Lab Dept: Chemistry Test Name: VENOUS BLOOD GAS (VBG)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Versus Laboratory for Estimating of Dehydration Severity
Clinical versus laboratory for estimating of dehydration severity Majid Malaki Pediatric Health Research Center, Tabriz Medical University, Tabriz, Iran ABSTRACT Background: Acute gastroenteritis is a common cause of dehydration and precise estimation of dehydration Materials and Methods: D is a vital matter for clinical decisions. We try to find how much clinically diagnosed scales are compatible with ORIGINAL ARTICLE laboratory tests measures. uring 2 years 95 infants and children aged between 2 and 108 months entered to emergency room with acute gastroenteritis. They were categorized as mild, moderate and severe dehydration, their recorded laboratory tests include blood urea nitrogen (BUN), creatinine, venous blood gases values were expressedP by means ±95% of confidence intervalResult and compared by mann-whitney test in each groups with SPSS 16, sensitivity, specificity and likelihood ratio measured for defined cut off values in severe dehydration group, value less than 0.05 was significant. : Severe dehydration includes 3% Conclusionof all hospitalization: R due to dehydration. Laboratory tests cannot differentiate mild to moderate dehydration definietly but this difference is significant between severe to mild and severe to moderate dehydration. outine laboratory test are not generally helpful for dehydration severity estimation but they can be discriminate severe from mild or moderate dehydration exclusively. Creatinine higher than 0.9 mg/dl and BaseKey words deficit: beyond-16A are specific (90%) for severe dehydration estimation -

Evaluation of Abnormal Liver Chemistries
ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries Paul Y. Kwo, MD, FACG, FAASLD1, Stanley M. Cohen, MD, FACG, FAASLD2, and Joseph K. Lim, MD, FACG, FAASLD3 1Division of Gastroenterology/Hepatology, Department of Medicine, Stanford University School of Medicine, Palo Alto, California, USA; 2Digestive Health Institute, University Hospitals Cleveland Medical Center and Division of Gastroenterology and Liver Disease, Department of Medicine, Case Western Reserve University School of Medicine, Cleveland, Ohio, USA; 3Yale Viral Hepatitis Program, Yale University School of Medicine, New Haven, Connecticut, USA. Am J Gastroenterol 2017; 112:18–35; doi:10.1038/ajg.2016.517; published online 20 December 2016 Abstract Clinicians are required to assess abnormal liver chemistries on a daily basis. The most common liver chemistries ordered are serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase and bilirubin. These tests should be termed liver chemistries or liver tests. Hepatocellular injury is defined as disproportionate elevation of AST and ALT levels compared with alkaline phosphatase levels. Cholestatic injury is defined as disproportionate elevation of alkaline phosphatase level as compared with AST and ALT levels. The majority of bilirubin circulates as unconjugated bilirubin and an elevated conjugated bilirubin implies hepatocellular disease or cholestasis. Multiple studies have demonstrated that the presence of an elevated ALT has been associated with increased liver-related mortality. A true healthy normal ALT level ranges from 29 to 33 IU/l for males, 19 to 25 IU/l for females and levels above this should be assessed. The degree of elevation of ALT and or AST in the clinical setting helps guide the evaluation. -

Total Bilirubin in Athletes, Determination of Reference Range
