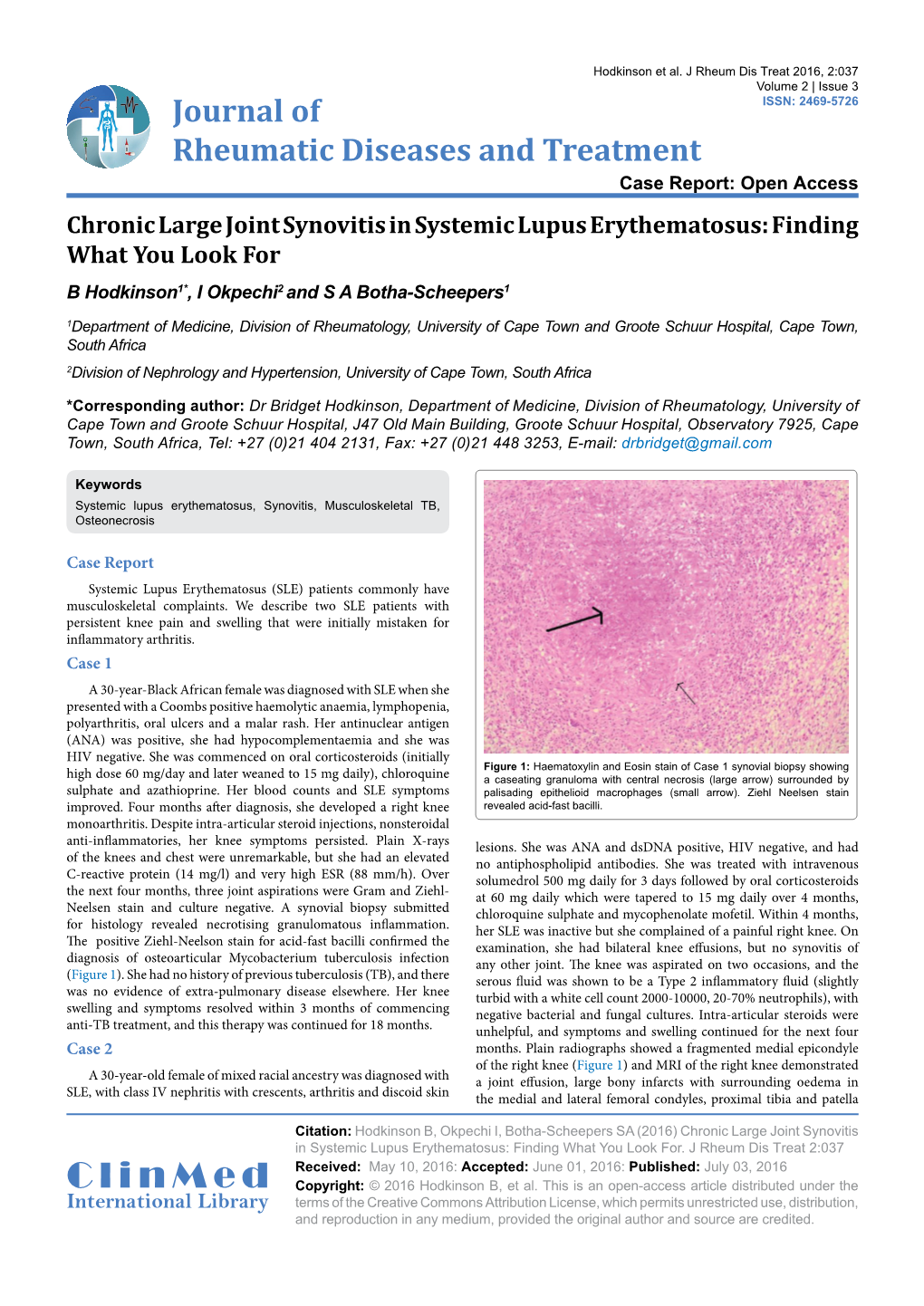
Chronic Large Joint Synovitis in Systemic Lupus Erythematosus: Finding What You Look for B Hodkinson1*, I Okpechi2 and S a Botha-Scheepers1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Synovial Fluidfluid 11
LWBK461-c11_p253-262.qxd 11/18/09 6:04 PM Page 253 Aptara Inc CHAPTER SynovialSynovial FluidFluid 11 Key Terms ANTINUCLEAR ANTIBODY ARTHROCENTESIS BULGE TEST CRYSTAL-INDUCED ARTHRITIS GROUND PEPPER HYALURONATE MUCIN OCHRONOTIC SHARDS RHEUMATOID ARTHRITIS (RA) RHEUMATOID FACTOR (RF) RICE BODIES ROPE’S TEST SEPTIC ARTHRITIS Learning Objectives SYNOVIAL SYSTEMIC LUPUS ERYTHEMATOSUS 1. Define synovial. VISCOSITY 2. Describe the formation and function of synovial fluid. 3. Explain the collection and handling of synovial fluid. 4. Describe the appearance of normal and abnormal synovial fluids. 5. Correlate the appearance of synovial fluid with possible cause. 6. Interpret laboratory tests on synovial fluid. 7. Suggest further testing for synovial fluid, based on preliminary results. 8. List the four classes or categories of joint disease. 9. Correlate synovial fluid analyses with their representative disease classification. 253 LWBK461-c11_p253-262.qxd 11/18/09 6:04 PM Page 254 Aptara Inc 254 Graff’s Textbook of Routine Urinalysis and Body Fluids oint fluid is called synovial fluid because of its resem- blance to egg white. It is a viscous, mucinous substance Jthat lubricates most joints. Analysis of synovial fluid is important in the diagnosis of joint disease. Aspiration of joint fluid is indicated for any patient with a joint effusion or inflamed joints. Aspiration of asymptomatic joints is beneficial for patients with gout and pseudogout as these fluids may still contain crystals.1 Evaluation of physical, chemical, and microscopic characteristics of synovial fluid comprise routine analysis. This chapter includes an overview of the composition and function of synovial fluid, and laboratory procedures and their interpretations. -

