A. Beta-Lactam Antibiotics A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Small Outbreak of Third Generation Cephem-Resistant Citrobacter
Jpn. J. Infect. Dis., 57, 2004 Laboratory and Epidemiology Communications A Small Outbreak of Third Generation Cephem-Resistant Citrobacter freundii Infection on a Surgical Ward Toshi Nada*, Hisashi Baba, Kumiko Kawamura2, Teruko Ohkura, Keizo Torii1 and Michio Ohta1 Department of Clinical Laboratory, Nagoya University Hospital, Nagoya 466-8560, 1Department of Bacteriology, Nagoya University Graduate School of Medicine, Nagoya 466-8550 and 2Department of Medical Technology, Nagoya University School of Health Sciences, Nagoya 461-8673 Communicated by Yoshichika Arakawa (Accepted June 11, 2004) Citrobacter freundii is a member of family Enterobacteri- from those of type a and b strains. aceae and has been associated with nosocomial infections As previous studies have indicated, third generation in the urinary, respiratory, and biliary tracts of debilitated cephem-resistance of Gram-negative bacteria are due to the hospital patients. C. freundii has an inducible chromosomally hydrolysis of β-lactams by β-lactamases. These β-lactamases encoded cephalosporinase that can inactivate cephamycins include extended spectrum β-lactamase (ESBL), metallo- and cephalosporins. However, most clinical isolates are β-lactamase, and plasmid-encoded AmpC cephalosporinase sensitive to new third generation cephems and carbapenems. (1-3). ESBL confers variable levels of resistance to cefotaxime, We report here a small outbreak of infection caused by ceftazidime, and other broad-spectrum cephalosporins and third generation cephem-resistant C. freundii on a surgical to monobactams, but has no detectable activity against ward of a university hospital in 2002. We identified four cephamycins and carbapenems, and is relatively sensitive patients with biliary infection and two carrier patients during to sulbactam (1). Plasmid-encoded metallo-β-lactamase July and October. -

Sepsis Caused by Newly Identified Capnocytophaga Canis Following Cat Bites: C
doi: 10.2169/internalmedicine.9196-17 Intern Med 57: 273-277, 2018 http://internmed.jp 【 CASE REPORT 】 Sepsis Caused by Newly Identified Capnocytophaga canis Following Cat Bites: C. canis Is the Third Candidate along with C. canimorsus and C. cynodegmi Causing Zoonotic Infection Minami Taki 1, Yoshio Shimojima 1, Ayako Nogami 2, Takuhiro Yoshida 1, Michio Suzuki 3, Koichi Imaoka 3, Hiroki Momoi 1 and Norinao Hanyu 1 Abstract: Sepsis caused by a Capnocytophaga canis infection has only been rarely reported. A 67-year-old female with a past medical history of splenectomy was admitted to our hospital with fever and general malaise. She had been bitten by a cat. She showed disseminated intravascular coagulation and multi-organ failure because of severe sepsis. On blood culture, characteristic gram-negative fusiform rods were detected; therefore, a Capnocytophaga species infection was suspected. A nucleotide sequence analysis revealed the species to be C. canis, which was newly identified in 2016. C. canis may have low virulence in humans; however, C. canis with oxidase activity may cause severe zoonotic infection. Key words: Capnocytophaga canis, Capnocytophaga canimorsus, sepsis, oxidase activity (Intern Med 57: 273-277, 2018) (DOI: 10.2169/internalmedicine.9196-17) Introduction Case Report The genus Capnocytophaga consists of gram-negative A 67-year-old woman was admitted to our hospital with rod-shaped bacteria that reside in the oral cavities of humans general malaise and fever for 3 days starting the day after and domestic animals. Capnocytophaga formerly comprised being bitten by a cat on both her hands. She had a medical eight species (1, 2). -

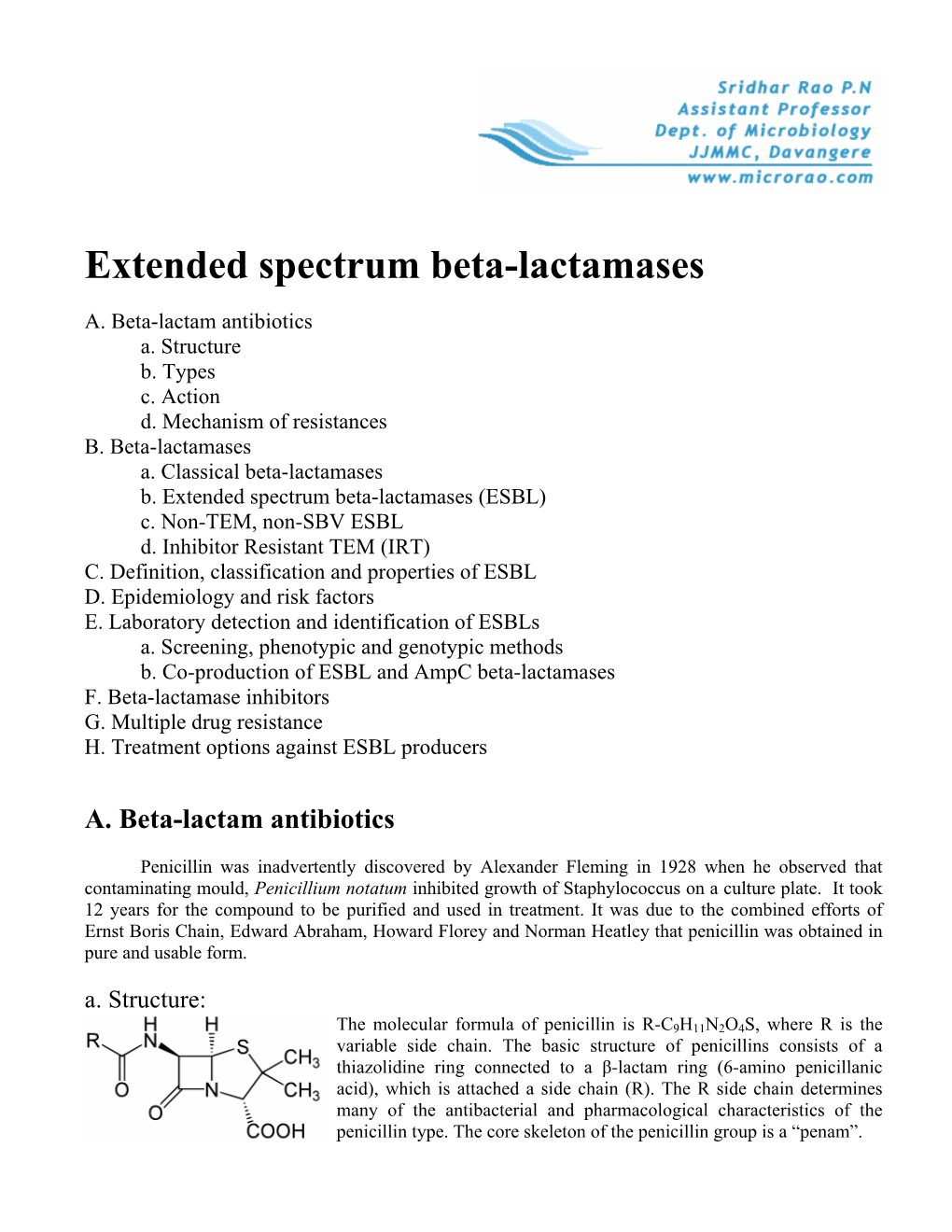
B-Lactams: Chemical Structure, Mode of Action and Mechanisms of Resistance