OriginalTotal bilirubin Paper in athletes DOI: 10.5114/biolsport.2017.63732 Biol. Sport 2017;34:45-48 Total bilirubin in athletes, determination of reference range AUTHORS: Witek K1, Ścisłowska J2, Turowski D1, Lerczak K1, Lewandowska-Pachecka S2, Corresponding author: Pokrywka A3 Konrad Witek Department of Biochemistry, Institute of Sport - National 1 Department of Biochemistry, Institute of Sport - National Research Institute, Warsaw, Poland Research Institute 2 01-982 Warsaw, Poland Faculty of Pharmacy with the Laboratory Medicine Division, Medical University of Warsaw, Poland 3 E-mail: Department of Biochemistry, 2nd Faculty of Medicine, Medical University of Warsaw, Poland [email protected] ABSTRACT: The purpose of this study was to determine a typical reference range for the population of athletes. Results of blood tests of 339 athletes (82 women and 257 men, aged 18-37 years) were retrospectively analysed. The subjects were representatives of different sports disciplines. The measurements of total bilirubin (BIT), iron (Fe), alkaline phosphatase (ALP), alanine aminotransferase (ALT) and gamma-glutamyltransferase (GGT) were made using a Pentra 400 biochemical analyser (Horiba, France). Red blood cell count (RBC), reticulocyte count and haemoglobin concentration measurements were made using an Advia 120 haematology analyser (Siemens, Germany). In groups of women and men the percentage of elevated results were similar at 18%. Most results of total bilirubin in both sexes were in the range 7-14 μmol ∙ L-1 (49% of women and 42% of men). The highest results of elevated levels of BIT were in the range 21-28 μmol ∙ L-1 (12% of women and 11% of men). There was a significant correlation between serum iron and BIT concentration in female and male athletes whose serum total bilirubin concentration does not exceed the upper limit of the reference range. -
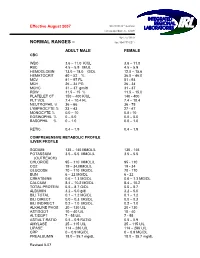
Normal Rangesа–А
Effective August 2007 5361 NW 33 rd Avenue Fort Lauderdale, FL 33309 954-777-0018 NORMAL RANGES – fax: 954-777-0211 ADULT MALE FEMALE CBC WBC 3.6 – 11.0 K/UL 3.6 – 11.0 RBC 4.5 – 5.9 M/UL 4.5 – 5.9 HEMOGLOBIN 13.0 – 18.0 G/DL 12.0 – 15.6 HEMATOCRIT 40 – 52 % 36.0 – 46.0 MCV 81 – 97 FL 81 93 MCH 26 – 34 PG 26 34 MCHC 31 – 37 gm/dl 31 37 RDW 11.5 – 15 % 11.5 – 15.0 PLATELET CT 150 – 400 K/UL 140 400 PLT VOL 7.4 – 10.4 FL 7.4 – 10.4 NEUTROPHIL % 36 – 66 36 75 LYMPHOCYTE % 23 – 43 27 47 MONOCYTE % 0.0 – 10 0.0 10 EOSINOPHIL % 0 – 5.0 0.0 – 5.0 BASOPHIL % 0 – 1.0 0.0 – 1.0 RETIC 0.4 – 1.9 0.4 – 1.9 COMPREHENSIVE METABOLIC PROFILE /LIVER PROFILE SODIUM 135 – 145 MMOL/L 135 145 POTASSIUM 3.5 – 5.5 MMOL/L 3.5 – 5.5 (OUTREACH) CHLORIDE 95 – 110 MMOL/L 95 110 CO2 19 – 34.MMOL/L 19 34 GLUCOSE 70 – 110 MG/DL 70 110 BUN 6 – 22 MG/DL 6 22 CREATININE 0.6 – 1.3 MG/DL 0.6 – 1.3 MG/DL CALCIUM 8.4 – 10.2 MG/DL 8.4 – 10.2 TOTAL PROTEIN 5.5 – 8.7 G/DL 5.5 – 8.7 ALBUMIN 3.2 – 5.0 g/dl 3.2 – 5.0 BILI TOTAL 0.1 – 1.2 MG/DL 0.1 – 1.2 BILI DIRECT 0.0 – 0.3 MG/DL 0.0 – 0.3 BILI INDIRECT 0.2 – 1.0 MG/DL 0.2 – 1.0 ALKALINE PHOS 20 – 130 U/L 20 130 AST/SGOT 10 – 40 U/L 10 40 ALT/SGPT 7 55 U/L 7 55 AST/ALT RATIO 0.5 – 0.9 RATIO 0.5 – 0.9 AMYLASE 25 – 115 U/L 25 – 115 U/L LIPASE 114 – 286 U/L 114 – 286 U/L CRP 0 – 0.9 MG/DL 0 – 0.9 MG/DL PREALBUMIN 18.0 – 35.7 mg/dL 18.0 – 35.7 mg/dL Revised 807 MAGNESIUM 1.8 – 2.4 mg/dL 1.8 – 2.4 mg/Dl LDH 100 – 200 Units /L 100 – 200 Units/L PHOSPHOROUS 2.3 – 5.0 mg/dL 2.3 – 5.0 mg/dL LACTIC ACID 0.4 -

Laboratory Test Reference Ranges
