Better Care, Through Better Technology | 2015 HEART and VASCULAR REPORT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Still Thriving Cover Story: Peterman’Sflower Shop Continues Impressive History
December 2019 Still thriving Cover story: Peterman’sFlower Shop continues impressive history ................................PAGES 3 Altoona chiropractors have harmonious goals ................................PAGE 5 Ribbon Cuttings ..........................PAGE 15-16 695-5323 COMMERCIAL OPPORTUNITIES COMMERCIAL OPPORTUNITIES FOR SALE/LEASE - LISTING AGENT MATT DEPAOLIS 814-329-3021 LZe^ hk E^Zl^' Hpg^k ÛgZg\bg` Zg] \hg]h himbhgl #52799 & E>:L>' :iikhqbfZm^er +%,.) lj _m hg ma^ fZbg ZoZbeZ[e^' FZbg [nbe]bg` aZl ZiikhqbfZm^er ,-%-22 l_ e^o^e *%+)) lj _m hg ma^ ehp^k e^o^e' <hfie^m^ k^ghoZmbhg pbma - ehZ]bg` ]h\dl Zg] mph `khng] e^o^e ho^ka^Z] h_ ma^ ^qm^kbhk fZbg e^o^e fZdbg` mabl \eZll : h_Û\^ liZ\^' ]hhkl' <nkk^gm m^gZgm h\\nib^l ZiikhqbfZm^er +%+/+ l_ h_ FZbg e^o^e :=: \hfiebZgm' LaZk^] nl^ h_ Z eZk`^ \hg_^k^g\^ h_Û\^ Zg] +,%+)) l_ h_ pZk^ahnl^ liZ\^' :iikhqbfZm^er *)%1))l_ h_ fZbg [nbe]bg` Zg] *%*.+ bg Z ]^mZ\a^] [nbe]bg` khhf(\eZll khhf' ?ehhkbg` ZeehpZg\^' Ab`a mkZ_Û\ \hngm Zg] \nkk^gmer ngh\\nib^]' K^lb]^gmbZe ngbm hg ma^ l^\hg] Ühhk' ]bk^\m Z\\^ll mh B&22 Km^ ++' <hgmZ\m FZmm =^IZhebl !1*-" <Zee FZmm =^IZhebl !1*-" ,+2&,)+* ,+2&,)+* _hk fhk^ bg_hkfZmbhg Zg] mh l^m ni Z mhnk' 2 Blair County 2 Blair Business Mirror Chamber News www.blairchamber.com Chamber Notes New Members Heading to 2020 with my hair on fire Sometimes the hardest part of writing approved by the Chamber Board of Direc- this column is coming-up with an appro- tors is making the Business Hall of Fame priate title. -

UPMC Quarterly Disclosure
UPMC Quarterly Disclosure For the Period Ended June 30, 2016 UPMC QUARTERLY DISCLOSURE FOR THE PERIOD ENDED JUNE 30, 2016 TABLE OF CONTENTS Introduction to Management’s Discussion and Analysis . .1 Management’s Discussion and Analysis Financial Highlights . .2 Operating Component Information . .5 Revenue and Operating Metrics . .8 Key Financial Indicators . .11 Market Share . 12 Asset and Liability Management . 13 Utilization Statistics . 15 Outstanding Debt . 16 Debt Covenant Calculations . 17 Audited Consolidated Financial Statements Report of Independent Registered Public Accounting Firm 19 Consolidated Balance Sheets . .20 Consolidated Statements of Operations and Changes in Net Assets . .21 Consolidated Statements of Cash Flows . .22 Notes to Consolidated Financial Statements . .23 The following financial data is derived from both the June 30, 2016 audited consolidated financial statements of UPMC and the unaudited interim consolidated financial statements of UPMC The interim financial data includes all adjustments consisting of a normal recurring nature that UPMC considers necessary for a fair presentation of its financial position and the results of operations for these periods Operating and financial results reported herein are not necessarily indicative of the results that may be expected for any future periods The information contained herein is being filed by UPMC for the purpose of complying with its obligations under Continuing Disclosure Agreements entered into in connection with the issuance of the series of bonds listed -