b-Lactams: chemical structure, mode of action and mechanisms of resistance Ru´ben Fernandes, Paula Amador and Cristina Prudeˆncio This synopsis summarizes the key chemical and bacteriological characteristics of b-lactams, penicillins, cephalosporins, carbanpenems, monobactams and others. Particular notice is given to first-generation to fifth-generation cephalosporins. This review also summarizes the main resistance mechanism to antibiotics, focusing particular attention to those conferring resistance to broad-spectrum cephalosporins by means of production of emerging cephalosporinases (extended-spectrum b-lactamases and AmpC b-lactamases), target alteration (penicillin-binding proteins from methicillin-resistant Staphylococcus aureus) and membrane transporters that pump b-lactams out of the bacterial cell. Keywords: b-lactams, chemical structure, mechanisms of resistance, mode of action Historical perspective Alexander Fleming first noticed the antibacterial nature of penicillin in 1928. When working with Antimicrobials must be understood as any kind of agent another bacteriological problem, Fleming observed with inhibitory or killing properties to a microorganism. a contaminated culture of Staphylococcus aureus with Antibiotic is a more restrictive term, which implies the the mold Penicillium notatum. Fleming remarkably saw natural source of the antimicrobial agent. Similarly, under- the potential of this unfortunate event. He dis- lying the term chemotherapeutic is the artificial origin of continued the work that he was dealing with and was an antimicrobial agent by chemical synthesis [1]. Initially, able to describe the compound around the mold antibiotics were considered as small molecular weight and isolates it. He named it penicillin and published organic molecules or metabolites used in response of his findings along with some applications of penicillin some microorganisms against others that inhabit the same [4]. -

Who Expert Committee on Specifications for Pharmaceutical Preparations
WHO Technical Report Series 902 WHO EXPERT COMMITTEE ON SPECIFICATIONS FOR PHARMACEUTICAL PREPARATIONS A Thirty-sixth Report aA World Health Organization Geneva i WEC Cover1 1 1/31/02, 6:35 PM The World Health Organization was established in 1948 as a specialized agency of the United Nations serving as the directing and coordinating authority for international health matters and public health. One of WHO’s constitutional functions is to provide objective and reliable information and advice in the field of human health, a responsibility that it fulfils in part through its extensive programme of publications. The Organization seeks through its publications to support national health strat- egies and address the most pressing public health concerns of populations around the world. To respond to the needs of Member States at all levels of development, WHO publishes practical manuals, handbooks and training material for specific categories of health workers; internationally applicable guidelines and standards; reviews and analyses of health policies, programmes and research; and state-of-the-art consensus reports that offer technical advice and recommen- dations for decision-makers. These books are closely tied to the Organization’s priority activities, encompassing disease prevention and control, the development of equitable health systems based on primary health care, and health promotion for individuals and communities. Progress towards better health for all also demands the global dissemination and exchange of information that draws on the knowledge and experience of all WHO’s Member countries and the collaboration of world leaders in public health and the biomedical sciences. To ensure the widest possible availability of authoritative information and guidance on health matters, WHO secures the broad international distribution of its publica- tions and encourages their translation and adaptation. -