Laboratory Test Reference Ranges Central Zone Always refer to the laboratory report for appropriate reference ranges at the time of analysis. This document lists the test reference ranges that were established for the analysis methodologies used only by Nova Scotia Health Central Zone (Central Zone) Department of Pathology and Laboratory Medicine facilities. Anatomical Pathology Blood Tests Name of Test Specimen Units Low High Critical Type Anti-Cardiac Muscle Antibody Serum (SST) Qualitative N/A N/A N/A Anti-Skeletal Muscle Antibody Serum (SST) Qualitative N/A N/A N/A Anti-Pemphigoid Antibody Serum (SST) Qualitative N/A N/A N/A Anti-Pancreatic Islet Cell Antibody Serum (SST) Qualitative N/A N/A N/A Anti-Smooth Muscle Antibody Serum (SST) Qualitative N/A N/A N/A Anti-Liver Kidney Microsomal Antibody Serum (SST) Qualitative N/A N/A N/A Clinical Chemistry Blood Tests Name of Test Gender Age Units Low High Critical Acetaminophen M/F >0min µmol/L >350 Interpretive Data: Therapeutic range: 66-199 umol/L Toxic level: Refer to Rumack Matthew nomogram. Acetaminophen results can be falsely low for patients undergoing treatment of N- acetylcysteine (NAC). Adrenocorticotropic M/F >0min pmol/L 2.3 10.1 hormone Interpretive Data: Adrenocorticotropic Hormone (ACTH) reference ranges are based on (ACTH) samples collected prior to 10 AM. Albumin M/F 0-1yr g/L 25 46 >1yr 35 50 Alcohol M/F >0min mmol/L None Detected >54 Interpretive Data: The method is intended for clinical purposes only. Medical-legal specimens should be analyzed by gas chromatographic method for confirmation of results. -

Severe Metabolic Acidosis in a Patient with an Extreme Hyperglycaemic Hyperosmolar State: How to Manage? Marloes B
Clinical Case Reports and Reviews Case Study ISSN: 2059-0393 Severe metabolic acidosis in a patient with an extreme hyperglycaemic hyperosmolar state: how to manage? Marloes B. Haak, Susanne van Santen and Johannes G. van der Hoeven* Department of Intensive Care Medicine, Radboud University Medical Center, Nijmegen, the Netherlands Abstract Hyperglycaemic hyperosmolar state (HHS) and diabetic ketoacidosis (DKA) are often accompanied by severe metabolic and electrolyte disorders. Analysis and treatment of these disorders can be challenging for clinicians. In this paper, we aimed to discuss the most important steps and pitfalls in analyzing and treating a case with extreme metabolic disarrangements as a consequence of an HHS. Electrolyte disturbances due to fluid shifts and water deficits may result in potentially dangerous hypernatriema and hyperosmolality. In addition, acid-base disorders often co-occur and several approaches have been advocated to assess the acid-base disorder by integration of the principles of mass balance and electroneutrality. Based on the case vignette, four explanatory methods are discussed: the traditional bicarbonate-centered method of Henderson-Hasselbalch, the strong ion model of Stewart, and its modifications ‘Stewart at the bedside’ by Magder and the simplified Fencl-Stewart approach. The four methods were compared and tested for their bedside usefulness. All approaches gave good insight in the metabolic disarrangements of the presented case. However, we found the traditional method of Henderson-Hasselbalch and ‘Stewart at the bedside’ by Magder most explanatory and practical to guide treatment of the electrolyte disturbances and in exploring the acid-base disorder of the presented case. Introduction This is accompanied by changes in pCO2 and bicarbonate (HCO₃ ) levels, depending on the cause of the acid-base disorder. -

Determination of Reference Ranges for Selected Clinical Laboratory Tests for a Medical Laboratory in Namibia Using Pre-Tested Data
