Acid Base Balance and Blood Gas Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Versus Laboratory for Estimating of Dehydration Severity
Clinical versus laboratory for estimating of dehydration severity Majid Malaki Pediatric Health Research Center, Tabriz Medical University, Tabriz, Iran ABSTRACT Background: Acute gastroenteritis is a common cause of dehydration and precise estimation of dehydration Materials and Methods: D is a vital matter for clinical decisions. We try to find how much clinically diagnosed scales are compatible with ORIGINAL ARTICLE laboratory tests measures. uring 2 years 95 infants and children aged between 2 and 108 months entered to emergency room with acute gastroenteritis. They were categorized as mild, moderate and severe dehydration, their recorded laboratory tests include blood urea nitrogen (BUN), creatinine, venous blood gases values were expressedP by means ±95% of confidence intervalResult and compared by mann-whitney test in each groups with SPSS 16, sensitivity, specificity and likelihood ratio measured for defined cut off values in severe dehydration group, value less than 0.05 was significant. : Severe dehydration includes 3% Conclusionof all hospitalization: R due to dehydration. Laboratory tests cannot differentiate mild to moderate dehydration definietly but this difference is significant between severe to mild and severe to moderate dehydration. outine laboratory test are not generally helpful for dehydration severity estimation but they can be discriminate severe from mild or moderate dehydration exclusively. Creatinine higher than 0.9 mg/dl and BaseKey words deficit: beyond-16A are specific (90%) for severe dehydration estimation -
Cardiovascular System 9
Chapter Cardiovascular System 9 Learning Outcomes On completion of this chapter, you will be able to: 1. State the description and primary functions of the organs/structures of the car- diovascular system. 2. Explain the circulation of blood through the chambers of the heart. 3. Identify and locate the commonly used sites for taking a pulse. 4. Explain blood pressure. 5. Recognize terminology included in the ICD-10-CM. 6. Analyze, build, spell, and pronounce medical words. 7. Comprehend the drugs highlighted in this chapter. 8. Describe diagnostic and laboratory tests related to the cardiovascular system. 9. Identify and define selected abbreviations. 10. Apply your acquired knowledge of medical terms by successfully completing the Practical Application exercise. 255 Anatomy and Physiology The cardiovascular (CV) system, also called the circulatory system, circulates blood to all parts of the body by the action of the heart. This process provides the body’s cells with oxygen and nutritive ele- ments and removes waste materials and carbon dioxide. The heart, a muscular pump, is the central organ of the system. It beats approximately 100,000 times each day, pumping roughly 8,000 liters of blood, enough to fill about 8,500 quart-sized milk cartons. Arteries, veins, and capillaries comprise the network of vessels that transport blood (fluid consisting of blood cells and plasma) throughout the body. Blood flows through the heart, to the lungs, back to the heart, and on to the various body parts. Table 9.1 provides an at-a-glance look at the cardiovascular system. Figure 9.1 shows a schematic overview of the cardiovascular system. -
Oxygen Concentration of Blood: PO
