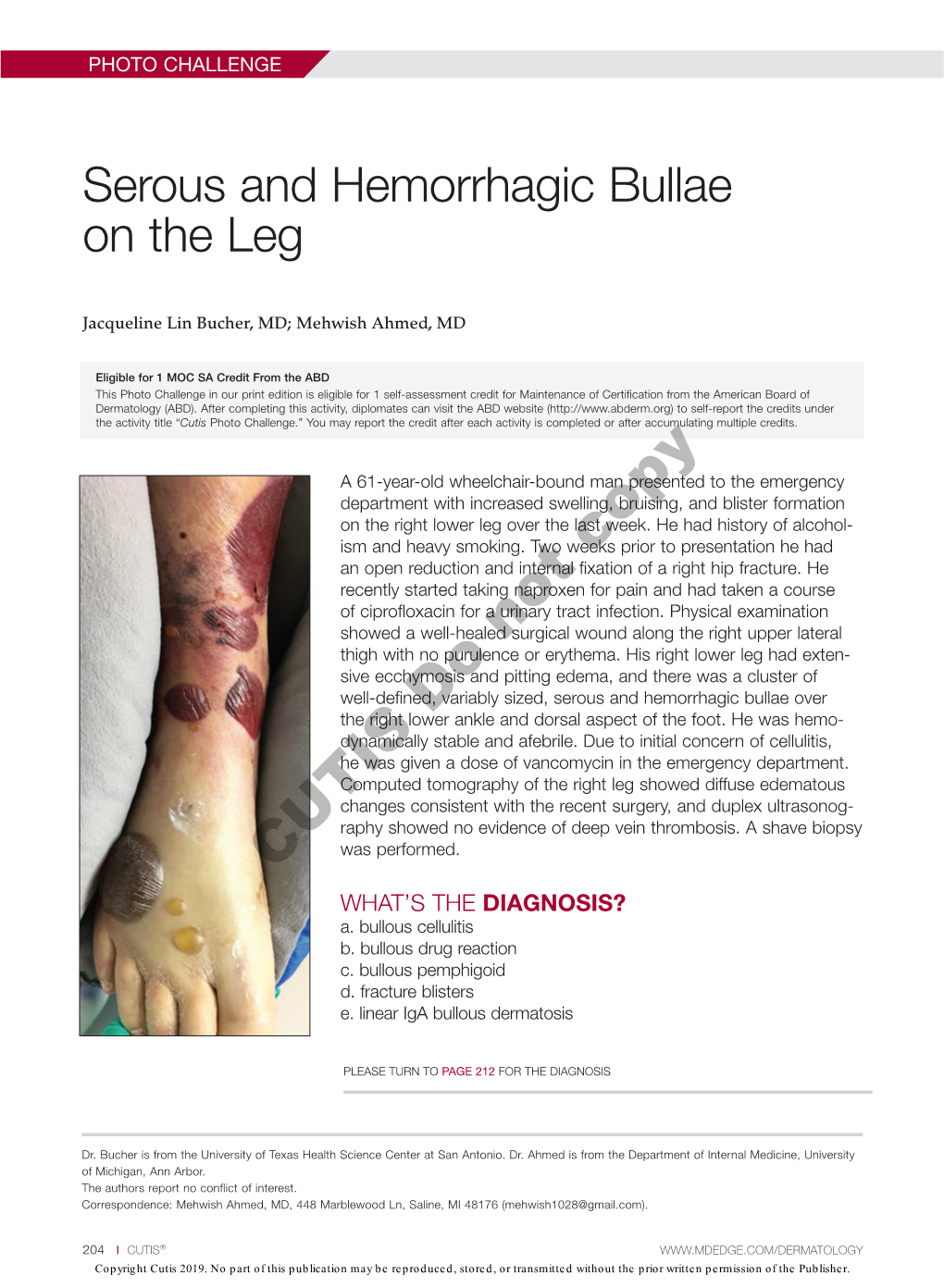
Serous and Hemorrhagic Bullae on the Leg
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Case of Bilateral Calcaneal Fracture, Following Fall from 35 Feet
rauma & Sastry et al., J Trauma Treat 2015, 4:3 f T T o re l a t a m DOI: 10.4172/2167-1222.1000254 n r e u n o t J Journal of Trauma & Treatment ISSN:ISSN: 2167-1222 2167-1222 CaseResearch Report Article OpenOpen Access Access A Case of Bilateral Calcaneal Fracture, Following Fall from 35 Feet Purushothama Sastry, Sujana Theja JS, Supreeth N and Arjun Markanday* Department of Orthopaedics, JSS Hospital, Mysore, India Abstract Introduction: Called Lover’s Fractures, the calcaneus commonly fractures due to fall from height. The calcaneus is the most frequently fractured tarsal bone. Tarsal bone fractures account for about 2% of all adult fractures. Of these, 60% are calcaneus fractures.The heel bone is often injured in a high-energy collision where other parts of the skeleton are also injured. In up to 10% of cases, the patient can also sustain a fracture of the spine, hip, or the other calcaneus. Injuries to the calcaneus often damage the subtalar joint and cause the joint to become stiff. This makes it difficult to walk on uneven ground or slanted surfaces. Case Report: A 24 year old male, working as a lift operator presented to the casualty of the hospital after the elevator broke down and came down in a free fall from about a height of 4 stories (35 feet). He presented along with the other occupants of the lift who also sustained calcaneal fractures.The case on arrival was subjected to ATLS protocol and through radiologic work up was done. Following a period of 12 days post trauma he was operated for bilateral calcaneal fractures and discharged 10 days post operatively. -