DETERMINATION OF REFERENCE RANGES FOR SELECTED CLINICAL LABORATORY TESTS FOR A MEDICAL LABORATORY IN NAMIBIA USING PRE-TESTED DATA by CORNELIA DE WAAL-MILLER Student no: 197084516 Thesis submitted in fulfillment of the requirements of the degree Master of Technology: Biomedical Technology in the Faculty of Health and Wellness Sciences at the Cape Peninsula University of Technology Supervisor: Professor A.J. Esterhuyse Co-Supervisor: Professor B. Noden Bellville March 2015 CPUT copyright information The thesis may not be published either in part (in scholarly, scientific or technical journals), or as a whole (as a monograph), unless permission has been obtained from the University. (i) Declaration I, Cornelia de Waal-Miller, declare that the content of this thesis represents my own unaided work, and that this thesis has not previously been submitted for academic examination towards any qualification. Furthermore, this thesis represents my own opinions and not necessarily those of the Cape Peninsula University of Technology. 12th March 2015 Signed Date 2 | of 84 Pages (ii) Abstract Aim: The aim of the study was to compile pre-tested laboratory results stored in the laboratory database of the Namibia Institute of Pathology (NIP). The study also aimed to assess the usefulness and validity of using retrospective laboratory results of different patients in varying degrees of health and which were produced using various methods in different laboratories in Namibia. Methods: 254,271 test results (female: 134,261, male = 117,091, unknown gender= 2,919) consisting of Haemoglobin, serum Urea, serum Creatinine, plasma Glucose (fasting and random), serum Cholesterol, serum Triglycerides and serum Uric Acid was extracted from NIP Laboratory Information System over a period of four years and of the 13 different regions of Namibia were analyzed. -

Study on Acid-Base Balance Disorders and the Relationship
ArchiveNephro-Urol of Mon SID. 2020 May; 12(2):e103567. doi: 10.5812/numonthly.103567. Published online 2020 May 23. Research Article Study on Acid-Base Balance Disorders and the Relationship Between Its Parameters and Creatinine Clearance in Patients with Chronic Renal Failure Tran Pham Van 1, *, Thang Le Viet 2, Minh Hoang Thi 1, Lan Dam Thi Phuong 1, Hang Ho Thi 1, Binh Pham Thai 3, Giang Nguyen Thi Quynh 3, Diep Nong Van 4, Sang Vuong Dai 5 and Hop Vu Minh 1 1Biochemistry Department, Military Hospital 103, Hanoi, Vietnam 2Nephrology and Hemodialysis Department, Military Hospital 103, Hanoi, Vietnam 3National Hospital of Endocrinology, Hanoi, Vietnam 4Biochemistry Department, Backan Hospital, Vietnam 5Biochemistry Department, Thanh Nhan Hospital, Hanoi, Vietnam *Corresponding author: Biochemistry Department, Military Hospital 103, Hanoi, Vietnam. Email: [email protected] Received 2020 May 09; Accepted 2020 May 09. Abstract Objectives: We aimed to determine the parameters of acid-base balance in patients with chronic renal failure (CRF) and the rela- tionship between the parameters evaluating acid-base balance and creatinine clearance. Methods: The current cross-sectional study was conducted on 300 patients with CRF (180 males and 120 females). Clinical examina- tion and blood tests by taking an arterial blood sample for blood gas measurement as well as venous blood for biochemical tests to select study participants were performed. Results: Patients with CRF in the metabolic acidosis group accounted for 74%, other types of disorders were less common. The average pH, PCO2, HCO3, tCO2 and BE of the patient group were 7.35 ± 0.09, 34.28 ± 6.92 mmHg, 20.18 ± 6.06 mmol/L, 21.47 ± 6.48 mmHg and -4.72 ± 6.61 mmol/L respectively. -

A Practical Approach to Acid-Base Balance for Small Animal Practitioners
