Surgical Procedure Terms and Definitions All Surgeries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Management of Transcatheter Heart Valves
Corporate Medical Policy Surgical Management of Transcatheter Heart Valves File Name: surgica l_management_of_transcatheter_heart_valves Origination: 1/2011 Last CAP Review: 6/2021 Next CAP Review: 6/2022 Last Review: 6/2021 Description of Procedure or Service As the proportion of older adults increases in the U.S. population, the incidence of degenerative heart valve disease also increases. Aortic stenosis and mitra l regurgita tion are the most common valvular disorders in adults aged 70 years and older. For patients with severe valve disease, heart valve repair or replacement involving open heart surgery can improve functional status and qua lity of life. A variety of conventional mechanical and bioprosthetic heart valves are readily available. However, some individuals, due to advanced age or co-morbidities, are considered too high risk for open heart surgery. Alternatives to the open heart approach to heart valve replacement are currently being explored. Transcatheter heart valve replacement and repair are relatively new interventional procedures involving the insertion of an artificial heart valve or repair device using a catheter, rather than through open heart surgery, or surgical valve replacement (SAVR). The point of entry is typically either the femoral vein (antegrade) or femora l artery (retrograde), or directly through the myocardium via the apical region of the heart. For pulmonic and aortic valve replacement surgery, an expandable prosthetic heart valve is crimped onto a catheter and then delivered and deployed at the site of the diseased native valve. For valve repair, a small device is delivered by catheter to the mitral valve where the faulty leaflets are clipped together to reduce regurgitation. -

The Conversion to Rastelli's Type Operation from Patrick-Mcgoon's
General Thoracic and Cardiovascular Surgery (2019) 67:551–553 https://doi.org/10.1007/s11748-018-0942-x CASE REPORT The conversion to Rastelli’s type operation from Patrick-McGoon’s procedure of an adult with Taussig–Bing heart: a case report Keiichi Fujiwara1 · Kousuke Yoshizawa1 · Nobuhisa Ohno1 · Hisanori Sakazaki2 Received: 30 January 2018 / Accepted: 18 May 2018 / Published online: 11 June 2018 © The Japanese Association for Thoracic Surgery 2018 Abstract A 23-year-old female of Taussig–Bing heart with antero-posterior relation of the great arteries was underwent Patrick- McGoon’s intraventricular rerouting at 6 years old of age. The left ventricular outflow obstruction (peak pressure gradient of 100 mmHg) developed, and severe aortic valve regurgitation following bacterial endocarditis was noted. The conversion to Rastelli’s type operation and aortic valve replacement were performed successfully at 23 years old of age. She is doing well without any significant left or right ventricular outflow obstruction at 7 years postoperatively. Keywords Taussig–Bing heart · Intraventricular rerouting · Patrick-McGoon’s operation · Left ventricular outflow obstruction · Adult congenital heart disease Introduction Case Taussig–Bing heart is characterized by double-outlet right A 23-year-old female diagnosed of double outlet right ventricle with subpulmonary ventricular septal defect [1, 2]. ventricle with subpulmonary ventricular septal defect and Currently, the arterial switch procedure as anatomic repair, antero-posterior relation of the great arteries, was referred to connecting the left ventricle to aorta and the right ventricle our hospital for severe left ventricular outflow tract obstruc- to pulmonary artery, is a popular surgical management for tion following Patrick-McGoon’s intraventricular rerouting Taussig–Bing heart regardless of relation of the great arter- and moderate to severe aortic valve regurgitation following ies. -