Oxygen Concentration of Blood: PO2, Co-Oximetry, and More Gary L. Horowitz, MD Beth Israel Deaconess Medical Center Boston, MA Objectives • Define “O2 Content”, listing its 3 major variables • Define the limitations of pulse oximetry • Explain why a normal arterial PO2 at sea level on room air is ~100 mmHg (13.3 kPa) • Describe the major features of methemogobin and carboxyhemglobin O2 Concentration of Blood • not simply PaO2 – Arterial O2 Partial Pressure ~100 mm Hg (~13.3 kPa) • not simply Hct (~40%) – or, more precisely, Hgb (14 g/dL, 140 g/L) • not simply “O2 saturation” – i.e., ~89% O2 Concentration of Blood • rather, a combination of all three parameters • a value labs do not report • a value few medical people even know! O2 Content mm Hg g/dL = 0.003 * PaO2 + 1.4 * [Hgb] * [%O2Sat] = 0.0225 * PaO2 + 1.4 * [Hgb] * [%O2Sat] kPa g/dL • normal value: about 20 mL/dL Why Is the “Normal” PaO2 90-100 mmHg? • PAO2 = (FiO2 x [Patm - PH2O]) - (PaCO2 / R) – PAO2 is alveolar O2 pressure – FiO2 is fraction of inspired oxygen (room air ~0.20) – Patm is atmospheric pressure (~760 mmHg at sea level) o – PH2O is vapor pressure of water (47 mmHg at 37 C) – PaCO2 is partial pressure of CO2 – R is the respiratory quotient (typically ~0.8) – 0.21 x (760-47) - (40/0.8) – ~100 mm Hg • Alveolar–arterial (A-a) O2 gradient is normally ~ 10, so PaO2 (arterial PO2) should be ~90 mmHg NB: To convert mm Hg to kPa, multiply by 0.133 Insights from PAO2 Equation (1) • PaO2 ~ PAO2 = (0.21x[Patm-47]) - (PaCO2 / 0.8) – At lower Patm, the PaO2 will be lower • that’s -

Effects of Lethal Levels of Environmental Hypercapnia on Cardiovascular and Blood-Gas Status in Yellowtail, Seriola Quinqueradiata
ZOOLOGICAL SCIENCE 20: 417–422 (2003) 2003 Zoological Society of Japan Effects of Lethal Levels of Environmental Hypercapnia on Cardiovascular and Blood-Gas Status in Yellowtail, Seriola quinqueradiata Kyoung-Seon Lee1, Jun Kita2 and Atsushi Ishimatsu1* 1Marine Research Institute, Nagasaki University, Tairamachi, Nagasaki 851-2213, Japan 2Research Institute of Innovative Technology for the Earth (RITE), Kizucho, Kyoto 619-0209, Japan ABSTRACT—The cardiorespiratory responses were examined in yellowtail, Seriola quinqueradiata exposed to two levels of hypercapnia (seawater equilibrated with a gas mixture containing 1% CO2 (water PCO2 = 7 mmHg) or 5% CO2 (38 mmHg)) for 72 hr at 20°C. Mortality was 100% within 8 hr at 5% CO2, while no fish died at 1% CO2. No cardiovascular variables (cardiac output, Q;˙ heart rate, HR; stroke volume, SV and arterial blood pressure, BP) significantly changed from pre-exposure values during exposure to 1% CO2. Arterial CO2 partial pressure (PaCO2) significantly increased (P < 0.05), reaching a new steady- state level after 3 hr. Arterial blood pH (pHa) decreased initially (P < 0.05), but was subsequently restored – by elevation of plasma bicarbonate ([HCO3 ]). Arterial O2 partial pressure (PaO2), oxygen content (CaO2), and hematocrit (Hct) were maintained throughout the exposure period. In contrast, exposure to 5% CO2 dramatically reduced Q˙ (P < 0.05) through decreasing SV (P < 0.05), although HR did not change. BP was transiently elevated (P < 0.05), followed by a precipitous fall before death. The pHa was restored – incompletely despite a significant increase in [HCO3 ]. PaO2 decreased only shortly before death, whereas CaO2 kept elevated due to a large increase in Hct (P < 0.05). -

Pathophysiology of Acid Base Balance: the Theory Practice Relationship