(12) Patent Application Publication (10) Pub. No.: US 2011/0136210 A1 Benjamin Et Al
US 2011013621 OA1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2011/0136210 A1 Benjamin et al. (43) Pub. Date: Jun. 9, 2011 (54) USE OF METHYLSULFONYLMETHANE Publication Classification (MSM) TO MODULATE MICROBIAL ACTIVITY (51) Int. Cl. CI2N 7/06 (2006.01) (75) Inventors: Rodney L. Benjamin, Camas, WA CI2N I/38 (2006.01) (US); Jeffrey Varelman, Moyie (52) U.S. Cl. ......................................... 435/238; 435/244 Springs, ID (US); Anthony L. (57) ABSTRACT Keller, Ashland, OR (US) Disclosed herein are methods of use of methylsulfonyl (73) Assignee: Biogenic Innovations, LLC methane (MSM) to modulate microbial activity, such as to enhance or inhibit the activity of microorganisms. In one (21) Appl. No.: 13/029,001 example, MSM (such as about 0.5% to 5% MSM) is used to enhance fermentation efficiency. Such as to enhance fermen (22) Filed: Feb. 16, 2011 tation efficiency associated with the production of beer, cider, wine, a biofuel, dairy product or any combination thereof. Related U.S. Application Data Also disclosed are in vitro methods for enhancing the growth of one or more probiotic microorganisms and methods of (63) Continuation of application No. PCT/US2010/ enhancing growth of a microorganism in a diagnostic test 054845, filed on Oct. 29, 2010. sample. Methods of inhibiting microbial activity are also disclosed. In one particular example, a method of inhibiting (60) Provisional application No. 61/294,437, filed on Jan. microbial activity includes selecting a medium that is suscep 12, 2010, provisional application No. 61/259,098, tible to H1N1 influenza contamination; and contacting the filed on Nov. -

Different Antibiotic Treatments for Group a Streptococcal Pharyngitis (Review)
Different antibiotic treatments for group A streptococcal pharyngitis (Review) van Driel ML, De Sutter AIM, Keber N, Habraken H, Christiaens T This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2010, Issue 10 http://www.thecochranelibrary.com Different antibiotic treatments for group A streptococcal pharyngitis (Review) Copyright © 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 BACKGROUND .................................... 2 OBJECTIVES ..................................... 3 METHODS ...................................... 3 RESULTS....................................... 5 DISCUSSION ..................................... 8 AUTHORS’CONCLUSIONS . 11 ACKNOWLEDGEMENTS . 11 REFERENCES ..................................... 12 CHARACTERISTICSOFSTUDIES . 16 DATAANDANALYSES. 43 Analysis 1.1. Comparison 1 Cephalosporin versus penicillin, Outcome 1 Resolution of symptoms post-treatment (ITT analysis). ................................... 45 Analysis 1.2. Comparison 1 Cephalosporin versus penicillin, Outcome 2 Resolution of symptoms post-treatment (evaluable participants)................................... 46 Analysis 1.3. Comparison 1 Cephalosporin versus penicillin, Outcome 3 Resolution of symptoms within 24 hours of treatment(ITTanalysis).. 47 Analysis 1.4. Comparison 1 Cephalosporin versus penicillin, Outcome -
The Use of Natural Product Substrates for the Synthesis of Libraries of Biologically Active, New Chemical Entities