The Arterial Switch Operation for Transposition of the Great Arteries
The Arterial Switch Operation for Transposition of the Great Arteries Richard A. Jonas Transposition of the great arteries, together with tetral- Ijased on the fact that (luring fetal life hoth ventricles ogy of Fallot, is one of the most common congenital are exposed to the same pressure load. Thus, the left cardiac anomalies resulting in cyanosis. It is hardly ventricle is prepared at birth. However, hecause pulnio- surprising, therefore, that shortly after the introduc- nary resistance falls ra1)idlj within 6 to 8 weeks ancl tion of cardiopulmonary hypass in the early 195Os, perhaps as quicltly as within 2 to 4 weeks, the left attempts were made at anatomical correction of transpo- ventricle is no longer prepared. Iiitroduction of an sition, ie, the arterial switch procedure. These early essentially elective complex neonatal operation in 1983 attempts were uniformly unsuccessful for a number of initially met with consitlerahle resistance, particularly reasons : 1)ecause hy this time the surgical mortality for the atrial 1. Microvascular techniques were not adequately level procedures had reached very low levels. However, developed for delicate coronary artery transfer. a prospectivr study conducted Ijy the Congenital Heart 2. Pulmonary vascular disease is common in transpo- Surgeons Society‘ showed that the overall survival of an sition beyond the first year of life. entire population of patients with transposition en- 3. Surgeons failed to appreciate that in the presence rolled in the neonatal period was superior with the of an intact ventricular septum, the left ventricle was neonatal arterial switch approach because of the previ- inadequately prepared to acntely take over the pressure ously uncaptured deaths that occurred before atrial load of the systemic circulation. -

Positive Maternal and Foetal Outcomes After Cardiopulmonary Bypass Surgery
Case Study: Positive maternal and foetal outcomes after cardiopulmonary bypass surgery Positive maternal and foetal outcomes after cardiopulmonary bypass surgery in a parturient with severe mitral valve disease aMokgwathi GT, MBChB aLebakeng EM, MBChB, DA(SA), MMed(Anaes) bOgunbanjo GA, MBBS, FCFP(SA), MFamMed, FACRRM, FACTM, FAFP(SA), FWACP(Fam Med) aDepartment of Anaesthesiology, University of Limpopo (Medunsa Campus) bDepartment of Family Medicine and Primary Health Care, University of Limpopo (Medunsa Campus) Correspondence to: Dr GT Mokgwathi, e-mail: [email protected] Keywords: anaesthesia, cardiac surgery, parturient, cardiopulmonary bypass surgery, mitral valve replacement Abstract This case study describes the successful management of a parturient with severe mitral stenosis and moderate mitral regurgitation who underwent cardiopulmonary bypass (CPB) surgery. A healthy baby was delivered by Caesarean section 11 days later. The effects of CPB surgery and mitral valve replacement on parturient and foetus are discussed. Peer reviewed. (Submitted: 2011-01-04, Accepted: 2011-06-16) © SASA South Afr J Anaesth Analg 2011;17(4):299-302 Introduction she was classified as New York Heart Association (NYHA) class III and World Health Organization (WHO) heart Heart disease is the primary cause of nonobstetric mortality failure stage C. Her blood pressure was 90/60 mmHg in pregnancy, occurring in 1-4 % of pregnancies1-3 and and her heart rate was 82 beats per minute and regular. accounting for 10–15 % of maternal mortality in developed She had a tapping apex beat, loud first heart sound, loud countries.1,2 Cardiac disease contributes to 40.2% of pulmonary component of the second heart sound and a maternal deaths in South Africa.4 Soma-Pillay et al noted grade 3/4 diastolic murmur heard loudest at the apex. -

Heart Valve Disease: Mitral and Tricuspid Valves
Heart Valve Disease: Mitral and Tricuspid Valves Heart anatomy The heart has two sides, separated by an inner wall called the septum. The right side of the heart pumps blood to the lungs to pick up oxygen. The left side of the heart receives the oxygen- rich blood from the lungs and pumps it to the body. The heart has four chambers and four valves that regulate blood flow. The upper chambers are called the left and right atria, and the lower chambers are called the left and right ventricles. The mitral valve is located on the left side of the heart, between the left atrium and the left ventricle. This valve has two leaflets that allow blood to flow from the lungs to the heart. The tricuspid valve is located on the right side of the heart, between the right atrium and the right ventricle. This valve has three leaflets and its function is to Cardiac Surgery-MATRIx Program -1- prevent blood from leaking back into the right atrium. What is heart valve disease? In heart valve disease, one or more of the valves in your heart does not open or close properly. Heart valve problems may include: • Regurgitation (also called insufficiency)- In this condition, the valve leaflets don't close properly, causing blood to leak backward in your heart. • Stenosis- In valve stenosis, your valve leaflets become thick or stiff, and do not open wide enough. This reduces blood flow through the valve. Blausen.com staff-Own work, CC BY 3.0 Mitral valve disease The most common problems affecting the mitral valve are the inability for the valve to completely open (stenosis) or close (regurgitation). -