Deep Tissue Injury
Deep Tissue Injury Overview Deep tissue injury is a term proposed by NPAUP to describe a unique form of pressure ulcers. These ulcers have been described by clinicians for many years with terms such as purple pressure ulcers, ulcers that are likely to deteriorate and bruises on bony prominences (Ankrom, 2005). NPAUP’s proposed definition, is “A pressure-related injury to subcutaneous tissues under intact skin. Initially, these lesions have the appearance of a deep bruise. These lesions may herald the subsequent development of a Stage III-IV pressure ulcer even with optimal treatment.”(NPAUP, 2002). Why is it important to have another label for pressure ulcers? Aren’t four stages enough? Perhaps not, because deep tissue injury represents a dangerous lesion due to its potential for rapid deterioration. Proper labeling will afford clinicians a more accurate diagnosis, and lay a foundation for the development of efficacious interventions. Background Shea (1975) is often credited with labeling the stages of pressure ulcers, and his descriptions of four depths of ulcers were adapted by IAET, AHCPR, and NPUAP. Missing from that four stage system label is deep tissue injury. However, Shea did not forget them in his review. He described ulcers that appear innocent yet conceal a deep, potentially fatal lesion. In 1873 Paget may have been the first to describe deep tissue injury describing purple areas with sloughing of tissue and large cavities once they open. In 1942, Groth created deep, “malignant pressure sores” in an animal model in a series of experiments that began in deeper tissues and spread to the surface. -

Staged Management of Tibial Plateau Fractures
A Review Paper Staged Management of Tibial Plateau Fractures Douglas R. Dirschl, MD, and Daniel Del Gaizo, MD also warrant staged management because of patient, soft tissue, ABSTRACT or biologic factors. A low-energy injury in a patient with com- Careful and thorough assessment of injury severity, promised physiology (uncontrolled diabetes, smoking, morbid with particular attention paid to identifying high-energy obesity, immunocompromised state, etc) may have a greater risk injuries, is critical to achieving optimal outcomes and of complications than a high-energy injury in a healthy patient.2 avoiding complications following tibial plateau fractures. Performing acute open reduction internal fixation will increase Staged management of tibial plateau fractures refers the risk of soft tissue complications (Figure 1).3 to the use of temporizing methods of care (often span- ning external fixation) in high-energy injuries, as well as delaying definitive fracture surgery until such a time History as the risk of soft tissue complications is decreased. A focused, yet complete, history and physical examination This article discusses the principles and techniques of is the first step in evaluating any patient with a fracture. It is staged management, including the use of less invasive crucial to recognize whether or not the patient was in a situ- methods for definitive stabilization. ation where a large amount of energy was imparted to the limb. Motor vehicle/motorcycle collisions, falls from heights ractures of the tibial plateau encompass a wide greater than 10 feet, or being struck by a vehicle while range of severity, from stable nondisplaced frac- walking are some of the more common high-energy mecha- tures with minimal soft tissue injury to highly nisms.2 An appropriate history also includes investigation comminuted unstable fractures with massive soft of patient factors (comorbid conditions) that could impact Ftissue injury that threaten limb viability.1 Careful and the treatment plan or affect the patient’s overall prognosis. -