A PRACTICAL APPROACH TO ACID-BASE BALANCE FOR SMALL ANIMAL PRACTITIONERS IVMA CE Self-Study Offering Dr Nicola Parry, DipACVP Midwest Veterinary Pathology, LLC Lafayette, IN AIM OF THIS ARTICLE Acid-base balance (ABB) is a convoluted concept that requires detailed comprehension of the metabolic pathways used to eliminate the H+ ion from the body. Not surprisingly, many practitioners find it daunting to retain the key concepts and apply them in a meaningful way clinical practice. This article aims to review some of the major points about ABB, and to provide a stepwise approach to evaluating laboratory data in order to identify key aspects of acid-base disorders. Although the chemical/biochemical basis of ABB is important, this article aims to share a practical and more factual, informal approach to the subject that will hopefully appeal to the majority of practitioners. Readers who crave extensive derivations of the Henderson-Hasselbalch equation are welcome to revisit their dusty textbooks for increased levels of excitement! LEARNING OBJECTIVES Following completion of this continuing education article, you will be able to: Indicate whether the pH level indicates acidosis or alkalosis List major sources of acids in the body Identify the major chemical buffer systems in the body Identify the cause of the pH imbalance as either respiratory or metabolic Distinguish between acidosis and alkalosis resulting from respiratory and metabolic factors Describe the importance of respiratory and renal compensations to ABB Determine if there is any compensation for the acid-base imbalance Identify the causes of high anion gap metabolic acidosis Use a systematic, step-by-step approach to diagnose acid-base disorders from laboratory data SO WHAT IS ABB & WHY DO WE CARE ABOUT IT? ABB is fundamental to physiologic homeostasis and refers to the way in which the body maintains a relatively constant pH despite continuous production of metabolic end products. -

BLOOD GAS ANALYSIS Deorari , AIIMS 2008
Deorari , AIIMS 2008 BLOOD GAS ANALYSIS Deorari , AIIMS 2008 Contents 1. Introduction, indications and sources of errors 2. Terminology and normal arterial blood gases 3. Understanding the print outs 4. Details about (i) pH (ii) Oxygenation, oxygen saturation, oxygen content, alveolar gas equation, indices of oxygenation (iii) Carbon dioxide transport, Pco2 total CO2 content, and bicarbonate levels (iv) Base excess and buffer base 5. Simple and mixed disorders 6. Compensation mechanisms 7. Anion Gap 8. Approach to arterial blood gases and exercises 9. Arterial blood gases decision tree 10. Practical tips for sampling for ABG. 2 Deorari , AIIMS 2008 Abbreviations ABE Actual base excess ABG Arterial blood gas AaDO2 Alveolar to arterial oxygen gradient Baro/PB Barometric pressure BB Buffer base BE Base excess BEecf Base excess in extracellular fluid BPD Bronchopulmonary dysplasia CH+ Concentration of hydrogen ion CO2 Carbon dioxide ECMO Extra corporeal membrane oxygenation FiO2 Fraction of inspired oxygen HCO3 Bicarbonate H2CO3 Carbonic acid MAP Mean airway pressure O2CT Oxygen content of blood PaCO2 Partial pressure of carbon dioxide in arterial blood PaO2 Partial pressure of oxygen in arterial blood pAO2 Partial pressure of oxygen in alveoli pH2O Water vapour pressure PPHN Persistent pulmonary hypertension in newborn RBC Red blood corpuscles 3 Deorari , AIIMS 2008 RQ Respiratory quotient Sat Saturation SBE Standard base excess - St HCO 3/SBC Standard bicarbonate TCO2 Total carbon dioxide content of blood THbA Total haemoglobin concentration UAC Umbilical artery catheter 4 Deorari , AIIMS 2008 The terminology of arterial blood gas (ABG) is complex and confusing. It is made worse by the printouts generated by recent microprocessors. -

Calcium, Plasma, Total