A Quick Guide for Patients and Family Learn More About Local Restaurants, Hotels, and Pharmacies
A Quick Guide for Patients and Family Learn more about local restaurants, hotels, and pharmacies. Hospital Phone Numbers • Main Hospital Number – 889-2011 • Dietary –889-2351 • Gift Shop – 889-2080 • Front Lobby/Desk –889-6613 • Information Desk –889-2094 • Patient Access –889-2236 • Pastoral Care – 889- 2132 • Patient Relations –889-3219 • Hospital Police –889-2121 *Please dial 9 to get an outside line on your bedside phone. Restaurants • 12Eleven Brisket: 814-201-2311 • Allstar Pizza and Subs: 814-942-7070 • Brothers Pizza: 814-942-1900 • Dickey’s Barbeque Pit: 814-201-2770 • Great China Chinese Restaurant: 814-941-8780 • Hungry Howie’s Pizza: 814-943-7000 • Lychee: 814-940-8600 • Mama Randazzo’s Pizzeria: 814-943-9011 • No. 1 Chinese Restaurant: 814-949-9583 • OIP (Original Italian Pizza): 814-946-9400 • Tom and Joe’s: 814-943-3423 • Tost at Market Square: 814-515-2233 Fast Food Options (1-mile radius) • McDonalds • Sheetz • Taco Bell • Wendy’s Local Hotels and the Friendship House Wingate by Wyndham Altoona Donna Jean Friendship House at 909 Chestnut Avenue UPMC Altoona Altoona, PA 16601 Check availability with hospital police at (814) 515-2233 814-889-2121. (0.3 miles from UPMC Altoona) Microtel Inn & Suites by Wyndham *Please ask about patient/family hospital 1601 Valley View Blvd rates when checking into a hotel! Altoona, PA 16602 (814) 946-1400 (2.2 miles from UPMC Altoona) Fairfield Inn & Townplace Suites – Marriott 2915 Pleasant Valley Blvd Altoona, PA 16602 (814) 946-0422 (3.3 miles from UPMC Altoona) Hampton Inn Altoona 180 Charlotte Drive Altoona, PA 16601 (814) 941-3500 (5.5 miles from UPMC Altoona) Days Inn & Suites Altoona 458 Sabbath Rest Road Altoona, PA 16601 (814) 944-4499 (5.7 miles from UPMC Altoona Comfort Suites 140 Stroehman Drive Altoona, PA 16601 (814) 942-2600 (6.0 miles from UPMC Altoona) Courtyard by Marriott- 2 Convention Center Drive Altoona, PA 16602 (814) 312-1800 online code U39 (6.0 miles from UPMC Altoona) Local Pharmacies Altoona Pharmacy* UPMC Altoona Suite 403- G -Building 814-283-0602 Mon-Fri: 8 a.m. -

Frequently Asked Insurance Questions
Frequently Asked Insurance Questions If I have a Highmark card, can I utilize UPMC Hamot Medical Center and their physicians? • Yes, but services will be processed under the out-of-network level of benefits, subject to a higher deductible, coinsurance and may be subject to balance billing. Emergency services will be covered at the in-network level of benefits. If I have a UPMC card, can I utilize Saint Vincent Health System and their physicians? • Yes, but services will be processed under the out-of-network level of benefit, subject to a higher deductible, coinsurance and may be subject to balance billing. What is Highmark’s provider and hospital network outside of Western Pennsylvania? • Highmark has a nationwide network and access to participating providers in each state. Will my prescription drugs remain covered if I switch from Highmark to another carrier? • Every carrier has a preferred formulary which is a list of drugs that offer the greatest overall value to the members. These formularies may vary slightly and are subject to change. What is Highmark’s preferred/formulary drug list? • You can access Highmark’s formulary by visiting their website at www.HighmarkBCBS.com Can I have UPMC coverage and my spouse have Highmark coverage? • Only if you are both employed at the Erie School District. Will there be a pre-existing condition disruption by moving to another carrier? • No, pre-existing conditions will not be affected. Can I switch back to my previous carrier if my employer offers a dual choice? • Yes, during your annual open enrollment period What UPMC facilities will remain in network for Highmark members after 7/1/2019? • Children’s Hospital of Pittsburgh (through 6/30/2022), UPMC Altoona, UPMC Bedford, UPMC Kane, UPMC Jameson, UPMC Northwest, UPMC Horizon (both campuses). -
20 Under 40 Recipients Since the Program’S Inception in 2007
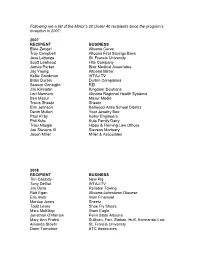
Following are a list of the Mirror’s 20 Under 40 recipients since the program’s inception in 2007: 2007 RECIPIENT BUSINESS Elsie Zengel Altoona Curve Troy Campbell Altoona First Savings Bank Jess Lattanza St. Francis University Scott Lawhead Hite Company James Parker Blair Medical Associates Jay Young Altoona Mirror Kellie Goodman WTAJ-TV Brian Durbin Durbin Companies Season Consiglio REI Jim Kilmartin Kingdom Solutions Lori Manners Altoona Regional Health Systems Ben Mazur Mazur Media Travis Sheetz Sheetz Erin Johnson Bellwood-Antis School District Devin Mullen Your Jewelry Box Paul Kirby Keller Engineers Phil Kulp Kulp Family Dairy Traci Naugle Hippo & Fleming Law Offices Joe Stevens III Stevens Mortuary Jason Miller Miller & Associates 2008 RECIPIENT BUSINESS Tim Cassidy New Pig Tony DeGol WTAJ-TV Jim Della Reliable Towing Rob Egan Altoona-Johnstown Diocese Eric Irwin Irwin Financial Monica Jones Sheetz Todd Lewis Shoe Fly Shoes Marc McKillop Giant Eagle Jonathan O’Harrow Penn State Altoona Mary Ann Probst Sullivan, Forr, Stokan, Huff, Kormanski Law Amanda Stoehr St. Francis University Darin Tornatore ATC Associates Tara Wood Sanofi-Aventis Phamaceutical Rachel Derby Blair County Respiratory Amanda Barry Altoona Mirror Sarah Piper Hollidaysburg Community Partnership Jeff Garner Altoona Curve Jen Mallad Blair Business Communications Jason Davis Snap Fitness Matt Garber Virtual Office Systems 2009 RECIPIENT BUSINESS Amy Mearkle WTAJ-TV Matthew Fox ABCD Tyke Steiner Hollidaysburg YMCA Jennifer Knisely Altoona Public Library Mike Hofer Central Blair Rec Commission *Matt Vipond Vipond Appliance Sean Burke McQuaide Blasko Law Elizabeth Benjamin Andrews & Beard Law Offices Robert Donlan The Hancock Group Cory Giger Altoona Mirror Derek Miller Advantage Resource Group Becky Crilly Reliance Bank Joe Nyanko JPN Management Inc. -