Calcaneal Fracture and Rehabilitation
1 Calcaneal Fracture and Rehabilitation Surgical Indications and Considerations Anatomic Considerations: The calcaneus articulates with the talus superiorly at the subtalar joint. The three articulating surfaces of the subtalar joint are the: anterior, middle, and posterior facets, with the posterior facet representing the major weight-bearing surface. The subtalar joint is responsible for the majority of foot inversion/eversion (or pronation/supination). The interosseous ligament and medial, lateral, and posterior talocalcaneal ligaments provide additional support for the joint. The tibial artery, nerve, posterior tibial tendon, and flexor hallucis longus tendon are located medially to the calcaneus and are at risk for impingement with a calcaneal fracture, as are the peroneal tendons located on the lateral aspect of the calcaneus. The calcaneus serves three major functions: 1) acts as a foundation and support for the body’s weight, 2) supports the lateral column of the foot and acts as the main articulation for inversion/eversion, and 3) acts as a lever arm for the gastrocnemius muscle complex. Pathogenesis: Fractures of the calcaneal body, anterior process, sustentaculum tali, and superior tuberosity are known as extra-articular fractures and usually occur as a result of blunt force or sudden twisting. Fractures involving any of the three subtalar articulating surfaces are known as intra-articular fractures and are common results of: a fall from a height usually 6 feet or more, a motor vehicle accident (MVA), or an impact on a hard surface while running or jumping. Intra-articular fractures are commonly produced by axial loading; a combination of shearing and compression forces produce both the primary and secondary fracture lines. -

AM17 International Poster 008: Investigating the “Weekend Effect
9400 West Higgins Road, Suite 305 Rosemont, IL 60018-4975 Phone: (847) 698-1631 FAX: (847) 430-5140 E-mail: [email protected] It is my pleasure to provide the OTA Annual Meeting welcome for the sec- ond consecutive year. This anomaly is related to an organizational shift in the timing for transition of OTA held offices and positions from the Spring AAOS to the Fall OTA meeting. When the OTA was established, some 30 years ago, there was no OTA Annual Meeting. There was no OTA specific venue or opportunity for gathering, sharing, learning, educating, partner- ing, or doing OTA business. Since 1985, our Annual Meeting has grown from nonexistent to the premier orthopaedic trauma related meeting in the world. The timing shift for transition affected all committees. The Program William M. Ricci, MD Committee was no exception. Last year Mike McKee did double duty as the Program Committee Chair and Second President- Elect positions and Mike Gardner entered as Co-Chair of the Program Committee. Rather than following the normal two-year cycle in their Pro- gram Committee leadership duties, Mike McKee rotated off after one year to assume Presidential Line responsibilities, and Mike Gardner assumed the helm of the Program Committee a year early. Stephen Kottmeier joined the Program Committee as co-Chair. Despite the disturbance in normal cadence, the 2018 OTA Annual Meeting in Orlando, FL, as you will see, represents an evolution toward a more robust, more comprehensive, and more modern Annual Meeting sure to be our best yet. A testament to the commitment and dedication of all our member volunteers and the hard work of our OTA staff. -

