Diarrhea After Hours Telephone Triage Protocols | Adult | 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Case Report Acute Abdomen Caused by Brucellar Hepatic Abscess
Case Report Acute Abdomen Caused by Brucellar Hepatic Abscess Cem Ibis, Atakan Sezer, Ali K. Batman, Serkan Baydar, Alper Eker,1 Ercument Unlu,2 Figen Kuloglu,1 Bilge Cakir2 and Irfan Coskun, Departments of General Surgery, 1Infectious Diseases and 2Radiology, Faculty of Medicine, Trakya University, Edirne, Turkey. Brucellosis is a zoonotic infection that is transmitted from animals to humans by ingestion of infected food products, direct contact with an infected animal, or aerosol inhalation. The disease is endemic in many coun- tries, including the Mediterranean basin, the Middle East, India, Mexico, Central and South America and, central and southwest Asia. Human brucellosis is a systemic infection with a wide clinical spectrum. Although hepatic involvement is very common during the course of chronic brucellosis, hepatic abscess is a very rare complication of Brucella infection. We present a case of hepatic abscess caused by Brucella, which resembled the clinical presentation of surgical acute abdomen. [Asian J Surg 2007;30(4):283–5] Key Words: acute abdomen, Brucella, brucelloma, hepatic abscess, percutaneous drainage Introduction and high fever. His symptoms began 2 days before admis- sion. For the previous 2 weeks, he suffered from a slight Brucellosis is a zoonotic infection transmitted from ani- evening fever and associated sweating. Physical examina- mals to humans by ingestion of infected food products, tion revealed moderate splenomegaly, tenderness, abdom- direct contact with an infected animal, or inhalation of inal guarding, and rebound tenderness in the right upper aerosols.1 The disease remains endemic in many coun- quadrant. The symptoms of peritoneal irritation in the tries, mainly in the Mediterranean basin, the Middle East, right upper quadrant of the abdomen clinically suggested a India, Mexico, Central and South America and, currently, surgical acute abdomen. -

2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome
MEDICAL POLICY – 2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome BCBSA Ref. Policy: 2.04.26 Effective Date: July 1, 2021 RELATED MEDICAL POLICIES: Last Revised: June 8, 2021 None Replaces: N/A Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction Intestinal dysbiosis is a condition that occurs when the microorganisms in the digestive tract are out of balance. This condition is believed to cause diseases of the digestive tract, including poor nutrient absorption, overgrowth of certain bacteria, and irritable bowel syndrome (IBS). Symptoms of these digestive problems are similar and may include: abdominal pain, excess gas, bloating, and changes in bowel movements (constipation or diarrhea, or both). One method of diagnosing digestive disorders is by testing a fecal sample. Using fecal analysis to diagnose intestinal dysbiosis, IBS, malabsorption, or small intestinal overgrowth of bacteria is unproven (investigational). More studies are needed to see if this testing improves health outcomes. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. The rest of the policy uses specific words and concepts familiar to medical professionals. It is intended for providers. A provider can be a person, such as a doctor, nurse, psychologist, or dentist. A provider also can be a place where medical care is given, like a hospital, clinic, or lab. This policy informs them about when a service may be covered. -

Management of Travellers' Diarrhoea in Adults In
MANAGEMENT OF TRAVELLERS’ DIARRHOEA IN ADULTS IN PRIMARY CARE Homerton University Hospital and Hospital for Tropical Diseases December 2016 (review date December 2017) Presence of Assess as per NICE • Diarrhoea +/- nausea / vomiting and >3 loose stools per day guidelines on acute • PLUS travel outside of Western Europe / N America / Australia / diarrhoea New Zealand NO https://cks.nice.org • OR diarrhoea in men who have sex with other men (MSM) even in .uk/diarrhoea- the absence of foreign travel adults-assessment YES Refer to Homerton Infectious Diseases (ID) clinic (box Duration > 2 weeks 3) & commence stool investigations (MC&S, OCP +/- YES C difficle toxin test) NO Features of severe illness: • Fever >38.5 +/- bloody diarrhoea +/- severe abdominal pain OR • Immunocompromised (chemotherapy/ after tissue transplant/HIV with a low CD4 count) • Underlying intestinal pathology (inflammatory bowel disease/ ileostomy/short bowel syndrome) • Conditions where reduced oral intake may be dangerous (diabetes, sickle cell disease, elderly) YES Refer to YES • Dehydrated? Homerton • Evidence of sepsis? A&E (box 3) • Fever plus travel to malaria-endemic area NO • Acute abdomen/ signs suggestive of appendicitis? • Unable to manage at home/ clinician concern NO Diarrhoea with risk factors for severe illness/ Non-severe illness complications Investigations Investigations • Stool MC&S • Stool MC&S • Stool OC&P x 2 • Stool OC&P x 2 • C. difficile toxin test - if recent • C. difficile toxin test - if recent hospitalisation hospitalisation or antibiotics -