A Study on Pattern of Heart Disease and Maternal and Fetal Outcome Of
University Heart Journal Vol. 11, No. 1, January 2015 A Study on Pattern of Heart Disease and Maternal and Fetal Outcome of Pregnancy in a Tertiary Level Hospital NAHREEN AKHTAR1 , TAJMIRA SULTANA1, SYEDA SAYEEDA2, TABASSUM PARVEEN1,FIROZA BEGUM1 1Fetomaternal Medicine Wing, Dept of Obs & Gynae, Bangabandhu Sheikh Mujib Medical University, Dhaka, 2Dept of Obs & Gynae, Bangabandhu Sheikh Mujib Medical University, Dhaka. Address for Correspondence: Dr Nahreen Akhtar Professor, Fetomaternal Medicine wing, Department of Obstetric & Gynaecology. Bangabandhu Sheikh Mujib Medical University, Dhaka. E-mail – nahreenakhtar10@g mail.com Abstract: Background: Cardiac disease is the most common cause of indirect maternal deaths and the most common cause of death overall. It complicates 1% of maternal death. Objective: Management of pregnancy in patients with valvular heart disease continues to pose a challenge to the clinician.the present study was therefore design to find the pattern of Heart Disease and to evaluate the maternal and fetal outcome of pregnancy. Method: This is a cross sectional study done during the period Jan to Dec, 2011in fetomaternal medicine wing of department of Obs & Gynae, BSMMU. All the patients admitted with heart disease in pregnancy during this study period were included in this study. This study prospectively enrolled 54 pregnant women with heart disease.All cases were followed during pregnancy , labour, delivery and in early puerperium. Results: The mean (SD±) age of the patients was 26.08 ± 3.96 ranging from 20 to 35yrs, most ( 26% ) belonged to age group 26 - 30yrs and five (9.26% ) belonged to >30years of age group. Most of the patients 21 (38.89%) were primigravid and 16(29.63%) patients were of second gravida. -

World Journal for Pediatric & Congenital Heart Surgery
World Journal for Pediatric & Congenital Heart Surgery Keywords List A __________________________________________________________________________________ Ablative therapy (all modalities) Acute respiratory distress syndrome (ARDS) Adult Adult Congenital Heart Disease Airway Allograft, homograft Anastomosis Anatomy Anesthesia (includes agents, pharmacology, care and research) Aneurysm (aortic, myocardial, other) Angiogenesis Angiography Angioplasty Angioplasty (balloon dilatation) Animal model Annuloplasty (indicate location) Antibiotics Antibody/antigen Aorta/aortic Aortic arch Aortic dissection (includes ulcers, hematomas) Aortic operation Aortic root Aortic valve, repair Aortic valve, replacement Apoptosis Arrhythmia Arrhythmia surgery (includes Maze) Arterial switch operation Artery/arteries Artificial organs Atherosclerosis Atrial fibrillation, flutter Atrial Septal Defect (ASD) Atrio-ventricular Septal Defect (AVSD) Atrium Autograft Autonomic nervous system B __________________________________________________________________________________ Biochemistry Bioengineering Biomaterials Biopsy (indicate tissue) Blood Blood conservation Blood substitutes Blood transfusion Blood, coagulation/anticoagulation Brain Bronchial arteries Bronchiolitis obliterans Bronchoscopy/bronchus C __________________________________________________________________________________ Calcification Cardiac (use in combination) Cardiac anatomy/pathologic anatomy Cardiac catheterization/intervention Cardiac function Cardiac tumors (includes myxoma, primary, metastases) -