Intensive and Critical Care Nursing (2008) 24, 28—40 ORIGINAL ARTICLE Pathophysiology of acid base balance: The theory practice relationship Sharon L. Edwards ∗ Buckinghamshire Chilterns University College, Chalfont Campus, Newland Park, Gorelands Lane, Chalfont St. Giles, Buckinghamshire HP8 4AD, United Kingdom Accepted 13 May 2007 KEYWORDS Summary There are many disorders/diseases that lead to changes in acid base Acid base balance; balance. These conditions are not rare or uncommon in clinical practice, but every- Arterial blood gases; day occurrences on the ward or in critical care. Conditions such as asthma, chronic Acidosis; obstructive pulmonary disease (bronchitis or emphasaemia), diabetic ketoacidosis, Alkalosis renal disease or failure, any type of shock (sepsis, anaphylaxsis, neurogenic, cardio- genic, hypovolaemia), stress or anxiety which can lead to hyperventilation, and some drugs (sedatives, opoids) leading to reduced ventilation. In addition, some symptoms of disease can cause vomiting and diarrhoea, which effects acid base balance. It is imperative that critical care nurses are aware of changes that occur in relation to altered physiology, leading to an understanding of the changes in patients’ condition that are observed, and why the administration of some immediate therapies such as oxygen is imperative. © 2007 Elsevier Ltd. All rights reserved. Introduction the essential concepts of acid base physiology is necessary so that quick and correct diagnosis can The implications for practice with regards to be determined and appropriate treatment imple- acid base physiology are separated into respi- mented. ratory acidosis and alkalosis, metabolic acidosis The homeostatic imbalances of acid base are and alkalosis, observed in patients with differing examined as the body attempts to maintain pH bal- aetiologies. -

Severe Metabolic Acidosis in a Patient with an Extreme Hyperglycaemic Hyperosmolar State: How to Manage? Marloes B
Clinical Case Reports and Reviews Case Study ISSN: 2059-0393 Severe metabolic acidosis in a patient with an extreme hyperglycaemic hyperosmolar state: how to manage? Marloes B. Haak, Susanne van Santen and Johannes G. van der Hoeven* Department of Intensive Care Medicine, Radboud University Medical Center, Nijmegen, the Netherlands Abstract Hyperglycaemic hyperosmolar state (HHS) and diabetic ketoacidosis (DKA) are often accompanied by severe metabolic and electrolyte disorders. Analysis and treatment of these disorders can be challenging for clinicians. In this paper, we aimed to discuss the most important steps and pitfalls in analyzing and treating a case with extreme metabolic disarrangements as a consequence of an HHS. Electrolyte disturbances due to fluid shifts and water deficits may result in potentially dangerous hypernatriema and hyperosmolality. In addition, acid-base disorders often co-occur and several approaches have been advocated to assess the acid-base disorder by integration of the principles of mass balance and electroneutrality. Based on the case vignette, four explanatory methods are discussed: the traditional bicarbonate-centered method of Henderson-Hasselbalch, the strong ion model of Stewart, and its modifications ‘Stewart at the bedside’ by Magder and the simplified Fencl-Stewart approach. The four methods were compared and tested for their bedside usefulness. All approaches gave good insight in the metabolic disarrangements of the presented case. However, we found the traditional method of Henderson-Hasselbalch and ‘Stewart at the bedside’ by Magder most explanatory and practical to guide treatment of the electrolyte disturbances and in exploring the acid-base disorder of the presented case. Introduction This is accompanied by changes in pCO2 and bicarbonate (HCO₃ ) levels, depending on the cause of the acid-base disorder. -

CHEM 301 Assignment #3