Acute Abdomen
Acute abdomen: Shaking down the Acute abdominal pain can be difficult to diagnose, requiring astute assessment skills and knowledge of abdominal anatomy 2.3 ANCC to discover its cause. We show you how to quickly and accurately CONTACT HOURS uncover the clues so your patient can get the help he needs. By Amy Wisniewski, BSN, RN, CCM Lehigh Valley Home Care • Allentown, Pa. The author has disclosed that she has no significant relationships with or financial interest in any commercial companies that pertain to this educational activity. NIE0110_124_CEAbdomen.qxd:Deepak 26/11/09 9:38 AM Page 43 suspects Determining the cause of acute abdominal rapidly, indicating a life-threatening process, pain is often complex due to the many or- so fast and accurate assessment is essential. gans in the abdomen and the fact that pain In this article, I’ll describe how to assess a may be nonspecific. Acute abdomen is a patient with acute abdominal pain and inter- general diagnosis, typically referring to se- vene appropriately. vere abdominal pain that occurs suddenly over a short period (usually no longer than What a pain! 7 days) and often requires surgical interven- Acute abdominal pain is one of the top tion. Symptoms may be severe and progress three symptoms of patients presenting in www.NursingMadeIncrediblyEasy.com January/February 2010 Nursing made Incredibly Easy! 43 NIE0110_124_CEAbdomen.qxd:Deepak 26/11/09 9:38 AM Page 44 the ED. Reasons for acute abdominal pain Visceral pain can be divided into three Your patient’s fall into six broad categories: subtypes: age may give • inflammatory—may be a bacterial cause, • tension pain. -

Pneumatosis Intestinalis Presenting As Small Bowel Obstruction Without Bowel Ischemia After Mechanical Ventilation
Acute and Critical Care 2019 February 34(1):81-85 Acute and Critical Care https://doi.org/10.4266/acc.2016.00311 | pISSN 2586-6052 | eISSN 2586-6060 Pneumatosis Intestinalis Presenting as Small Bowel Obstruction without Bowel Ischemia after Mechanical Ventilation Dong Joon Kim1, Yong Joon Choi1, Young Sun Yoo2 Departments of 1Anesthesiology and Pain Medicine and 2Surgery, Chosun University Hospital, Gwangju, Korea Pneumatosis intestinalis (PI) is a rare condition of the presence of gas within the bowel walls. PI is associated with numerous underlying diseases, ranging from life-threatening to innocu- Case Report ous conditions. PI is believed to be secondary to coexisting disorders in approximately 85% of all cases. This paper reviews the case of a patient who was diagnosed 7 years prior with pneu- Received: April 18, 2016 Revised: September 12, 2016 moperitoneum from unknown causes without any symptoms. The patient was admitted to Accepted: September 28, 2016 the intensive care unit for the management of aspiration pneumonia and developed exten- sive PI after mechanical ventilation, presenting as small bowel obstruction with mesenteric Corresponding author torsion. Although the exact mechanism and etiology of PI are unclear, this case provides an Young Sun Yoo update on the imaging features of and the clinical conditions associated with PI, as well as Department of Surgery, Chosun University Hospital, 365 Pilmun- the management of this condition. daero, Dong-gu, Gwangju 61453, Korea Key Words: intestinal obstruction; pneumatosis intestinalis; pulmonary emphysema Tel: +82-62-220-3676 Fax: +82-62-228-3441 E-mail: [email protected] Pneumatosis intestinalis (PI) is described as the presence of gas confined within the bowel walls. -