19-ALSM-0265-Annual-Report.Pdf
2018 ANNUAL REPORT “ALSM serves the most vulnerable. From seniors who are no longer able to pay for their care to families who are struggling to raise their children, Greetings! Jesus calls us to help the least among us. I support It is that time of the year when we share with you what we as Allegheny Lutheran Social Ministries ALSM knowing that I am supporting those in need. (ALSM) have achieved by meeting the needs of the people we serve. As a former teacher, it is important to me to see the benefit of the Head Start program for children and Last year, we provided $2.6 million in benevolent support to those in our care who have limited the intergenerational childcare and programming. funds. We are grateful for the generosity of our donors, both past and present, who have supported It is a great opportunity for both children and the ALSM so that we have the investments to continue our mission of service. aging population.” - Helen Brenneman, ALSM Donor, In addition to our benevolent care, we also accomplished the following: Board of Trustees • Blairmont Commons cottages were completed. They were fully and quickly occupied with persons 55 and over. • At our Annual Dinner we honored several people who have made a Allegheny Lutheran difference in the history of ALSM. Those honorees are Mondon Smith, Social Ministries Board who received The Rev. Dr. Luke Rhoads Lutheran of the Year award; of Trustees George Penrod, designated as the Helping Hand recipient; Meghan and Carrie Frederick, who received the Youth Service award. -

Community Health Needs Assessment Community Health Strategic Plan Bedford and Blair Counties
Community Health Needs Assessment Community Health Strategic Plan Bedford and Blair Counties June 30, 2019 Enhancing the Health of Our Communities Bedford and Blair Counties COMMUNITY HEALTH NEEDS ASSESSMENT UPDATE COVERING UPMC BEDFORD UPMC ALTOONA Table of Contents Introduction Regional Progress Report: 2016 – 2019 . Page 1 I. Executive Summary................................................................Page 4 II. Overview and Methods Used to Conduct the Community Health Needs Assessment .........Page 8 III. Results of the Community Health Needs Assessment and In-Depth Community Profile .......Page 14 IV. UPMC Hospitals: Community Health Improvement Progress and Plans .....................Page 28 2016 – 2019 Progress Reports and 2019 – 2022 Implementation Plans by Hospital UPMC Bedford . Page 26 UPMC Altoona . Page 35 V. Appendices.......................................................................Page 45 Appendix A: Secondary Data Sources and Analysis . Page 46 Appendix B: Detailed Community Health Needs Profile . Page 48 Appendix C: Input from Persons Representing the Broad Interests of the Community . Page 51 Appendix D: Concept Mapping . Page 56 Appendix E: Healthy Blair County Coalition: Community Health Needs Assessment and Implementation Plan . Page 60 2016-2019 UPMC is stepping forward to help our neighbors in Bedford and Blair counties by offering REGIONAL programs and services to improve health and PROGRESS REPORT quality of life in our communities . PROVIDING LOCAL ACCESS TO NATIONALLY • Caring for More Patients with Telemedicine: Founded in 2013, the RANKED, WORLD-CLASS CARE UPMC Bedford Teleconsult Center is a multi-specialty outpatient clinic that uses advances in technology to connect patients with UPMC is taking steps to make health care more convenient for those specialists. From 2013 to 2017, the UPMC Bedford Teleconsult we serve. -

