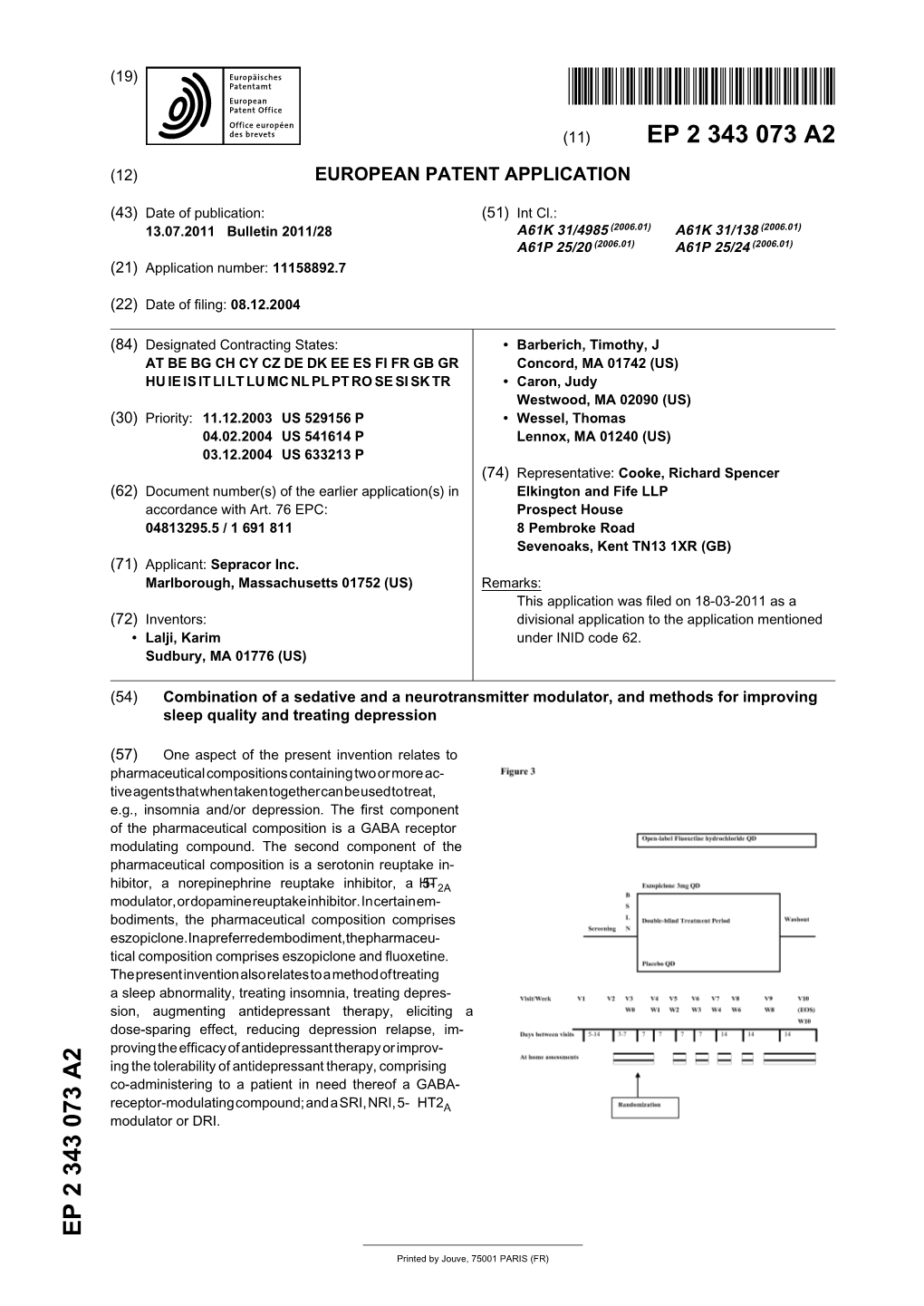
Combination of a Sedative and a Neurotransmitter Modulator, and Methods for Improving Sleep Quality and Treating Depression
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Still the Leading Antidepressant After 40
BRITISH JOURNAL OF PSYCHIATRY "2001), 178, 129^144 REVIEW ARTICLE Amitriptyline vv.therest:stilltheleading METHOD Inclusion criteria antidepressant after 40 years of randomised All RCTs comparing amitriptyline with any y other tricyclic,heterocyclic or SSRI were in- controlled trials cluded. Crossover studies were excluded. Studies adopting any criteria to define CORRADO BARBUI and MATTHEW HOTOPF patients suffering from depression were included; a concurrent diagnosis of another psychiatric disorder was not considered an exclusion criterion. Trials in patients with depression with a concomitant medical ill- Background Tricyclic antidepressants Amitriptyline is one of the first `reference' ness were not included in this review. have similar efficacy and slightly lower tricyclic antidepressants TCAs). Over the past 40 years a number of newer tricyclics, tolerability than selective serotonin Search strategy heterocyclics and selective serotonin re- Relevant studies were located by searching reuptakeinhibitorsreuptake inhibitors SSRIs).However, uptake inhibitors SSRIs) have been intro- the Cochrane Collaboration Depression, there are no systematic reviews assessing duced Garattini et aletal,1998). Despite Anxiety and Neurosis Controlled Trials several large systematic reviews comparing amitriptyline, the reference tricyclic drug, Register CCDANCTR). This specialised tricyclics and SSRIs there is no clear agree- vv. other tricyclics and SSRIs directly. register is regularly updated by electronic ment over first-line treatment of depression Medline,Embase,PsycINFO,LILACS, SongSong et aletal,1993; Anderson & Tomenson, Aims ToreviewTo review the tolerability and Psyndex,CINAHL,SIGLE) and non-electro- 1995; Montgomery & Kasper,1995; efficacy of amitriptyline inthe nicnicliterature searches. The register was HotopfHotopf et aletal,1996; Canadian Coordinating management of depression. searched using the following terms: Office for Health Technology Assessment, AMITRIPTYLIN**AMITRIPTYLIN oror AMITRILAMITRIL oror ELA-ELA- 19971997aa). -