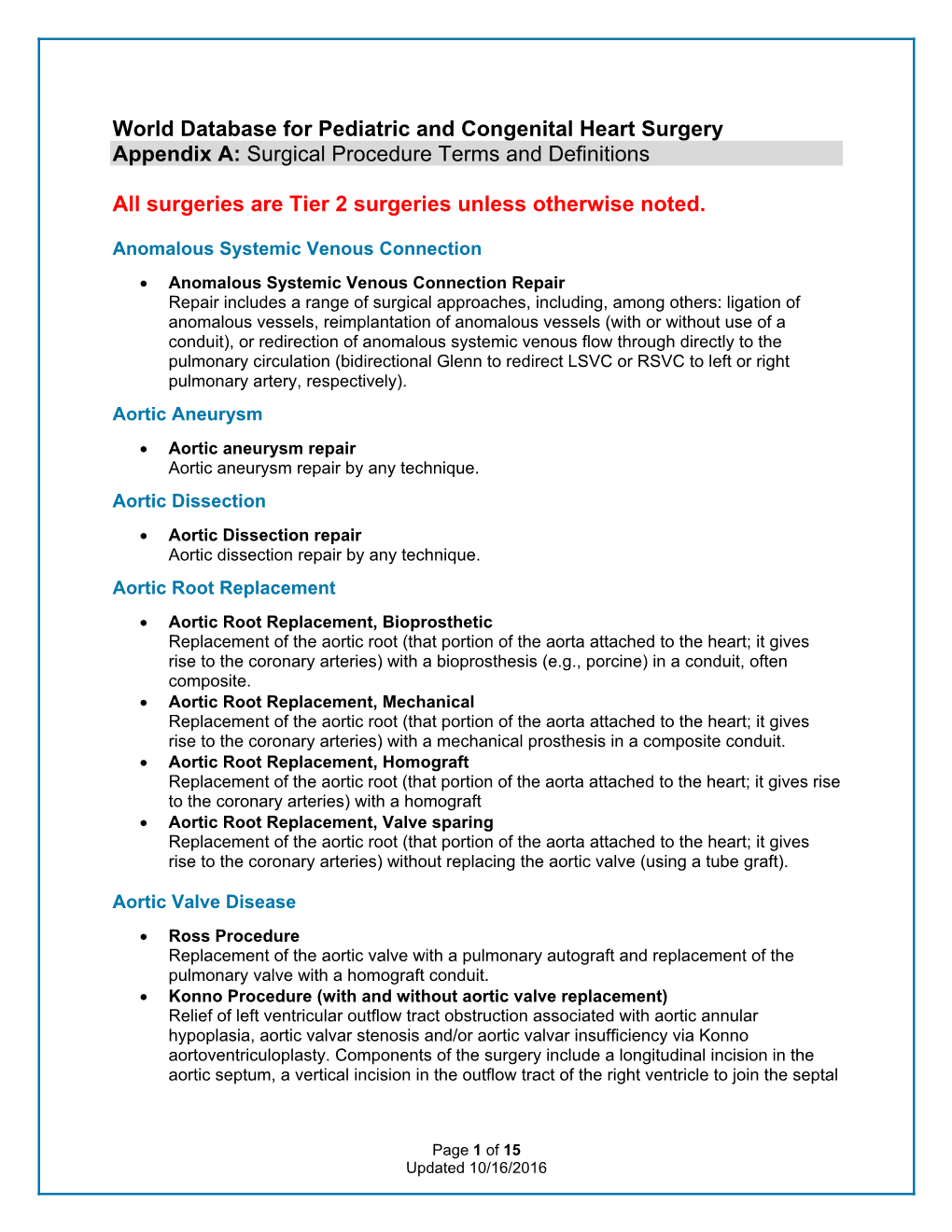
Appendix A: Surgical Procedure Terms and Definitions
Appendix A: Surgical Procedure Terms and Definitions Anomalous Systemic Venous Connection Anomalous Systemic Venous Connection Repair Repair includes a range of surgical approaches, including, among others: ligation of anomalous vessels, reimplantation of anomalous vessels (with or without use of a conduit), or redirection of anomalous systemic venous flow through directly to the pulmonary circulation (bidirectional Glenn to redirect LSVC or RSVC to left or right pulmonary artery, respectively). Aortic Aneurysm Aortic aneurysm repair Aortic aneurysm repair by any technique. Aortic Dissection Aortic Dissection repair Aortic dissection repair by any technique. Aortic Root Replacement Aortic Root Replacement, Bioprosthetic Replacement of the aortic root (that portion of the aorta attached to the heart; it gives rise to the coronary arteries) with a bioprosthesis (e.g., porcine) in a conduit, often composite. Aortic Root Replacement, Mechanical Replacement of the aortic root (that portion of the aorta attached to the heart; it gives rise to the coronary arteries) with a mechanical prosthesis in a composite conduit. Aortic Root Replacement, Homograft Replacement of the aortic root (that portion of the aorta attached to the heart; it gives rise to the coronary arteries) with a homograft Aortic Root Replacement, Valve sparing Replacement of the aortic root (that portion of the aorta attached to the heart; it gives rise to the coronary arteries) without replacing the aortic valve (using a tube graft). Aortic Valve Disease Ross Procedure Replacement of the aortic valve with a pulmonary autograft and replacement of the pulmonary valve with a homograft conduit. Konno Procedure (with and without aortic valve replacement) Relief of left ventricular outflow tract obstruction associated with aortic annular hypoplasia, aortic valvar stenosis and/or aortic valvar insufficiency via Konno aortoventriculoplasty. -