Adult Still's Disease
44 y/o male who reports severe knee pain with daily fevers and rash. High ESR, CRP add negative RF and ANA on labs. Edward Gillis, DO ? Adult Still’s Disease Frontal view of the hands shows severe radiocarpal and intercarpal joint space narrowing without significant bony productive changes. Joint space narrowing also present at the CMC, MCP and PIP joint spaces. Diffuse osteopenia is also evident. Spot views of the hands after Tc99m-MDP injection correlate with radiographs, showing significantly increased radiotracer uptake in the wrists, CMC, PIP, and to a lesser extent, the DIP joints bilaterally. Tc99m-MDP bone scan shows increased uptake in the right greater than left shoulders, as well as bilaterally symmetric increased radiotracer uptake in the elbows, hands, knees, ankles, and first MTP joints. Note the absence of radiotracer uptake in the hips. Patient had bilateral total hip arthroplasties. Not clearly evident are bilateral shoulder hemiarthroplasties. The increased periprosthetic uptake could signify prosthesis loosening. Adult Stills Disease Imaging Features • Radiographs – Distinctive pattern of diffuse radiocarpal, intercarpal, and carpometacarpal joint space narrowing without productive bony changes. Osseous ankylosis in the wrists common late in the disease. – Joint space narrowing is uniform – May see bony erosions. • Tc99m-MDP Bone Scan – Bilaterally symmetric increased uptake in the small and large joints of the axial and appendicular skeleton. Adult Still’s Disease General Features • Rare systemic inflammatory disease of unknown etiology • 75% have onset between 16 and 35 years • No gender, race, or ethnic predominance • Considered adult continuum of JIA • Triad of high spiking daily fevers with a skin rash and polyarthralgia • Prodromal sore throat is common • Negative RF and ANA Adult Still’s Disease General Features • Most commonly involved joint is the knee • Wrist involved in 74% of cases • In the hands, interphalangeal joints are more commonly affected than the MCP joints. -

Joint Pain Or Joint Disease
ARTHRITIS BY THE NUMBERS Book of Trusted Facts & Figures 2020 TABLE OF CONTENTS Introduction ............................................4 Medical/Cost Burden .................................... 26 What the Numbers Mean – SECTION 1: GENERAL ARTHRITIS FACTS ....5 Craig’s Story: Words of Wisdom What is Arthritis? ...............................5 About Living With Gout & OA ........................ 27 Prevalence ................................................... 5 • Age and Gender ................................................................ 5 SECTION 4: • Change Over Time ............................................................ 7 • Factors to Consider ............................................................ 7 AUTOIMMUNE ARTHRITIS ..................28 Pain and Other Health Burdens ..................... 8 A Related Group of Employment Impact and Medical Cost Burden ... 9 Rheumatoid Diseases .........................28 New Research Contributes to Osteoporosis .....................................9 Understanding Why Someone Develops Autoimmune Disease ..................... 28 Who’s Affected? ........................................... 10 • Genetic and Epigenetic Implications ................................ 29 Prevalence ................................................... 10 • Microbiome Implications ................................................... 29 Health Burdens ............................................. 11 • Stress Implications .............................................................. 29 Economic Burdens ........................................ -