Maturation and Development. Biological and Psychological Perspectives
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.46.4.375-b on 1 April 1983. Downloaded from Journal of Neurology, Neurosurgery, and Psychiatry 1983;46:375-376 definition by trained transcribers with an tumours in childhood. Book reviews interexaminer reliability of F = 0-81 fol- These volumes are much recommended Gilies de la Tourette Syndrome Volume 35 lowed by 2-way Anovas with blocking for to all neurosurgeons who wish to be of Advances in Neurology. Edited by subject pairs to compute F ratios for com- acquainted with the "state of play" in Arnold J Friedhoff and Thomas N Chase. paring the mean Z scores on each language paediatric neurosurgery. The editors are, (Pp 478; $58.90.) New York, Raven Press. function. This is incomprehensible as well however, very naive if they believe, as they 1982. as meaningless. It is impossible to find out suggest in their preface to volume 2, that it whether clonidine is really useful or not or may be "possible for paediatric This volume contains the proceedings of whether haloperidol does possess definite neurosurgeons throughout the entire world the 1981 New York symposium on advantages over other neuroleptics. to provide their knowledge and care to the Tourette syndrome. The 67 papers are This is the second major work on Gilles benefit of all children". At least 1000 mil- organised into 10 main sections, clinical de la Tourette's syndrome to appear in 4 lion of the world's population are provided and historical over-view, neuro-anatomy years, the first edited by the Shapiros, with very few neurosurgeons (for the and neuropathology, neurophysiology, Bruun, and Sweet. -

Pindolol of the Activation of Postsynaptic 5-HT1A Receptors
Potentiation by (-)Pindolol of the Activation of Postsynaptic 5-HT1A Receptors Induced by Venlafaxine Jean-Claude Béïque, Ph.D., Pierre Blier, M.D., Ph.D., Claude de Montigny, M.D., Ph.D., and Guy Debonnel, M.D. The increase of extracellular 5-HT in brain terminal regions antagonist WAY 100635 (100 g/kg, i.v.). A short-term produced by the acute administration of 5-HT reuptake treatment with VLX (20 mg/kg/day ϫ 2 days) resulted in a inhibitors (SSRI’s) is hampered by the activation of ca. 90% suppression of the firing activity of 5-HT neurons somatodendritic 5-HT1A autoreceptors in the raphe nuclei. in the dorsal raphe nucleus. This was prevented by the The present in vivo electrophysiological studies were coadministration of (-)pindolol (15 mg/kg/day ϫ 2 days). undertaken, in the rat, to assess the effects of the Taken together, these results indicate that (-)pindolol coadministration of venlafaxine, a dual 5-HT/NE reuptake potentiated the activation of postsynaptic 5-HT1A receptors inhibitor, and (-)pindolol on pre- and postsynaptic 5-HT1A resulting from 5-HT reuptake inhibition probably by receptor function. The acute administration of venlafaxine blocking the somatodendritic 5-HT1A autoreceptor, but not and of the SSRI paroxetine (5 mg/kg, i.v.) induced a its postsynaptic congener. These results support and extend suppression of the firing activity of dorsal hippocampus CA3 previous findings providing a biological substratum for the pyramidal neurons. This effect of venlafaxine was markedly efficacy of pindolol as an accelerating strategy in major potentiated by a pretreatment with (-)pindolol (15 mg/kg, depression. -