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Graduate School Professional Papers 2010 The seU of Natural Product Substrates for the Synthesis of Libraries of Biologically Active, New Chemical Entities Joshua Bryant Phillips The University of Montana Let us know how access to this document benefits ouy . Follow this and additional works at: https://scholarworks.umt.edu/etd Recommended Citation Phillips, Joshua Bryant, "The sU e of Natural Product Substrates for the Synthesis of Libraries of Biologically Active, New Chemical Entities" (2010). Graduate Student Theses, Dissertations, & Professional Papers. 1100. https://scholarworks.umt.edu/etd/1100 This Dissertation is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. THE USE OF NATURAL PRODUCT SUBSTRATES FOR THE SYNTHESIS OF LIBRARIES OF BIOLOGICALLY ACTIVE, NEW CHEMICAL ENTITIES by Joshua Bryant Phillips B.S. Chemistry, Northern Arizona University, 2002 B.S. Microbiology (health pre-professional), Northern Arizona University, 2002 Presented in partial fulfillment of the requirements for the degree of Doctor of Philosophy Chemistry The University of Montana June 2010 Phillips, Joshua Bryant Ph.D., June 2010 Chemistry THE USE OF NATURAL PRODUCT SUBSTRATES FOR THE SYNTHESIS OF LIBRARIES OF BIOLOGICALLY ACTIVE, NEW CHEMICAL ENTITIES Advisor: Dr. Nigel D. Priestley Chairperson: Dr. Bruce Bowler ABSTRACT Since Alexander Fleming first noted the killing of a bacterial culture by a mold, antibiotics have revolutionized medicine, being able to treat, and often cure life-threatening illnesses and making surgical procedures possible by eliminating the possibility of opportunistic infection. -

Anew Drug Design Strategy in the Liht of Molecular Hybridization Concept
www.ijcrt.org © 2020 IJCRT | Volume 8, Issue 12 December 2020 | ISSN: 2320-2882 “Drug Design strategy and chemical process maximization in the light of Molecular Hybridization Concept.” Subhasis Basu, Ph D Registration No: VB 1198 of 2018-2019. Department Of Chemistry, Visva-Bharati University A Draft Thesis is submitted for the partial fulfilment of PhD in Chemistry Thesis/Degree proceeding. DECLARATION I Certify that a. The Work contained in this thesis is original and has been done by me under the guidance of my supervisor. b. The work has not been submitted to any other Institute for any degree or diploma. c. I have followed the guidelines provided by the Institute in preparing the thesis. d. I have conformed to the norms and guidelines given in the Ethical Code of Conduct of the Institute. e. Whenever I have used materials (data, theoretical analysis, figures and text) from other sources, I have given due credit to them by citing them in the text of the thesis and giving their details in the references. Further, I have taken permission from the copyright owners of the sources, whenever necessary. IJCRT2012039 International Journal of Creative Research Thoughts (IJCRT) www.ijcrt.org 284 www.ijcrt.org © 2020 IJCRT | Volume 8, Issue 12 December 2020 | ISSN: 2320-2882 f. Whenever I have quoted written materials from other sources I have put them under quotation marks and given due credit to the sources by citing them and giving required details in the references. (Subhasis Basu) ACKNOWLEDGEMENT This preface is to extend an appreciation to all those individuals who with their generous co- operation guided us in every aspect to make this design and drawing successful. -

Pharmaceutical Appendix to the Tariff Schedule 2
Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACIDUM LIDADRONICUM 63132-38-7 ABAFUNGIN 129639-79-8 ACIDUM SALCAPROZICUM 183990-46-7 ABAMECTIN 65195-55-3 ACIDUM SALCLOBUZICUM 387825-03-8 ABANOQUIL 90402-40-7 ACIFRAN 72420-38-3 ABAPERIDONUM 183849-43-6 ACIPIMOX 51037-30-0 ABARELIX 183552-38-7 ACITAZANOLAST 114607-46-4 ABATACEPTUM 332348-12-6 ACITEMATE 101197-99-3 ABCIXIMAB 143653-53-6 ACITRETIN 55079-83-9 ABECARNIL 111841-85-1 ACIVICIN 42228-92-2 ABETIMUSUM 167362-48-3 ACLANTATE 39633-62-0 ABIRATERONE 154229-19-3 ACLARUBICIN 57576-44-0 ABITESARTAN 137882-98-5 ACLATONIUM NAPADISILATE 55077-30-0 ABLUKAST 96566-25-5 ACODAZOLE 79152-85-5 ABRINEURINUM 178535-93-8 ACOLBIFENUM 182167-02-8 ABUNIDAZOLE 91017-58-2 ACONIAZIDE 13410-86-1 ACADESINE 2627-69-2 ACOTIAMIDUM 185106-16-5 ACAMPROSATE 77337-76-9 -
History of Antimicrobial Agents and Resistant Bacteria