CHEM 301 Assignment #3 Provide solutions to the following questions in a neat and well organized manner. Clearly state assumptions and reference sources for any constants used. Due date: November 18th 1. Methane and carbon dioxide are produced under anaerobic conditions by the fermentation of organic matter, approximated by the following equation 2 {CH2O} CH4 + CO2 As gas bubbles are evolved at the sediment interface at 5 m depth and remain in contact with water at the sediment surface long enough so that equilibrium is attained. The total pressure at this depth is 148 kPa. If the pH is 8.20, calculate the total carbonate concentration in the interstitial water at 25oC. How would you expect your answer to change if these gas bubbles were present at 500 m depth? Strategy: The total pressure inside the gas bubble must be equal to the total pressure on the outside of the gas bubble (or else it would either explode or collapse). Furthermore, the total pressure inside that gas bubble is equal to the sum of the partial pressures of CH4 and CO2. We can then use the partial pressure of CO2 inside the gas bubble and the corresponding Henry’s law constant to calculate the concentration of aqueous CO2 at equilibrium. Given the pH of the solution and the expressions for Ka1 and Ka2, we can determine the concentration of HCO3- and 2- CO3 . (see textbook pgs 241-242; Chap 11, Q9) Solution: The total carbonate concentration is given by; 2- - 2- [CO3 ]T = [CO2(aq)] + [HCO3 ] + [CO3 ] From the pH speciation diagram (Fig. -

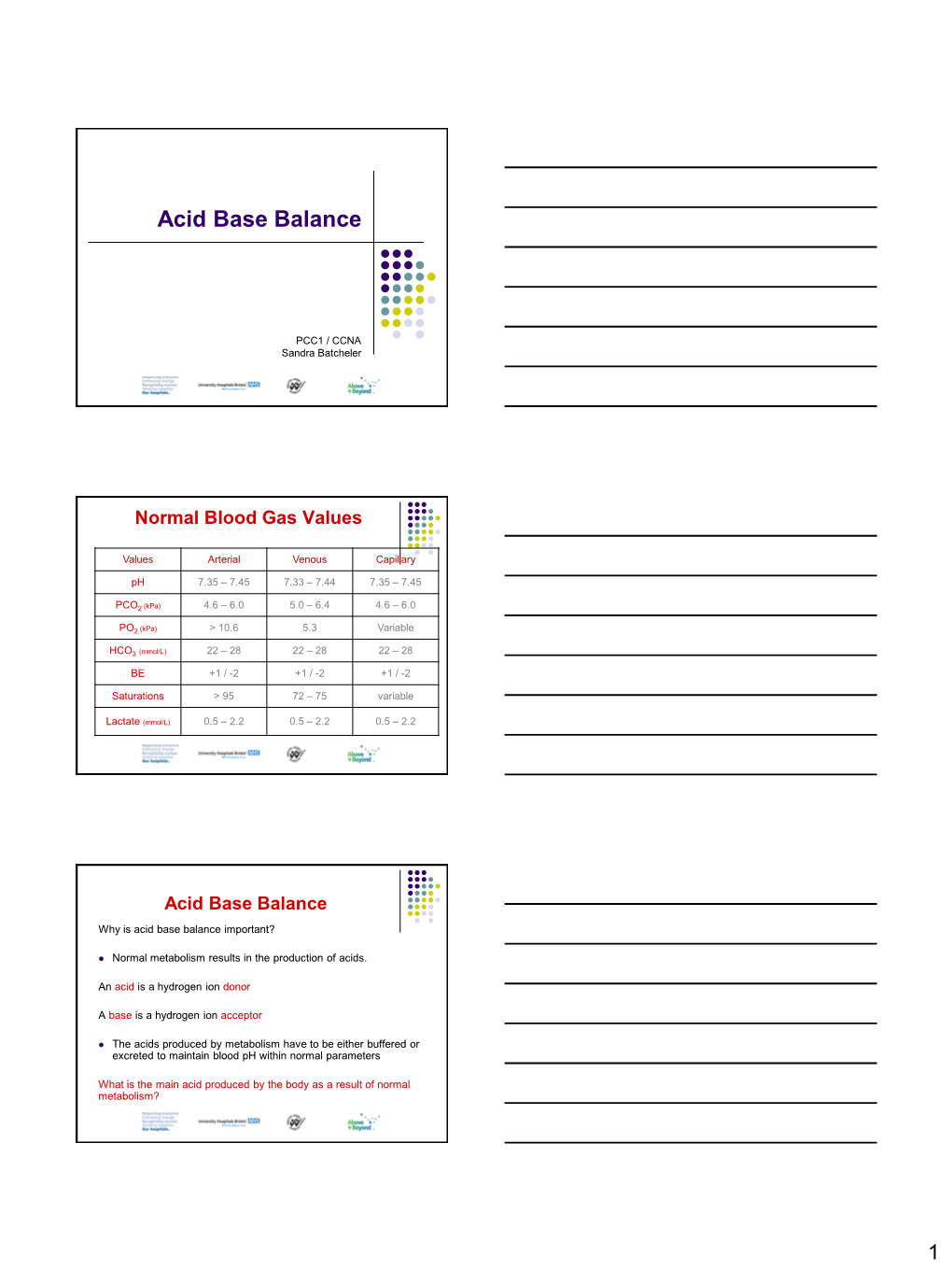
Arterial Blood Gases: Acid-Base Balance
EDUCATIONAL COMMENTARY – ARTERIAL BLOOD GASES: ACID-BASE BALANCE Educational commentary is provided through our affiliation with the American Society for Clinical Pathology (ASCP). To obtain FREE CME/CMLE credits click on Earn CE Credits under Continuing Education on the left side of the screen. **Florida licensees, please note: This exercise will appear in CE Broker under the specialty of Blood Gas Analysis. LEARNING OUTCOMES On completion of this exercise, the participant should be able to • identify the important buffering systems in the human body. • explain the Henderson-Hasselbalch equation and its relationship to the bicarbonate/carbonic acid buffer system. • explain the different acid-base disorders, causes associated with them, and compensatory measures. • evaluate acid-base status using patient pH and pCO2 and bicarbonate levels. Introduction Arterial blood gas values are an important tool for assessing oxygenation and ventilation, evaluating acid- base status, and monitoring the effectiveness of therapy. The human body produces a daily net excess of acid through normal metabolic processes: cellular metabolism produces carbonic, sulfuric, and phosphoric acids. Under normal conditions, the body buffers accumulated hydrogen ions (H+) through a variety of buffering systems, the respiratory center, and kidneys to maintain a plasma pH of between 7.35 and 7.45. This tight maintenance of blood pH is essential: even slight changes in pH can alter the functioning of enzymes, the cellular uptake and use of metabolites, and the uptake and release of oxygen. Although diagnoses are made by physicians, laboratory professionals must be able to interpret arterial blood gas values to judge the validity of the laboratory results they report. -

Relationship Between PCO 2 and Unfavorable Outcome in Infants With