(12) Patent Application Publication (10) Pub. No.: US 2012/0190743 A1 Bain Et Al
US 2012O190743A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2012/0190743 A1 Bain et al. (43) Pub. Date: Jul. 26, 2012 (54) COMPOUNDS FOR TREATING DISORDERS Publication Classification OR DISEASES ASSOCATED WITH (51) Int. Cl NEUROKININ 2 RECEPTORACTIVITY A6II 3L/23 (2006.01) (75) Inventors: Jerald Bain, Toronto (CA); Joel CD7C 69/30 (2006.01) Sadavoy, Toronto (CA); Hao Chen, 39t. ii; C Columbia, MD (US); Xiaoyu Shen, ( .01) Columbia, MD (US) A6IPI/00 (2006.01) s A6IP 29/00 (2006.01) (73) Assignee: UNITED PARAGON A6IP II/00 (2006.01) ASSOCIATES INC., Guelph, ON A6IPI3/10 (2006.01) (CA) A6IP 5/00 (2006.01) A6IP 25/00 (2006.01) (21) Appl. No.: 13/394,067 A6IP 25/30 (2006.01) A6IP5/00 (2006.01) (22) PCT Filed: Sep. 7, 2010 A6IP3/00 (2006.01) CI2N 5/071 (2010.01) (86). PCT No.: PCT/US 10/48OO6 CD7C 69/33 (2006.01) S371 (c)(1) (52) U.S. Cl. .......................... 514/552; 554/227; 435/375 (2), (4) Date: Apr. 12, 2012 (57) ABSTRACT Related U.S. Application Data Compounds, pharmaceutical compositions and methods of (60) Provisional application No. 61/240,014, filed on Sep. treating a disorder or disease associated with neurokinin 2 4, 2009. (NK) receptor activity. Patent Application Publication Jul. 26, 2012 Sheet 1 of 12 US 2012/O190743 A1 LU 1750 15OO 1250 OOO 750 500 250 O O 20 3O 40 min SampleName: EM2OO617 Patent Application Publication Jul. 26, 2012 Sheet 2 of 12 US 2012/O190743 A1 kixto CFUgan <tro CFUgan FIG.2 Patent Application Publication Jul. -

Strategies for Managing Sexual Dysfunction Induced by Antidepressant Medication
King’s Research Portal DOI: 10.1002/14651858.CD003382.pub3 Document Version Publisher's PDF, also known as Version of record Link to publication record in King's Research Portal Citation for published version (APA): Taylor, M. J., Rudkin, L., Bullemor-Day, P., Lubin, J., Chukwujekwu, C., & Hawton, K. (2013). Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database of Systematic Reviews, (5). https://doi.org/10.1002/14651858.CD003382.pub3 Citing this paper Please note that where the full-text provided on King's Research Portal is the Author Accepted Manuscript or Post-Print version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version for pagination, volume/issue, and date of publication details. And where the final published version is provided on the Research Portal, if citing you are again advised to check the publisher's website for any subsequent corrections. General rights Copyright and moral rights for the publications made accessible in the Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognize and abide by the legal requirements associated with these rights. •Users may download and print one copy of any publication from the Research Portal for the purpose of private study or research. •You may not further distribute the material or use it for any profit-making activity or commercial gain •You may freely distribute the URL identifying the publication in the Research Portal Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