Fellow in Training Research Abstracts Oral Competition Indiana-ACC Poster Competition Abstract
Fellow in Training Research Abstracts Oral Competition Indiana-ACC Poster Competition Abstract Do NOT write outside the boxes. Any text or images outside the boxes will be deleted. Do NOT alter this form by deleting parts of it (including this text) or adding new boxes. Please structure your clinical research abstract using the following headings: * Background * Objective * Methods * Results (if relevant) * Conclusion Please structure your case study abstract using the following headings: * Introduction/objective * Case presentation * Discussion * Conclusion Title: Multi-Disciplinary Team Approach to Cardiogenic Shock Reduces In-Hospital Mortality Abstract: (Your abstract must use Normal style and must fit into the box. You may not alter the size of this ) Purpose: To determine the effectiveness of a hospital-wide process improvement program labeled as level 1 cardiogenic shock rapid response that enables a concerted coordinated multi-disciplinary team approach to treatment of patients with cardiogenic shock. Methods: Conducted a retrospective analysis of the cardiogenic shock rapid response program (protocol group) comparing to similar cohort of cardiogenic shock patients who did not utilize the shock response program. The program required alerting the advanced heart failure trained cardiologist who advises activation of a burst page to the cardiogenic shock team. This team rapidly institutes protocol-directed therapy and use of advanced support devices if necessary. The primary endpoint was hospital mortality. Secondary endpoint was utilization of advanced therapy (temporary mechanical circulatory support) Results: 471 patients were in the control and 110 in the protocol group. Baseline characteristics were similar and etiology of cardiogenic shock. The protocol group had significant reductions in-hospital mortality (35% to 45% (p< 0.05). -

Minimally Invasive Concomitant Aortic and Mitral Valve Surgery: the “Miami Method”
Keynote Lecture Series Minimally invasive concomitant aortic and mitral valve surgery: the “Miami Method” Joseph Lamelas Division of Cardiac Surgery, Mount Sinai Medical Center, Miami Beach, Florida, USA Correspondence to: Joseph Lamelas, M.D. Chief of Cardiothoracic Surgery, Mount Sinai Medical Center, Mount Sinai Heart Institute 4300 Alton Road, Miami Beach, Florida 33140, USA. Email: [email protected]. Valve surgery via a median sternotomy has historically been the standard of care, but in the past decade various minimally invasive approaches have gained increasing acceptance. Most data available on minimally invasive valve surgery has generally involved single valve surgery. Therefore, robust data addressing surgical techniques in patients undergoing double valve surgery is lacking. For patients undergoing combined aortic and mitral valve surgery, a minimally invasive approach, performed via a right lateral thoracotomy (the “Miami Method”), is the preferred method at our institution. This method is safe and effective and leads to an enhanced recovery in our patients given the reduction in surgical trauma. The following perspective details our surgical approach, concepts and results for combined aortic and mitral valve surgery. Keywords: Minimally invasive; valve surgery; aortic valve replacement; mitral valve surgery; double valve surgery Submitted Jun 21, 2014. Accepted for publication Jul 17, 2014. doi: 10.3978/j.issn.2225-319X.2014.08.17 View this article at: http://dx.doi.org/10.3978/j.issn.2225-319X.2014.08.17 Introduction Technique for minimally invasive aortic and mitral valve surgery Minimally invasive valve surgery was first performed by Navia et al. in 1996, and by Cohn et al. in 1997 (1,2). -