Milky Mesentery: Acute Abdomen with Chylous Ascites
C A S E RE P O R T Milky Mesentery: Acute Abdomen with Chylous Ascites AAKANKSHA GOEL, MANISH KUMAR GAUR AND PANKAJ KUMAR GARG From Department of Surgery, University College of Medical Sciences and Guru Teg Bahadur Hospital, Shahdara, Delhi, India. Correspondence to: Dr Aakanksha Background: Clinical presentations of intestinal lymphangiectasia include pitting edema, Goel, House No 1 Sukh Vihar, chylous ascites, pleural effusion, diarrhea, malabsorption and intestinal obstruction. Case Delhi 110 051, India. Characteristics: An 8-year-old male child presented to the emergency department with [email protected] clinical features of peritonitis, raising suspicion of appendicular or small bowel perforation. Intervention/Outcome: Diagnosis of chylous ascites with primary intestinal Received: July 21, 2017; lymphangiectasia made on laparotomy. Message: Acute peritonitis may be a presentation Initial Review: December 26, 2017; of primary intestinal lymphangiectasia and chylous ascites. Accepted: May 24, 2018. Keywords: Acute abdomen, Intestinal lymphangiectasia, Peritonitis. lthough lymphangiectasia is common in the (lymphangiectasia) was made. The chylous fluid was neck and axilla, it rarely involves intra- drained and a thorough peritoneal lavage was done. abdominal organs [1]. Intestinal Biopsies were taken from the mesenteric lymph nodes and Alymphangiectasia is characterized by peritoneum. dilatation of intestinal lymphatics [2,3]. The clinical Histopathological report was negative for tuberculosis presentations of intestinal lymphangiectasia include and malignancy. The ascitic fluid was rich in triglycerides pitting edema, chylous ascites, pleural effusion, diarrhea, (254 mg/dL) and demonstrated chylomicrons and malabsorption and intestinal obstruction. Acute lymphocytes on biochemical analysis. Culture and gram peritonitis is a rare presentation, and it may mimic other stain were negative. -

An Osteopathic Approach to Reduction of Readmissions for Neonatal Jaundice
Osteopathic Family Physician (2013) 5, 17–23 REVIEW ARTICLE An osteopathic approach to reduction of readmissions for neonatal jaundice Rachel Click, DO,a Julie Dahl-Smith, DO,a Lindsay Fowler, DO,a Jacqueline DuBose, MD,a Margi Deneau-Saxton, RN, CCCE, CIMI, CLC, CPD,b Jennifer Herbert, MDc From aGeorgia Health Sciences University, Medical College of Georgia, Department of Family Medicine, GA; bGeorgia Health System, OB Labor and Delivery, GA; and cUniversity Primary Care, Evans, GA. KEYWORDS: Jaundice is a potentially life-threatening condition that continues to affect at-risk newborns, accounting Breastfeeding; for continued hospital readmissions. As family physicians, we should be cognizant of neonates who may Jaundice; be at risk for jaundice, including those with pathologic jaundice as well as newborns of breastfeeding Prevention; mothers, and ensure sufficient intervention is taken to help prevent further elevations in bilirubin levels. Hyperbilirubinemia; Interventions are likely to include evaluation for sepsis, education regarding feeding frequencies for both Neonatal massage breast- and bottle-fed neonates, reviewing maternal and hematologic risk factors for neonatal jaundice, and considering inborn errors of metabolism. An additional measure family physicians may consider is that of neonatal massage for those with elevated bilirubin levels. Neonatal massage, though not widely used, has been proven to promote excess bilirubin excretion, thus decreasing length of hospital stay; all the while, providing an intervention that allows parents to take an active role. r 2013 Elsevier Inc. All rights reserved. Introduction morbidity rate with bilirubin 4 20 mg/dL. “It has been estimated that the risk of kernicterus in infants with total Jaundice is a product of excess bilirubin (a product of serum bilirubin (TSB) greater than 30 mg/dL is about 1 in broken down red blood cells), which manifests as a 7 infants”.1 Less serious complications of hyperbilirubine- yellowing of the skin and eyes. -