624.Full.Pdf
1521-009X/44/5/624–633$25.00 http://dx.doi.org/10.1124/dmd.115.068932 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 44:624–633, May 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Development of a Rat Plasma and Brain Extracellular Fluid Pharmacokinetic Model for Bupropion and Hydroxybupropion Based on Microdialysis Sampling, and Application to Predict Human Brain Concentrations Thomas I.F.H. Cremers, Gunnar Flik, Joost H.A. Folgering, Hans Rollema, and Robert E. Stratford, Jr. Brains On-Line BV, Groningen, The Netherlands (T.I.F.H.C., G.F. J.H.A.F.); Rollema Biomedical Consulting, Mystic, Connecticut (H.R.); and Division of Pharmaceutical Sciences, Mylan School of Pharmacy, Duquesne University, Pittsburgh, Pennsylvania (R.E.S.) Received December 11, 2015; accepted February 24, 2016 Downloaded from ABSTRACT Administration of bupropion [(6)-2-(tert-butylamino)-1-(3-chlorophenyl) concentration ratio at early time points was observed with propan-1-one] and its preformed active metabolite, hydroxybupropion bupropion; this was modeled as a time-dependent uptake clear- [(6)-1-(3-chlorophenyl)-2-[(1-hydroxy-2-methyl-2-propanyl)amino]- ance of the drug across the blood–brain barrier. Translation of the 1-propanone], to rats with measurement of unbound concentrations model was used to predict bupropion and hydroxybupropion dmd.aspetjournals.org by quantitative microdialysis sampling of plasma and brain extra- exposure in human brain extracellular fluid after twice-daily cellular fluid was used to develop a compartmental pharmacoki- administration of 150 mg bupropion. Predicted concentrations netics model to describe the blood–brain barrier transport of both indicate that preferential inhibition of the dopamine and norepi- substances. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

(12) United States Patent (10) Patent No.: US 8,580,832 B2 Gaul Et Al
USOO858O832B2 (12) United States Patent (10) Patent No.: US 8,580,832 B2 Gaul et al. (45) Date of Patent: Nov. 12, 2013 (54) SUBSTITUTED PHENOXY Pacifici, R.J., “Estrogen, Cytokines, and Pathogenesis of AMINOTHAZOLONES AS ESTROGEN Postmenopausal Osteoporosis.”. Bone Miner. Res., 1996, vol. 11 (8), RELATED RECEPTOR-O MODULATORS pp. 1043-1051. International Search Report, PCT/US2008/056029, date of mailing (75) Inventors: Michael Gaul, Yardley, PA (US); of International Search Repont, Jul. 4, 2008. Alexander Kim, Levittown, PA (US); Written Opinion relating to PCT/US2008/056029. Lily Lee Searle, Waltham, MA (US); Strum et al., “Rosiglitazone Induces Mitochondrial Biogenesis in Dionisios Rentzeperis, Downingtown, Mouse Brain”, Journal of Alzheimer's Disease, 2007, vol. 11(1), pp. PA (US); Gilles C. Bignan, Brigewater, 45-51, IOS Press, Asterdam, NL. NJ (US) Grundy, S., et al. “Definition of Metabolic Syndrome'. Circulation 2004:109:433-438. (73) Assignee: Janssen Pharmaceutica N.V. (BE) Kamei, Y, et al. “PPARY Coactivator 13/ERR Ligand 1 is an ERR Protein Ligand, Whose Expression Induces a High-Energy Expendi (*) Notice: Subject to any disclaimer, the term of this ture and Antagonizes Obesity”, PNAS, vol. 100, No. 21, 2003, pp. patent is extended or adjusted under 35 12378-12383. U.S.C. 154(b) by 768 days. Jones, P. et al. “N-CoR-HDAC Corepressor Complexes: Roles in Transcriptional Regulation by Nuclear Hormone Receptors', Chap (21) Appl. No.: 12/043,311 ter 9, Curr. Top. Microbiol. Immunol. 2003, 274, pp. 237-268. Luo, J., et al. “Reduced Fat Mass in Mice Lacking Orphan Nuclear (22) Filed: Mar. -

Evaluation of Antidepressant-Related Behavioral Responses in Mice Lacking the Serotonin Transporter Andrew Holmes, Rebecca J
Evaluation of Antidepressant-related Behavioral Responses in Mice Lacking the Serotonin Transporter Andrew Holmes, Rebecca J. Yang, Dennis L. Murphy, and Jacqueline N. Crawley Inhibition of the serotonin transporter (5-HTT) is a 5-HTT Ϫ/Ϫ mice on the C57BL/6J background showed no principal initial target of many antidepressants. However, baseline antidepressant-related phenotype on either test. the contribution of the 5-HTT to their therapeutic efficacy is The behavioral effects of three antidepressants were tested in incompletely understood. We utilized a targeted gene 5-HTT mutant mice (C57BL/6J background) in the tail mutation approach to examine the role of the 5-HTT in the suspension test. The anti-immobility effects of the serotonin behavioral actions of antidepressants. The 5-HTT mutation reuptake inhibitor, fluoxetine (30 mg/kg), were abolished in was bred onto two separate genetic backgrounds, C57BL/6J 5-HTT Ϫ/Ϫ mice, confirming that the 5-HTT gene is and 129S6. On a preliminary screen for gross physical, required for the behavioral effects of fluoxetine. In contrast, neurological and behavioral functions, all measures were 5-HTTϪ/Ϫ mice retained sensitivity to the anti-immobility normal with the exception that 5-HTT Ϫ/Ϫ mice on the effects of the norepinephrine reuptake inhibitor, desipramine C57BL/6J background showed increased body weight and (20 mg/kg), and the mixed serotonin/norepinephrine poor rotarod performance, and 5-HTT Ϫ/Ϫ mice on the reuptake inhibitor, imipramine (25 mg/kg). 5-HTT 129S6 background showed reduced neuromuscular knockout mice provide a valuable tool for delineating the strength. On the tail suspension test, 5-HTT Ϫ/Ϫ mice on neuropsychopharmacological actions of antidepressants. -