Approach to Polyarthritis for the Primary Care Physician
24 Osteopathic Family Physician (2018) 24 - 31 Osteopathic Family Physician | Volume 10, No. 5 | September / October, 2018 REVIEW ARTICLE Approach to Polyarthritis for the Primary Care Physician Arielle Freilich, DO, PGY2 & Helaine Larsen, DO Good Samaritan Hospital Medical Center, West Islip, New York KEYWORDS: Complaints of joint pain are commonly seen in clinical practice. Primary care physicians are frequently the frst practitioners to work up these complaints. Polyarthritis can be seen in a multitude of diseases. It Polyarthritis can be a challenging diagnostic process. In this article, we review the approach to diagnosing polyarthritis Synovitis joint pain in the primary care setting. Starting with history and physical, we outline the defning characteristics of various causes of arthralgia. We discuss the use of certain laboratory studies including Joint Pain sedimentation rate, antinuclear antibody, and rheumatoid factor. Aspiration of synovial fuid is often required for diagnosis, and we discuss the interpretation of possible results. Primary care physicians can Rheumatic Disease initiate the evaluation of polyarthralgia, and this article outlines a diagnostic approach. Rheumatology INTRODUCTION PATIENT HISTORY Polyarticular joint pain is a common complaint seen Although laboratory studies can shed much light on a possible diagnosis, a in primary care practices. The diferential diagnosis detailed history and physical examination remain crucial in the evaluation is extensive, thus making the diagnostic process of polyarticular symptoms. The vast diferential for polyarticular pain can difcult. A comprehensive history and physical exam be greatly narrowed using a thorough history. can help point towards the more likely etiology of the complaint. The physician must frst ensure that there are no symptoms pointing towards a more serious Emergencies diagnosis, which may require urgent management or During the initial evaluation, the physician must frst exclude any life- referral. -

Arthritis and Joint Pain
Fact Sheet News from the IBD Help Center ARTHRITIS AND JOINT PAIN Arthritis, or inflammation (pain with swelling) of the joints, is the most common extraintestinal complication of IBD. It may affect as many as 30% of people with Crohn’s disease or ulcerative colitis. Although arthritis is typically associated with advancing age, in IBD it often strikes younger patients as well. In addition to joint pain, arthritis also causes swelling of the joints and a reduction in flexibility. It is important to point out that people with arthritis may experience arthralgia, but many people with arthralgia may not have arthritis. Types of Arthritis • Peripheral Arthritis. Peripheral arthritis usually affects the large joints of the arms and legs, including the elbows, wrists, knees, and ankles. The discomfort may be “migratory,” moving from one joint to another. If left untreated, the pain may last from a few days to several weeks. Peripheral arthritis tends to be more common among people who have ulcerative colitis or Crohn’s disease of the colon. The level of inflammation in the joints generally mirrors the extent of inflammation in the colon. Although no specific test can make an absolute diagnosis, various diagnostic methods—including analysis of joint fluid, blood tests, and X-rays—are used to rule out other causes of joint pain. Fortunately, IBD-related peripheral arthritis usually does not cause any lasting damage and treatment of the underlying IBD typically results in improvement in the joint discomfort. • Axial Arthritis. Also known as spondylitis or spondyloarthropathy, axial arthritis produces pain and stiffness in the lower spine and sacroiliac joints (at the bottom of the back). -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Conditions Related to Inflammatory Arthritis
Conditions Related to Inflammatory Arthritis There are many conditions related to inflammatory arthritis. Some exhibit symptoms similar to those of inflammatory arthritis, some are autoimmune disorders that result from inflammatory arthritis, and some occur in conjunction with inflammatory arthritis. Related conditions are listed for information purposes only. • Adhesive capsulitis – also known as “frozen shoulder,” the connective tissue surrounding the joint becomes stiff and inflamed causing extreme pain and greatly restricting movement. • Adult onset Still’s disease – a form of arthritis characterized by high spiking fevers and a salmon- colored rash. Still’s disease is more common in children. • Caplan’s syndrome – an inflammation and scarring of the lungs in people with rheumatoid arthritis who have exposure to coal dust, as in a mine. • Celiac disease – an autoimmune disorder of the small intestine that causes malabsorption of nutrients and can eventually cause osteopenia or osteoporosis. • Dermatomyositis – a connective tissue disease characterized by inflammation of the muscles and the skin. The condition is believed to be caused either by viral infection or an autoimmune reaction. • Diabetic finger sclerosis – a complication of diabetes, causing a hardening of the skin and connective tissue in the fingers, thus causing stiffness. • Duchenne muscular dystrophy – one of the most prevalent types of muscular dystrophy, characterized by rapid muscle degeneration. • Dupuytren’s contracture – an abnormal thickening of tissues in the palm and fingers that can cause the fingers to curl. • Eosinophilic fasciitis (Shulman’s syndrome) – a condition in which the muscle tissue underneath the skin becomes swollen and thick. People with eosinophilic fasciitis have a buildup of eosinophils—a type of white blood cell—in the affected tissue. -