Ankle and Foot Disorders Guideline
Ankle and Foot Disorders Effective Date: July 16, 2018 Contributors to Ankle and Foot Disorders Guideline Editor-in-Chief: Kurt T. Hegmann, MD, MPH, FACOEM, FACP Assistant Editor: Matthew A. Hughes, MD, MPH Evidence-based Practice Ankle and Foot Panel Chair: Nelson S. Haas, MD, MPH, FACOEM Evidence-based Practice Ankle and Foot Panel Members: Patrick J. Beecher, MD, MPH, MBA, FACOEM Mark Easley, MD Hannah Edwards, MD, MPH Harold Hoffman, MD, FRCPC Steven Mandel, MD, FACOEM RobRoy L. Martin, PhD, PT, CSCS Pete Thomas, DPM, QME The Evidence-based Practice Ankle/Foot Panel represents expertise in occupational medicine, neurology, podiatric surgery, foot and ankle surgery, physical therapy, and rehabilitation science. Guidelines Methodology Consultant: Kurt T. Hegmann, MD, MPH, FACOEM, FACP Research Conducted By: Kurt T. Hegmann, MD, MPH, FACOEM, FACP Matthew A. Hughes, MD, MPH Jeremy J. Biggs, MD, MSPH Matthew S. Thiese, PhD, MSPH Ulrike Ott, PhD, MSPH Kristine Hegmann, MSPH, CIC Atim Effiong, MPH Holly Diane Uphold Emilee Eden, MPH Jenna K. Lindsey, BS Copyright © 2008-2018 by Reed Group, Ltd. All rights reserved. Commercial use prohibited. Licenses may be purchased from Reed Group, Ltd. at https://www.mdguidelines.com/. Specialty Society and Society Representative Listing: ACOEM acknowledges the following organizations and their representatives who served as reviewers of the “Ankle and Foot Disorders” guideline. Their contributions are greatly appreciated. By listing the following individuals or organizations, it does not infer that these individuals or organizations support or endorse the ankle and foot treatment guidelines developed by ACOEM. Copyright ©2020 Reed Group, Ltd. Page | 1 2011 EXTERNAL REVIEWERS American Physical Therapy Association Stephanie Albin, DPT, FAAOMPT, OCS Thomas G. -

Fracture Blisters
CONTINUING MEDICAL EDUCATION Objectives After completion of this CME, the reader will: 1) Understand the etiology of fracture blisters. 2) Understand the difference Fracture Blisters between serous and hemor- rhagic fracture blisters. Here’s how to recognize and treat 3) Gain information on the various treatment options for this complication. the blisters. 4) Understand ways to pre- BY GEORGE F. WALLACE, DPM, MBA vent fracture blisters. 141 Welcome to Podiatry Management’s CME Instructional program. Our journal has been approved as a sponsor of Con- tinuing Medical Education by the Council on Podiatric Medical Education. You may enroll: 1) on a per issue basis (at $26.00 per topic) or 2) per year, for the special rate of $210 (you save $50). You may submit the answer sheet, along with the other information requested, via mail, fax, or phone. You can also take this and other exams on the Internet at www.podiatrym.com/cme. If you correctly answer seventy (70%) of the questions correctly, you will receive a certificate attesting to your earned credits. You will also receive a record of any incorrectly answered questions. If you score less than 70%, you can retake the test at no additional cost. A list of states currently honoring CPME approved credits is listed on pg. 146. Other than those entities currently accepting CPME-approved credit, Podiatry Management cannot guarantee that these CME credits will be acceptable by any state licensing agency, hospital, managed care organization or other entity. PM will, however, use its best efforts to ensure the widest acceptance of this program possible. -

