RIGHT? to plan and others which might not be We look at the amount of fluid following the desired script. you should be aiming to take on For ultra marathon runners, marathon runners, those aiming for 20 THERE IS A 5k, 10k, half-marathon PBs or others with track ambitions weighing heavily on their NEED FOR SPEED shoulders, this is where the really hard MARK SHEARMAN Why your running will benefit work is being done ahead of the big events 28 from upping the pace or ‘A’ races to come. With that in mind, we thought we’d 24 ELITE ADVICE present you with some advice and, Britain’s finest offer their hopefully, inspiration, in the form of this top training tips Training Guide to help keep you going as you log the miles and the sessions. -

IA Journal 200.Indd
ISSUE 200 SUMMER 2008 www.iasupport.org Quarterly Journal of IA issue The Bryan Brooke Lecture 2008 The IA200 Journal through the Ages Stoma problems - how common are they, A commemorative article for our 200th and what can we do to avoid them? issue Colitis and Ileostomy - Before and After Coming to Terms with a New Plumbing System This member’s experiences did not prevent Over 10 years with an internal pouch, and him taking part in the ‘3 peaks challenge’ very happy with it IA JOURNAL SUMMER 2008 From the editor John Smail A warm welcome to this I am pleased to say that members continue to 200th issue of the IA send in stories about their personal Journal. It is thanks to experiences, which others can share and learn all those pioneers in the from. On page 48 there is a story from a early days of ileostomy member who has over ten years experience surgery back in the 1950s, with his internal pouch and is very happy with and the work of countless it, and on page 54 there is a story from another supporters ever since, that we have reached member whose life with his family improved this significant landmark. dramatically following ileostomy surgery. In addition we have several other interesting In this edition, I have written a few pages on the articles and another excellent selection of history of the IA Journal which I hope you will readers’ letters. I would encourage members find interesting, including some illustrations of to respond to these letters either directly with our Journal in its earlier years. -

Marathon Training
ENDURANCE TRAINING By Mike Gratton 1983 London Marathon Winner WHAT ARE THE DEMANDS OF MARATHON RUNNING? You have to run for more than 2hrs Your energy reserves will become depleted In some races you will have up to 50,000 other runners in your way In some races you will have to run on Your own for a long way How do you prepare the body for such great demands? Recognise the demands of the event and build up steadily and systematically so that your body adapts gradually to these demands Your training should build over 12 to 16 weeks to gradually get close to the intensity of the marathon itself This means starting with a low level of intensity in your training – which is often called ‘base training’ - and then over time, running longer and faster as you get close to race day There may be different starting points depending on your running background: Established runners can build up the long run at the start of their training block and gradually increase the speed of the run towards race day Runners with some running back ground can build up the long run fairly quickly over the first half of the block then increase the speed towards race day Beginners will concentrate on gradually building up the length of the long run towards race day. YOUR LONG RUNS Build Endurance Cause adaptations to bones, muscle and cardio vascular system Develop energy systems and promote fat burning How far depends on your fitness levels – base on time rather than distance with optimal target of 2 to 2.5hrs CONSISTANCY IS THE KEY Frequency of training has been shown to be the most important factor in developing fitness. -

Feared Victim Cromword Ce ~Ost Death Notlcu 88 Opppse Tax Cut
' 'Have ihey caug im?' Protopappas sentenced to 15 years yROBERT AR s dnvsn nd h ve become Of IM DdJ f'lltf ltaft hysterical ByJEFF OLER 0 Parent , school nd police re 1'he kid re really fnnd." OlllleO.-, ......... tightenina unty measures to ad Shelly Repsher. n p rent of form r CC)$.t Mc d n11 Tony protect scltool children followmg two )'9ung daughters whO alt nd ProtopapPf wa scnt ctd to three three rooent all~d k1dnappmg Kettler Elementary School at concurre t 1~ year to hfe pnson attempt in Huntanston Bench. 8750 Dorsen Drive, •• nd the terms Monday for the anesthesia· In some instances, keen ~r marents are concerned ·· overdose killings of three paucnts m ent I concem - ifnot fear - has R~her, who J>reviou ly ha 1982-and 1983. e calated in neighborhood , ac been able to stand in front of her The sentence, pronounced by Or· cotding to parents. Some young- home and watch as her daughters anit County Superior Coun Judge 5ters reportedly h ve see" a car walked to school, has uined L.u1 Cardena following 1 da)-long similar to on older model green walking them 10 nd from the sentencao=na m the Santa Ana ............................ Chevrolet the suspect nll~dly (Pleue Me l"EAR/A2) (P eee DEKTISTI A2) Vlctim'e ltln 111& JKken &11d Dlo~ IDwat ........ Forecaate on A2. COAST IDlllDN - TUESDAY OCTOBER 23. 1984 ORANGF C OUNTY C A LI FORNIA :?5 CENT S Coast crashesI · kill woman, tot injuries she suffered when her car was Bradley said Ramsey, drivjng a to the hospital as a precauuon, m tly unrestra10ed in :the passenger &eat of • 'Minor injuries' claim Newport victim; broadsided in a Corona '"del Mar 1977 (.:tJc,.·rolet, was not wearing a be<::ause ofher aie.