Still Disease
University of Massachusetts Medical School eScholarship@UMMS Open Access Articles Open Access Publications by UMMS Authors 2019-02-17 Still Disease Juhi Bhargava Medstar Washington Hospital Center Et al. Let us know how access to this document benefits ou.y Follow this and additional works at: https://escholarship.umassmed.edu/oapubs Part of the Immune System Diseases Commons, Musculoskeletal Diseases Commons, Pathological Conditions, Signs and Symptoms Commons, Skin and Connective Tissue Diseases Commons, and the Viruses Commons Repository Citation Bhargava J, Panginikkod S. (2019). Still Disease. Open Access Articles. Retrieved from https://escholarship.umassmed.edu/oapubs/3764 Creative Commons License This work is licensed under a Creative Commons Attribution 4.0 License. This material is brought to you by eScholarship@UMMS. It has been accepted for inclusion in Open Access Articles by an authorized administrator of eScholarship@UMMS. For more information, please contact [email protected]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Still Disease Juhi Bhargava; Sreelakshmi Panginikkod. Author Information Last Update: February 17, 2019. Go to: Introduction Adult Onset Still's Disease (AOSD) is a rare systemic inflammatory disorder characterized by daily fever, inflammatory polyarthritis, and a transient salmon-pink maculopapular rash. AOSD is alternatively known as systemic onset juvenile idiopathic arthritis. Even though there is no specific diagnostic test, a serum ferritin level more than 1000ng/ml is common in AOSD. Go to: Etiology The etiology of AOSD is unknown. The hypothesis remains that AOSD is a reactive syndrome in which various infectious agents may act as triggers in a genetically predisposed host. Both genetic factors and a variety of viruses, bacteria like Yersinia enterocolitica and Mycoplasma pneumonia and other infectious factors have been suggested as important[1][2]. -

Juvenile Idiopathic Arthritis Associated Uveitis
children Review Juvenile Idiopathic Arthritis Associated Uveitis Emil Carlsson 1,*, Michael W. Beresford 1,2,3, Athimalaipet V. Ramanan 4, Andrew D. Dick 5,6,7 and Christian M. Hedrich 1,2,3,* 1 Department of Women’s and Children’s Health, Institute of Life Course and Medical Sciences, University of Liverpool, Liverpool L14 5AB, UK; [email protected] 2 Department of Rheumatology, Alder Hey Children’s NHS Foundation Trust Hospital, Liverpool L14 5AB, UK 3 National Institute for Health Research Alder Hey Clinical Research Facility, Alder Hey Children’s NHS Foundation Trust Hospital, Liverpool L14 5AB, UK 4 Bristol Royal Hospital for Children & Translational Health Sciences, University of Bristol, Bristol BS2 8DZ, UK; [email protected] 5 Translational Health Sciences, University of Bristol, Bristol BS2 8DZ, UK; [email protected] 6 UCL Institute of Ophthalmology, London EC1V 9EL, UK 7 NIHR Biomedical Research Centre, Moorfields Eye Hospital, London EC1V 2PD, UK * Correspondence: [email protected] (E.C.); [email protected] (C.M.H.); Tel.: +44-151-228-4811 (ext. 2690) (E.C.); +44-151-252-5849 (C.M.H.) Abstract: Juvenile idiopathic arthritis (JIA) is the most common childhood rheumatic disease. The development of associated uveitis represents a significant risk for serious complications, including permanent loss of vision. Initiation of early treatment is important for controlling JIA-uveitis, but the disease can appear asymptomatically, making frequent screening procedures necessary for patients at risk. As our understanding of pathogenic drivers is currently incomplete, it is difficult to assess which JIA patients are at risk of developing uveitis. -