Evaluation of Acute Abdominal Pain in Adults Sarah L
Evaluation of Acute Abdominal Pain in Adults SARAH L. CARTWRIGHT, MD, and MARK P. kNUDSON, MD, MSPh Wake Forest University School of Medicine, Winston-Salem, North Carolina Acute abdominal pain can represent a spectrum of conditions from benign and self-limited disease to surgical emergencies. Evaluating abdominal pain requires an approach that relies on the likelihood of disease, patient history, physical examination, laboratory tests, and imag- ing studies. The location of pain is a useful starting point and will guide further evaluation. For example, right lower quadrant pain strongly suggests appendicitis. Certain elements of the history and physical examination are helpful (e.g., constipation and abdominal distension strongly suggest bowel obstruction), whereas others are of little value (e.g., anorexia has little predictive value for appendicitis). The American College of Radiology has recommended dif- ferent imaging studies for assessing abdominal pain based on pain location. Ultrasonography is recommended to assess right upper quadrant pain, and computed tomography is recom- mended for right and left lower quadrant pain. It is also important to consider special popula- tions such as women, who are at risk of genitourinary disease, which may cause abdominal pain; and the elderly, who may present with atypical symptoms of a disease. (Am Fam Physi- cian. 2008;77(7):971-978. Copyright © 2008 American Academy of Family Physicians.) bdominal pain is a common pre- disease (e.g., vascular diseases such as aor- sentation in the outpatient setting tic dissection and mesenteric ischemia) and and is challenging to diagnose. surgical conditions (e.g., appendicitis, cho- Abdominal pain is the present- lecystitis). -

INFORMED CARING JAUNDICE Neonatal Jaundice BILIARY
1 INFORMED CARING Situations with Adults and Children with Gallbladder, Liver and Pancreatic Disorders 2 JAUNDICE ä Does NOT mean hepatitis ä Increased breakdown of RBCs ä Altered bilirubin breakdown ä Impeded flow through liver or bile duct ä First seen in sclera, then skin 3 Neonatal Jaundice ä Not liver failure ä RBC breakdown ä Phototherapy 4 BILIARY ATRESIA ä Jaundice 2-3 weeks after birth ä Easy bruising ä Stools putty like ä Tea colored urine ä Abdominal/organ distension 5 4 F’s of Gallbladder ä Fair ä Fat X size of person X amount in diet ä Fertile X BCP X Multiparity ä Forty 6 Cholelithiasis ä Calculi within the duct or gallbladder ä Severe colicky, cramp-like pain X radiates to shoulder blade X Murphy's sign ä Cholecystitis: inflammation X Can be caused by trauma, fasting, TPN or abdominal surgery 7 Diagnostic Studies ä Ultrasound of abdomen 1 X not for the obese ä HIDA scan X nuclear medicine ä Cholangiograms X endoscopic X transvenous X intraoperative 8 Post-op Care ä High abdominal incision X respiratory compromise ä T-tube X patients need to know how to empty it X may clamp it prior to removal X caution not dislodged with movements ä NO Morphine X spasms of sphincter of Oddi 9 Post-op Nutrition ä Limited fat in diet X can have rapid transit times ä Potential fat soluble vitamin deficit X A, D, E and K ä Weight loss diet 10 LIVER FAILURE ä Cirrhosis ä Drug toxicity X acetaminophen, anesthetics, HCTZ, chemotherapy ä Infection ä Cancer ä ETOH is single most linked cause 11 LIVER FAILURE S/S ä Don’t show up until 80-90% failed -

Abdominal Pain
10 Abdominal Pain Adrian Miranda Acute abdominal pain is usually a self-limiting, benign condition that irritation, and lateralizes to one of four quadrants. Because of the is commonly caused by gastroenteritis, constipation, or a viral illness. relative localization of the noxious stimulation to the underlying The challenge is to identify children who require immediate evaluation peritoneum and the more anatomically specific and unilateral inner- for potentially life-threatening conditions. Chronic abdominal pain is vation (peripheral-nonautonomic nerves) of the peritoneum, it is also a common complaint in pediatric practices, as it comprises 2-4% usually easier to identify the precise anatomic location that is produc- of pediatric visits. At least 20% of children seek attention for chronic ing parietal pain (Fig. 10.2). abdominal pain by the age of 15 years. Up to 28% of children complain of abdominal pain at least once per week and only 2% seek medical ACUTE ABDOMINAL PAIN attention. The primary care physician, pediatrician, emergency physi- cian, and surgeon must be able to distinguish serious and potentially The clinician evaluating the child with abdominal pain of acute onset life-threatening diseases from more benign problems (Table 10.1). must decide quickly whether the child has a “surgical abdomen” (a Abdominal pain may be a single acute event (Tables 10.2 and 10.3), a serious medical problem necessitating treatment and admission to the recurring acute problem (as in abdominal migraine), or a chronic hospital) or a process that can be managed on an outpatient basis. problem (Table 10.4). The differential diagnosis is lengthy, differs from Even though surgical diagnoses are fewer than 10% of all causes of that in adults, and varies by age group. -