Fracture Blisters
Case RepoRt Fracture Blisters Claire M. Uebbing, MD* *Henry Ford Hospital, Detroit, MI Mark Walsh, MD† †Indiana University School of Medicine, South Bend Campus Joseph B. Miller, MD* ‡Memorial Hospital of South Bend Mathew Abraham, MD‡ Clifford Arnold‡ Supervising Section Editor: Jeffrey Druck, MD Submission history: Submitted May 18, 2010; Revision received August 9, 2010; Accepted October 11, 2010 Reprints available through open access at http://escholarship.org/uc/uciem_westjem Fracture blisters are a relatively uncommon complication of fractures in locations of the body, such as the ankle, wrist elbow and foot, where skin adheres tightly to bone with little subcutaneous fat cushioning. The blister that results resembles that of a second degree burn. These blisters significantly alter treatment, making it difficult to splint or cast and often overlying ideal surgical incision sites. Review of the literature reveals no consensus on management; however, most authors agree on early treatment prior to blister formation or delay until blister resolution before attempting surgical correction or stabilization. [West J Emerg Med. 2011;12(1):131-133.] INTRODUCTION The patient presented two days later complaining of Fracture blisters are relatively uncommon, occurring in blisters bulging from his splint. He did admit to walking on 1 about 2.9% of all acute fractures requiring hospitalization. his splint to get back and forth to the bathroom, but said that These blisters alter the management and definitive repair he thought it was only a sprain. significantly; however, there is still no consensus on the Physical exam revealed interval formation of large, timing of surgery nor the treatment of the blisters themselves. -

Curriculum Vitae
Curriculum vitae Cyril Mauffrey, MD, FACS, FRCS Board Certified Orthopaedic Surgeon (ABOS : American Board of Orthopaedic Surgery) Professor of Orthopedics University of Colorado School of Medicine Director of Service (Interim) Director of Division: Orthopaedic Trauma Director of Division: Orthopaedic Research Director of the Orthopaedic Trauma Fellowship Department of Orthopedics, Physical Medicine & Rehabilitation Denver Health Medical Center 777 Bannock Street MC 0188 Denver, Colorado 80204 Orthopaedic Trauma and limb reconstructive Surgeon Complex fractures, pelvis/acetabulum/non-unions/infections Editor in Chief The European Journal of Orthopaedic Surgery and Traumatology (Springer) Editor (Basic Sciences and biomechanics section) Injury, International Journal of the Care of the Injured (Elsevier) Email: [email protected] Cell: +1 720-362-0361 PERSONAL DATA Languages: English, French, Italian and Spanish 1 BOARD CERTIFICATION • American Board of Orthopaedic Surgery (ABOS) Certified • The Royal College of Surgeons (Intercollegiate) boards in Trauma and Orthopaedics, UK, May 2010 (FRCS Tr&Orth) LICENSURES HELD CURRENT AND PAST • Colorado full medical license (current) • State License in Kentucky (expired) • General Medical Council (United Kingdom) UNDERGRADUATE EDUCATION • Singapore French International School 1980 – 1986 • Hong-Kong French International School 1986 – 1993, Scientific Baccalaureate. MEDICAL EDUCATION • The University of Turin Medical School, Italy 1996-2002 RESIDENCY PROGRAM • The Royal College of Surgeons Basic surgical training, Birmingham (UK) 2003- 2006 [neurosurgery, plastics surgery, trauma and Orthopaedics], obtained Certificate of Completion of basic surgical training (CCBST in 2006). • The Royal College of Surgeons Higher surgical training, Birmingham (UK) 2006- 2011 [Trauma and Orthopaedics]. FELLOWSHIPS • Orthopedic trauma, University of Louisville Hospital, Jul 2010-Jul 2011. • AIOD Trauma Fellowship, September 2007, Louisville, USA. -