Characterization and Localization of a Peripheral Neural 5Hydroxytryptamine Receptor Subtype (5=HT,,) with a Selective Agonist, 3H-5-Hydroxyindalpine
The Journal of Neuroscience, July 1988, 8(7): 2582-2595 Characterization and Localization of a Peripheral Neural 5Hydroxytryptamine Receptor Subtype (5=HT,,) with a Selective Agonist, 3H-5-Hydroxyindalpine Theresa A. Branchek, Gary M. Mawe, and Michael D. Gershon Department of Anatomy and Cell Biology, Columbia University, College of Physicians and Surgeons, New York, New York 10032 Peripheral neural 5hydroxytryptamine (5HT) receptors are (5-HTP-DP), that antagonize the binding of 3H-5-HT to enteric different from both classes 5-HT, and 5-HT,, which have membranes or tissue sections. It is concluded that 5-OHIP been described from studies of 5-HT receptors in the brain. is an agonist at peripheral neural 5-HT,, receptors and can Recently, it has been shown that, as in the CNS, there is be used to label these receptors selectively outside the brain. more than a single type of neural receptor for 5-HT in the Radioautographs demonstrated enteric 5-HT,, receptors in enteric nervous system. One of these, called 5-HT,,, has a the lamina propria of the intestinal mucosa and in the sub- high affinity for 3H-5-HT, initiates a long-lasting depolariza- mucosal and myenteric plexuses. Extraenteric 5-HT,, re- tion of enteric neurons associated with an increase in mem- ceptors were also found in the skin and heart. It is suggested brane resistance, and is the physiological receptor through that 5-HT,, receptors may be found on subtypes of primary which enteric serotoninergic neurons mediate slow EPSPs. afferent nerve fibers. The other receptor, called 5-HT, (5-HT,,), does not bind 3H- 5-HT with high affinity, and initiates a brief depolarization of Serotonin (5hydroxytryptamine, 5-HT) is found in both the enteric neurons with decreased input resistance, but a phys- wall and the lining epithelium of the gastrointestinal tract. -

Among a Series of Novel D4 Dopamine Receptor Agonists and Antagonists Jeremiah J
Topographically Based Search for an “Ethogram” Among a Series of Novel D4 Dopamine Receptor Agonists and Antagonists Jeremiah J. Clifford, Ph.D., and John L. Waddington, Ph.D., D.Sc. The effects of three selective D4 antagonists [CP-293,019, 25.0 mg/kg) failed to influence any behavior; whereas, PD L-745,870, and Ro 61-6270] and two putative selective D4 168077 (0.2–25.0 mg/kg) induced nonstereotyped shuffling agonists [CP-226,269 and PD 168077] were compared with locomotion with uncoordinated movements, jerking, and those of the generic D2-like [D2L/S,D3, D4] antagonist yawning, which were insensitive to antagonism by haloperidol to identify any characteristic “ethogram,” in CP-293,019, L-745,870, or haloperidol. These findings fail terms of individual topographies of behavior within the to indicate any “ethogram” for selective manipulation of D4 natural rodent repertoire, as evaluated using ethologically receptor function at the level of the interaction between based approaches. Among the D4 antagonists, neither motoric and psychological processes in sculpting behavioral L-745,870 (0.0016–1.0 mg/kg) nor Ro 61-6270 (0.2–25.0 topography over habituation of exploration through to mg/kg) influenced any behavior; whereas, CP-293,019 quiescence and focus attention on social, cognitive, or other (0.2–25.0 mg/kg) induced episodes of nonstereotyped levels of examination. sniffing, sifting, and vacuous chewing; there were no [Neuropsychopharmacology 22:538–544, 2000] consistent effects on responsivity to the D2-like agonist RU © 2000 American College of Neuropsychopharmacology. 24213. Among the putative D4 agonists, CP-226,269 (0.2– Published by Elsevier Science Inc.