Division of Laboratory Medicine Biochemistry Calcium, plasma, total Calcium is the most abundant mineral element in the body with about 99 percent in the bones primarily as hydroxyapatite. The remaining calcium is distributed between the various tissues and the extracellular fluids where it performs a vital role for many life sustaining processes. Among the extra skeletal functions of calcium are involvement in blood coagulation, neuromuscular conduction, excitability of skeletal and cardiac muscle, enzyme activation, and the preservation of cell membrane integrity and permeability. Calcium levels and hence the body content are controlled by parathyroid hormone (PTH), calcitonin, and vitamin D. To maintain calcium homeostasis, we require sufficient intake, normal metabolism and appropriate excretion. An imbalance in any of these modulators leads to alterations of the body and circulating calcium levels. Increases in serum PTH or vitamin D are usually associated with hypercalcemia. Increased calcium levels may also be observed in multiple myeloma and other neoplastic diseases. Hypocalcemia may be observed e.g. in hypoparathyroidism, nephrosis, and pancreatitis. Total Calcium is reported as direct and after adjustment for plasma albumin level. Adjusted total calcium has the same reference interval as total calcium and is a surrogate for ionised calcium. General information Collection container: Adults – serum (with gel separator, 4.9mL brown top Sarstedt tube) Paediatrics – lithium heparin plasma (1.2mL orange top Sarstedt tube) Type and volume of sample: The tubes should be thoroughly mixed before transport to the lab. 1mL whole blood is required as a minimum volume. Specimen transport/special precautions: N/A Laboratory information Method principle: Calcium ions react with 5‑nitro‑5’‑methyl‑BAPTA (NM‑BAPTA) under alkaline conditions to form a complex. -

Postconditioning in Major Vascular Surgery: Prevention of Renal Failure
Aranyi et al. Journal of Translational Medicine (2015) 13:21 DOI 10.1186/s12967-014-0379-7 RESEARCH Open Access Postconditioning in major vascular surgery: prevention of renal failure Peter Aranyi1, Zsolt Turoczi1, David Garbaisz1, Gabor Lotz2, Janos Geleji3, Viktor Hegedus1, Zoltan Rakonczay4, Zsolt Balla4, Laszlo Harsanyi1 and Attila Szijarto1* Abstract Background: Postconditioning is a novel reperfusion technique to reduce ischemia-reperfusion injuries. The aim of the study was to investigate this method in an animal model of lower limb revascularization for purpose of preventing postoperative renal failure. Methods: Bilateral lower limb ischemia was induced in male Wistar rats for 3 hours by infrarenal aorta clamping under narcosis. Revascularization was allowed by declamping the aorta. Postconditioning (additional 10 sec reocclusion, 10 sec reperfusion in 6 cycles) was induced at the onset of revascularization. Myocyte injury and renal function changes were assessed 4, 24 and 72 hours postoperatively. Hemodynamic monitoring was performed by invasive arterial blood pressure registering and a kidney surface laser Doppler flowmeter. Results: Muscle viability studies showed no significant improvement with the use of postconditioning in terms of ischemic rhabdomyolysis (4 h: ischemia-reperfusion (IR) group: 42.93 ± 19.20% vs. postconditioned (PostC) group: 43.27 ± 27.13%). At the same time, renal functional laboratory tests and kidney myoglobin immunohistochemistry demonstrated significantly less expressed kidney injury in postconditioned animals (renal failure index: 4 h: IR: 2.37 ± 1.43 mM vs. PostC: 0.92 ± 0.32 mM; 24 h: IR: 1.53 ± 0.45 mM vs. PostC: 0.77 ± 0.34 mM; 72 h: IR: 1.51 ± 0.36 mM vs.