nature publishing group Articles Clinical Investigation Relationship between PCO2 and unfavorable outcome in infants with moderate-to-severe hypoxic ischemic encephalopathy Krithika Lingappan1, Jeffrey R. Kaiser2, Chandra Srinivasan3, Alistair J. Gunn4; on behalf of the CoolCap Study Group BACKGROUND: Abnormal PCO2 is common in infants with term infants with HIE, both minimum and cumulative expo- hypoxic ischemic encephalopathy (HIE). The objective was to sure to hypocapnia in the first 12 h of the trial were associated determine whether hypocapnia was independently associated with death or adverse neurodevelopmental outcome (13). The with unfavorable outcome (death or severe neurodevelopmen- dose–response relationship between PCO2 and outcome for tal disability at 18 mo) in infants with moderate-to-severe HIE. infants with moderate-to-severe HIE is unknown. METHODS: This was a post hoc analysis of the CoolCap Study The risk of developing hypocapnia or hypercapnia may be in which infants were randomized to head cooling or standard affected by severity of brain injury, intensity and duration of care. Blood gases were measured at prespecified times after newborn resuscitation, timing after the primary injury, and/or randomization. PCO2 and follow-up data were available for 196 response to metabolic acidosis. Thus, in this secondary analy- of 234 infants. Analyses were performed to investigate the rela- sis of the CoolCap Study (14), we sought to confirm the obser- tionship between hypocapnia in the first 72 h after randomiza- vation that -

Arterial Blood Gases During Treatment of Congestive Heart Failure
University of Nebraska Medical Center DigitalCommons@UNMC MD Theses Special Collections 5-1-1969 Arterial blood gases during treatment of congestive heart failure John B. Byrd University of Nebraska Medical Center This manuscript is historical in nature and may not reflect current medical research and practice. Search PubMed for current research. Follow this and additional works at: https://digitalcommons.unmc.edu/mdtheses Part of the Medical Education Commons Recommended Citation Byrd, John B., "Arterial blood gases during treatment of congestive heart failure" (1969). MD Theses. 77. https://digitalcommons.unmc.edu/mdtheses/77 This Thesis is brought to you for free and open access by the Special Collections at DigitalCommons@UNMC. It has been accepted for inclusion in MD Theses by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. ARTERIAL BLOOD GASES DURING TREATMENT OF CONGESTIVE HEART FAILURE By John B~ Byrd A THESIS Presented to the Faculty of The CollsQs of Medicine in the Universi,!;v of Ne.braska In Partial Fulfillment of Requirements For the Degree of Doctor of Medicine Under the Supervision of John R. Jones, MO Omaha, Nebraska February 3, 1969 CONTENTS Introduction 1 Methods 4 Results 6 Discussion 7 Summary 9 References 10 ARTERIAL BLOOD GASES DURING TREATMENT OF CONGESTIVE HEART FAILURE The congestive syndromes of heart failure are classified as 1) acute pulmonary edema (acute left ventricular failure) and 2) chronic heart failure in Principles of Internal Medicine e d ~'t e d'oy H'arr~son, ea.tIll Acute left ventricular failure is characterized oy paroxysmal dyppnea. It may be caused by an elevated filling load (most common), acute myocardial infarction, ectopic tachycardia or fulminant myocarditis--th8 first causing a high-output syndrome with cardiogenic shock occurring late; the remaining causes characterized by an abrupt declir~in cardiac output. -

The Basics of Ventilator Management Overview How We Breath