Scoring Adult Onset Still's Disease
Editorial Scoring Adult Onset Still’s Disease Adult-onset Still’s disease (AOSD) is a systemic inflamma- patient may be counterproductive as initial treatment; simi- tory disease of uncertain etiology. Patients with AOSD larly, antiinfective treatment of an AOSD patient may delay develop a combination of several disease manifestations. immunosuppression. Thus, differentiating these 2 diseases Some of these disease manifestations are arthritis, fever, is important. leukocytosis, and evanescent rash. But, in parallel, various Besides the above mentioned AOSD classification and systemic manifestations such as splenomegaly and pneu- diagnostic criteria, Pouchot, et al published an activity monitis, among others, may occur. score with a sensitivity of 92% and a specificity of 93% for The diagnosis of AOSD is problematic, because no single discriminating active and non-active AOSD12. And, in this diagnostic test or characteristic histopathology exists. Patients issue of The Journal, Rau, et al13 used the same Pouchot sometimes suffer from delays in diagnosis including protract- score12 in a changed version, adding arthritis and serum fer- ed efforts to exclude occult infection or neoplasm because ritin > 3000 µg/l as new factors instead of abdominal pain AOSD is a rare diagnosis, and differential diagnoses must be and splenomegaly. The other factors of the Pouchot score excluded. The clinician should consider AOSD in the evalua- comprised fever, evanescent rash, pharyngitis, myalgia, tion of undiagnosed fever of unknown origin, particularly if pleuritis, pericarditis, pneumonia, lymphadenopathy, present in association with rheumatic complaints1. hepatomegaly or elevated liver enzymes, and leukocyte More than 99% of patients with AOSD manifest with fever count > 15,000/µl. -

A Rheumatologist Needs to Know About the Adult with Juvenile Idiopathic Arthritis
A Rheumatologist Needs to Know About the Adult With Juvenile Idiopathic Arthritis Juvenile idiopathic arthritis (JIA) encompasses a range of distinct phenotypes. By definition, JIA includes all forms of arthritis of unknown cause that start before the 16th birthday. The most common form is oligoarticular JIA, typically starting in early childhood (before age 6) and affecting only a few large joints. Polyarticular JIA, affecting 5 joints or more, can occur at any age; older children may develop seropositive arthritis indistinguishable from adult rheumatoid arthritis. Systemic JIA (sJIA) is characterized by fevers and rash at onset of disease, though it may evolve into an afebrile chronic polyarthritis that can be resistant to therapy. Patients with sJIA, like those with adult onset Still’s disease (AOSD), are susceptible to macrophage activation syndrome, a “cytokine storm” characterized by fever, disseminated intravascular coagulation, and end organ dysfunction. Other forms of arthritis in children include psoriatic JIA and so-called “enthesitis related arthritis,” encompassing the non-psoriatic spondyloarthropathies. Approximately 50% of JIA patients will have active disease into adulthood. JIA can be accompanied by destructive chronic uveitis. In addition to joints, JIA can involve the eyes, resulting in a form of chronic scarring uveitis not seen in adult arthritis. Patients at particularly high risk are those with oligoarticular or polyarticular arthritis beginning before the age of 6 years, especially if accompanied by positive ANA at any titer. In thehighest risk group, up to 30% of children may be affected. Patients who did not develop uveitis in childhood are very unlikely to do so as adults. -

T Helper Cell Infiltration in Osteoarthritis-Related Knee Pain
Journal of Clinical Medicine Article T Helper Cell Infiltration in Osteoarthritis-Related Knee Pain and Disability 1, 1, 1 1 Timo Albert Nees y , Nils Rosshirt y , Jiji Alexander Zhang , Hadrian Platzer , Reza Sorbi 1, Elena Tripel 1, Tobias Reiner 1, Tilman Walker 1, Marcus Schiltenwolf 1 , 2 2 1, 1, , Hanns-Martin Lorenz , Theresa Tretter , Babak Moradi z and Sébastien Hagmann * z 1 Clinic for Orthopedics and Trauma Surgery, Center for Orthopedics, Trauma Surgery and Spinal Cord Injury, Heidelberg University Hospital, Schlierbacher Landstr. 200a, 69118 Heidelberg, Germany; [email protected] (T.A.N.); [email protected] (N.R.); [email protected] (J.A.Z.); [email protected] (H.P.); [email protected] (R.S.); [email protected] (E.T.); [email protected] (T.R.); [email protected] (T.W.); [email protected] (M.S.); [email protected] (B.M.) 2 Department of Internal Medicine V, Division of Rheumatology, Heidelberg University Hospital, Im Neuenheimer Feld 410, 69120 Heidelberg, Germany; [email protected] (H.-M.L.); [email protected] (T.T.) * Correspondence: [email protected]; Tel.: +49-622-1562-6289; Fax: +49-622-1562-6348 These authors contributed equally to this study. y These authors share senior authorship. z Received: 16 June 2020; Accepted: 23 July 2020; Published: 29 July 2020 Abstract: Despite the growing body of literature demonstrating a crucial role of T helper cell (Th) responses in the pathogenesis of osteoarthritis (OA), only few clinical studies have assessed interactions between Th cells and OA—related symptoms.