Symptomatic Approach to Gas, Belching and Bloating 21
20 Osteopathic Family Physician (2019) 20 - 25 Osteopathic Family Physician | Volume 11, No. 2 | March/April, 2019 Gennaro, Larsen Symptomatic Approach to Gas, Belching and Bloating 21 Review ARTICLE to escape. This mechanism prevents the stomach from becoming IRRITABLE BOWEL SYNDROME (IBS) Symptomatic Approach to Gas, Belching and Bloating damaged by excessive dilation.2 IBS is abdominal pain or discomfort associated with altered with OMT Treatment Options Many patients with GERD report increased belching. Transient bowel habits. It is the most commonly diagnosed GI disorder lower esophageal sphincter (LES) relaxation is the major and accounts for about 30% of all GI referrals.7 Criteria for IBS is recurrent abdominal pain at least one day per week in the Carly Gennaro, DO1; Helaine Larsen, DO1 mechanism for both belching and GERD. Recent studies have shown that the number of belches is related to the number of last three months associated with at least two of the following: times someone swallows air. These studies have concluded that 1) association with defecation, 2) change in stool frequency, 1 Good Samaritan Hospital Medical Center, West Islip, NY patients with GERD swallow more air in response to heartburn and 3) change in stool form. Diagnosis should be made using these therefore belch more frequently.3 There is no specific treatment clinical criteria and limited testing. Common symptoms are for belching in GERD patients, so for now, physicians continue to abdominal pain, bloating, alternating diarrhea and constipation, treat GERD with proton pump inhibitors (PPIs) and histamine-2 and pain relief after defecation. Pain can be present anywhere receptor antagonists with the goal of suppressing heartburn and in the abdomen, but the lower abdomen is the most common KEYWORDS: ABSTRACT: Intestinal gas production is a normal physiologic progress. -
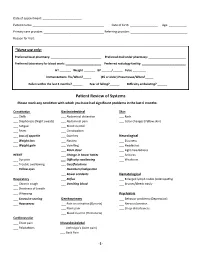
Patient Review of Systems Please Mark Any Condition with Which You Have Had Significant Problems in the Last 6 Months
Date of appointment: ________________________ Patient name: ____________________________________________ Date of birth: _________________ Age: ___________ Primary care provider: _____________________________________ Referring provider: ___________________________________ Reason for Visit: _____________________________________________________________________________________________ *Nurse use only: Preferred local pharmacy: _______________________________ Preferred mail order pharmacy: _______________________ Preferred laboratory for blood work: ______________________ Preferred radiology facility: ___________________________ HT _______ Weight _______ BP ______/______ Pulse ________ Immunizations: Flu/When?_____ (65 or older) Pneumovax/When?_____ Fallen within the last 3 months? ______ Fear of falling?______ Difficulty ambulating? ______ Patient Review of Systems Please mark any condition with which you have had significant problems in the last 6 months: Constitution Gastrointestinal Skin ___ Chills ___ Abdominal distention ___ Rash ___ Diaphoresis (Night sweats) ___ Abdominal pain ___ Color changes (Yellow skin) ___ Fatigue ___ Blood in stool ___ Fever ___ Constipation ___ Loss of appetite ___ Diarrhea Neurological ___ Weight loss ___ Nausea ___ Dizziness ___ Weight gain ___ Vomiting ___ Headaches ___ Black stool ___ Light-headedness HEENT ___ Change in bowel habits ___ Seizures ___ Eye pain ___ Difficulty swallowing ___ Weakness ___ Trouble swallowing ___ Gas/flatulence ___ Yellow eyes ___ Heartburn/indigestion ___ Bowel accidents Hematological