Fracture Blisters After Primary Total Knee Arthroplasty
A Case Report & Literature Review Fracture Blisters After Primary Total Knee Arthroplasty Mohamad J. Halawi, MD Abstract Fracture blisters are tense vesicles that arise on mark- deep venous thrombosis. The patient was treated with leg edly swollen skin overlying traumatized soft tissue. While elevation, loosely applied nonadhesive dressings, and a this relatively uncommon complication has been well short course of oral antibiotics after skin desquamation. described in the trauma literature, this article reports for Blood-filled blisters required longer time to reepithelial- the first time a case of fracture blisters after primary total ization than fluid-filled blisters. Knee stiffness developed knee arthroplasty. The fracture blisters developed within because of pain and fear of participation with physical 36 hours of surgery and were associated with profound therapy, but the patient was able to resume intensive re- swelling and erythema. There was no evidence of vascu- habilitation after resolution of the blisters. Patient factors, lar injury, compartment syndrome, iatrogenic fracture, or surgical factors, and review of the literature are discussed. racture blisters are a relatively uncommon complication swollen and erythematous skin. The incision was minimally of high-energy fractures, with an incidence of 2.9%.1 involved (Figure A). There was diffuse 2+ pitting edema with FIn the lower extremity, fracture blisters almost always hyperesthesia in the affected skin distal to the knee. Prior to 1 AJO occur distal to the knee. Histologically, the blisters represent these findings, the patient had complained of increasing pain an injury to the dermoepidermal junction.2 On physical ex- in his operative leg, but there was no escalation in analgesic re- amination, there are tense blood- and/or clear fluid–filled quirements. -

Staged Vs Early Definitive Fixation of High Energy Tibial Plateau and Plafond Fractures: What Is Best for the Soft Tissues and the Patient?
Staged vs Early Definitive Fixation of High Energy Tibial Plateau and Plafond Fractures: What is best for the soft tissues and the patient? Summary Bicondylar tibial plateau fractures and pilon fractures commonly result from a high energy injury mechanism, and are frequently associated with significant insult to the soft tissue envelope surrounding these fractures. Although excellent outcome and low complication rates were reported in early case series1 where low energy pilon fractures were managed with ORIF, application of this management to high energy pilon (and plateau) fractures resulted in significantly worse outcomes and alarmingly high complication rates.2,3,5,6 Implementation of a staged management protocol2,3,5 for these injuries has resulted in significantly improved outcomes and reduced complication rates. For this reason, staged management of high energy tibial plateau and pilon fractures has become widely adopted and is in most cases the “standard of care” for these injuries. Early definitive fixation of high energy tibial plateau and plafond fractures continues to have a role in the management of some patients with this type of injury. The results of several recent retrospective cohort studies7,8,9 show that early definitive fixation can be performed safely with outcomes and complication rates comparable to results achievable with staged management protocols. These studies point to several factors which seem to be the key to obtaining improved results with early definitive fixation: careful selection of patients appropriate for early care based on assessment of the soft tissue envelope, injury to surgery time typically less than 48h, avoidance of traditional single-incision approaches, and use of minimally invasive plate osteosynthesis techniques. -

Fracture Blisters Should Be Malleolus
CHAPTER 47 FRACTI]RE BLISTERS Richard J. Zirm, D.P.M. The treatment of fractures complicated by overly- in general. This signifies a lack of extensive araeri- ing trauma blister formation remains controversial oles between the rete ridges. Second, the as well as intimidating. There is very litt1e objective subcutaneous fat is sparse, especially over the data in the literature regarding their characteristics medial malleo1us and the lateral calcaneus where and management. Previous recommendations have the skin is relatively thin. There is an absence of ranged from benign neglect with operative well-formed adipose or muscular layers which, management through the blister, to surgical delay when present elsewhere protect the skin and until blister reepithelialization has occurred.' The deeper structures. The skin over the medial malle- most serious concern is the potential increased risk olus is usually 1.5 to 2.5 mm thick compared to 5 for infection that the fracture area presents. mm on the soles and palms.3 Additionally, there is Intelligent clinical decisions regarding the treatment extensive arborization of veins over the medial of fractures involving fracture blisters should be malleolus. Rupture of the venous plexuses causes made to prevent untoward complications. extensive hemorrhage, venous obstruction and arterial spasm. Finally, there is a significant varia- ETIOLOGY tion in the amount of hair follicles surrounding the foot and ankle. This may have important conse- Fracture blisters occuf after high-energy trat)mz, quences in the re-epithelialization of wounds since and are especially associated with a shear or torque the hair follicle is a major source of epithelial cells.