Research and Reviews History of Antimicrobial Agents and Resistant Bacteria JMAJ 52(2): 103–108, 2009 Tomoo SAGA,*1 Keizo YAMAGUCHI*2 Abstract Antimicrobial chemotherapy has conferred huge benefits on human health. A variety of microorganisms were elucidated to cause infectious diseases in the latter half of the 19th century. Thereafter, antimicrobial chemo- therapy made remarkable advances during the 20th century, resulting in the overly optimistic view that infectious diseases would be conquered in the near future. However, in response to the development of antimicrobial agents, microorganisms that have acquired resistance to drugs through a variety of mechanisms have emerged and continue to plague human beings. In Japan, as in other countries, infectious diseases caused by drug- resistant bacteria are one of the most important problems in daily clinical practice. In the current situation, where multidrug-resistant bacteria have spread widely, options for treatment with antimicrobial agents are limited, and the number of brand new drugs placed on the market is decreasing. Since drug-resistant bacteria have been selected by the use of antimicrobial drugs, the proper use of currently available antimicrobial drugs, as well as efforts to minimize the transmission and spread of resistant bacteria through appropriate infection control, would be the first step in resolving the issue of resistant organisms. Key words Antimicrobial agents, Resistant bacteria, History not achieve beneficial effect, and moreover, Introduction may lead to a worse prognosis. In addition, in a situation where multidrug-resistant organisms Antimicrobial drugs have caused a dramatic have spread widely, there may be quite a limited change not only of the treatment of infectious choice of agents for antimicrobial therapy. -

Synthetic Strategies to Combat Antibiotic Resistance
University of New Hampshire University of New Hampshire Scholars' Repository Master's Theses and Capstones Student Scholarship Winter 2018 Synthetic strategies to combat antibiotic resistance Jonathan Fifer University of New Hampshire, Durham Follow this and additional works at: https://scholars.unh.edu/thesis Recommended Citation Fifer, Jonathan, "Synthetic strategies to combat antibiotic resistance" (2018). Master's Theses and Capstones. 1262. https://scholars.unh.edu/thesis/1262 This Thesis is brought to you for free and open access by the Student Scholarship at University of New Hampshire Scholars' Repository. It has been accepted for inclusion in Master's Theses and Capstones by an authorized administrator of University of New Hampshire Scholars' Repository. For more information, please contact [email protected]. Synthetic strategies to combat antibiotic resistance BY Jonathan P. Fifer Chemistry (B.Sc), Penn State University, 2014 THESIS Submitted to the University of New Hampshire in Partial Fulfillment of the Requirements for the Degree of Master of Science In Chemistry December 2018 This thesis has been examined and approved in partial fulfillment of the requirements for the degree of Masters of Science in Chemistry. Synthetic strategies to combat antibiotic resistance BY Jonathan P. Fifer Thesis/Dissertation Director, Marc A. Boudreau, Assistant Professor of Chemistry ______________________________________ Eric B. Berda, Associate Professor of Chemistry ______________________________________ Arthur Greenburg, Professor of Chemistry ______________________________________ on December 12, 2018 Approval signatures are on file with the University of New Hampshire Graduate School. ii -TABLE OF CONTENTS- Dedication ………………………………….…………………………….……………….. iv Acknowledgements ………………………………………………………..……………… v List of Schemes …………………………………………………………….…………….. vi - vii Lists of Figures and Tables …………………….……..…………………………….……. viii Abbreviations ….……………..…………….…………………………………..………… ix - xi Abstract ………………………………………………………………………...………… xii - xiii Chapters 1. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0