3/23/2019 The Basics of Ventilator Management What are we really trying to do here Peter Lutz, MD Pulmonary and Critical Care Medicine Pulmonary Associates, Mobile, Al Overview • Approach to the physiology of the lung and physiological goals of mechanical Ventilation • Different Modes of Mechanical Ventilation and when they are indicated • Ventilator complications • Ventilator Weaning • Some basic trouble shooting How we breath http://people.eku.edu/ritchisong/301notes6.htm 1 3/23/2019 How a Mechanical Ventilator works • The First Ventilator- the Iron Lung – Worked by creating negative atmospheric pressure around the lung, simulating the negative pressure of inspiration How a Mechanical Ventilator works • The Modern Ventilator – The invention of the demand oxygen valve for WWII pilots if the basis for the modern ventilator https://encrypted-tbn0.gstatic.com/images?q=tbn:ANd9GcRI5v-veZULMbt92bfDmUUW32SrC6ywX1vSzY1xr40aHMdsCVyg6g How a Mechanical Ventilator works • The Modern Ventilator – How it works Inspiratory Limb Flow Sensor Ventilator Pressure Sensor Expiratory Limb 2 3/23/2019 So what are the goals of Mechanical Ventilation • What are we trying to control – Oxygenation • Amount of oxygen we are getting into the blood – Ventilation • The movement of air into and out of the lungs, mainly effects the pH and level of CO 2 in the blood stream Lab Oxygenation Ventilation Pulse Ox Saturation >88-90% Arterial Blood Gas(ABG) Po 2(75-100 mmHg) pCO 2(40mmHg) pH(~7.4) Oxygenation How do we effect Oxygenation • Fraction of Inspired Oxygen (FIO 2) – Percentage of the gas mixture given to the patient that is Oxygen • Room air is 21% • On the vent ranges from 30-100% • So if the patient’s blood oxygen levels are low, we can just increase the amount of oxygen we give them 3 3/23/2019 How do we effect Oxygenation • Positive End Expiratory Pressure (PEEP) – positive pressure that will remains in the airways at the end of the respiratory cycle (end of exhalation) that is greater than the atmospheric pressure in mechanically ventilated patients. -

Unit 4 Acid-Base Homeostasis
Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum UNIT 4 ACID-BASE HOMEOSTASIS UNIT OBJECTIVES: 1. Demonstrate an understanding of the biochemistry and physiology of acid-base homeostasis. 2. Demonstrate the ability to diagnose and effectively treat complex disorders of acid-base balance. COMPETENCY-BASED KNOWLEDGE OBJECTIVES: 1. Explain hydrogen ion biochemistry and physiology to include: a. The Henderson-Hasselbalch equation (1) Ventilatory component (pCO2) (2) Renal component (HCO3-) 2. Classify metabolic acidosis, including "anion gap" and hyperchloremic acidosis. 3. Identify specific causes of metabolic acidosis. 4. Given values for pH, pCO2, and HCO3-, distinguish between metabolic acidosis, respiratory acidosis, metabolic alkalosis, respiratory alkalosis, and mixed abnormalities; derive a differential diagnosis for each. 5. Predict the importance of primary diseases and their complications to the evaluation of patient risk for: a. Shock b. Bowel obstruction c. Sepsis 6. Analyze the acid-base problem and its cause in specific clinical situations, and determine an appropriate course of therapy for the following conditions: a. "Medical" problems such as: (1) Diabetic ketoacidosis (2) Lactic acidosis (3) Renal tubular acidosis (4) Renal insufficiency (5) Respiratory failure b. "Surgical" problems such as: (1) Gastric outlet obstruction (2) Fistulas (3) Shock COMPETENCY-BASED PERFORMANCE OBJECTIVES: 1. Diagnose and treat acid-base disturbances of all types. 2. Diagnose and treat complex and combined problems in acid-base disturbances as a component of overall care. 3. Manage complex situations in the intensive care unit where acid-base Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum abnormalities coexist with other metabolic derangements, including: a.