Risk Factors of Chronic Left Ventricular Dysfunction After Cardiac Valve Surgery
4859 Original Article Risk factors of chronic left ventricular dysfunction after cardiac valve surgery Xingli Fan#, Yangfeng Tang#, Guanxin Zhang#, Jiajun Zhang, Qing Xue, Boyao Zhang, Zhiyun Xu, Lin Han Department of Cardiovascular Surgery, Changhai Hospital, Naval Medical University, Shanghai, China Contributions: (I) Conception and design: L Han; (II) Administrative support: Z Xu; (III) Provision of study materials or patients: L Han, Z Xu; (IV) Collection and assembly of data: X Fan, Y Tang, G Zhang; (V) Data analysis and interpretation: X Fan, B Zhang, Q Xue, J Zhang; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. #These authors contributed equally to this work. Correspondence to: Lin Han. Department of Cardiovascular Surgery, Changhai Hospital, Naval Medical University, Shanghai, China. Email: [email protected]. Background: To analyze the risk factors of chronic left ventricular dysfunction (LVD) after cardiac valve surgery. Methods: A retrospective analysis of 860 patients who underwent heart valve surgery in our center from January 2017 to December 2018, including 650 males and 210 females, aged 58±5.8 years. Inclusion criteria: (I) the patient was clinically diagnosed with heart valve disease and met the surgical indications for mitral valve replacement (MVR), mitral valve repair (MVP), aortic valve replacement (AVR) and double valve replacement (DVR); (II) if atrial fibrillation, coronary artery disease, and tricuspid regurgitation are combined before surgery, radiofrequency ablation, coronary bypass and tricuspid angioplasty were performed contemporarily. Exclusion criteria: (I) preoperative LVEF <50%; (II) aortic dissection underwent Bentall and right heart valve replacement procedures; (III) cardiopulmonary resuscitation and death during perioperative period and 6 months after operation; (IV) postoperative CRRT, IABP, or ECMO assistance; (V) postoperative cardiac dysfunction due to valvular dysfunction, perivalvular leak, or infective endocarditis. -

Quantitative Electrocardiography for Prediction Of
QUANTITATIVE ELECTROCARDIOGRAPHY FOR PREDICTION OF POSTOPERATIVE ATRIAL FIBRILLATION AFTER CARDIAC SURGERY by FLORIAN RADER, M.D. Submitted in partial fulfillment of the requirements For the degree of Master of Science Clinical Research Scholars Program CASE WESTERN RESERVE UNIVERSITY January 2010 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the thesis/dissertation of Florian Rader, M.D. candidate for the Master of Science degree*. (signed) Regis E. McFadden (chair of the committee) Eugene H. Blackstone, M.D. Ottorino Costantini, M.D. Neal Dawson, M.D. (date) 10-28-2009 *We also certify that written approval has been obtained for any proprietary material contained therein. 2 Table of Contents List of Tables 4 List of Figures 5 Acknowledgments 6 List of Abbreviations 7 Abstract 9 Text Background and Significance 10 Specific aims 12 Methods 13 Results 21 Discussion 46 Limitations 54 Conclusions 54 References 55 3 List of Tables: Table 1: Patient characteristics 24 Table 2: Clinical predictors of postoperative atrial fibrillation 37 Table 3: ECG predictors of postoperative atrial fibrillation 38 4 List of Figures: Figure 1: Relationship of anatomic and ECG changes with POAF 11 Figure 2: Patient flow chart 22 Figure 3: Occurrence of POAF by days after surgery 33 Figure 4: Occurrence of POAF by surgery type 34 Figure 5: ROC curve of final prediction model 35 Figure 6: Calibration curve of final prediction model 36 Figure 7: Adjusted Co-plots of ECG predictors 39 Figure 8: Unadjusted and adjusted co-plot of P wave amplitude 41 Figure 9: Nomogram of final prediction model 42 Figure 10: Nomogram of prediction model with pre-op variables 43 Figure 11: Calibration curve of model without ECG predictors 45 Figure 12: Left atrial sizes by P wave amplitude in aVR 48 Figure 13: Correlation matrix (P wave amplitude, aVR, and left atrial volume) 49 5 Acknowledgments: I thank Dr.