How to Deliver High-Specialty Care At
How to deliver high-specialty care at home after liver transplantation: a sustainable approach Giovanni Vizzini, MD Department of Medicine - Transplant Hepatology Unit ISMETT-UPMC Palermo - Italy Evidenze cliniche ed economiche dei miglioramenti prodotti dall’uso dell’IT: l’IT realmente riduce i costi e migliora la cura? FORUM PA 2013 29 Maggio 2013 - Roma – Palazzo dei Congressi Agenda • A clinical perspective 1. ISMETT-UPMC: a multi-organ transplant center in Palermo (Italy) 2. The clinical patient’s needs after discharge from hospital 3. The limited resources 4. The challenge: Best care at the lower cost 5. The innovative use of available (and simple) technology 6. Clinical Results and Sustainability ISMETT-UPMC in Palermo (Italy) • ISMETT is a public-private 78-bed hospital partnership (The Sicilian Region - The University of Pittsburgh Medical Center) situated in Palermo, Sicily. It is the only multiorgan (liver, heart, lung, kidney and pancreas) transplant centre in Southern Italy. • We provide high specialty surgical and non-surgical procedures to the entire regional population (approximately 5 million people living in the Sicilian Region). • More than 1.300 patients have had transplants at ISMETT in the last 10 years. Solid organs transplant recipients: a growing population 160 ISMETT: 1378 transplants from July 1999 to Dec 2012 140 120 100 80 60 40 20 0 12 27 1999 49 2000 40 58 91 150 2001 104 2002 146 2003 127 2004 131 2005 118 2006 135 2007 133 2008 2009 2010 2011 2012 Solid organs transplant recipients: a growing population -

Rite Aid / Subway
OFFERING MEMORANDUM RITE AID / SUBWAY 3106 EAST PLEASANT VALLEY BLVD | ALTOONA (BELLWOOD) , PA 16601 EXCLUSIVELY LISTED BY: TABLE OF MATTHEW GORMAN CONTENTS +1 484 567 2340 [email protected] 04 TENANT OVERVIEW MICHAEL SHOVER +1 484 567 2344 06 FINANCIAL ANALYSIS [email protected] Property Highlights Financial Overview Investment Overview THOMAS FINNEGAN +1 484 567 2375 PROPERTY SUMMARY [email protected] 10 Property Photos Aerial Map Location Overview ROBERT THOMPSON Local/Regional Map +1 484 567 3341 Demographics [email protected] © 2017© 2019 CBRE, CBRE, INC. INC.ALL RIGHTS ALL RIGHTS RESERVED. RESERVED. VIEW PROPERTY VIDEO TENANT OVERVIEW RITE AID / SUBWAY | ALTOONA, PA TENANT OVERVIEW TENANT OVERVIEW FINANCIAL ANALYSIS PROPERTY SUMMARY FINANCIAL ANALYSIS TENANT OVERVIEW Rite Aid is the largest drugstore chain on the East Coast and the third-largest Subway is a privately held American fast food restaurant franchise that in the United States, employing roughly 89,000 associates. The company primarily serves submarine sandwiches and salads. Subway is one of operates retail drugstores which sell prescription drugs, as well as front- the fastest-growing franchises in the world and, as of June 2017, has end products including over-the-counter medications, health and beauty approximately 44,000 stores located in more than 112 countries. It world's aids, personal care items, cosmetics, household items, convenience foods, largest restaurant chain, serving 7 million made-to-order sandwiches a day. greeting cards, and seasonal merchandise. As of Dec 2, 2017, Rite Aid Founded more than 52 years ago, Subway is still a family-owned business, operated 4,404 stores in 31 states and the District of Columbia. -

World-Class Care in the Mediterranean
ISTITUTO MEDITERRANEO PER I TRAPIANTI E TERAPIE AD ALTA SPECIALIZZAZIONE For further information, please contact: ISMETT Phone: +39 091 21-92-111 Via E. Tricomi, 5 Fax: +39 091 21-92-400 90127 Palermo [email protected] Italy www.ismett.edu To book a consult: Phone: +39 091 21-92-133 [email protected] CLINICAL DISTINCTION ISMETT (Istituto Mediterraneo per i Trapianti e Terapie ad Alta Specializzazione) is a center of excellence in the field of transplantation. ISMETT physicians and researchers are major contributors to the advancement of therapies for patients requiring transplantation services. On September 12, 2014, the Italian Ministry of Health designated ISMETT a government- approved research hospital (Istituto di Ricovero e Cura a Carattere Scientifico - IRCCS) for treatment and research of end-stage organ diseases. An example of innovative and efficient clinical management, ISMETT is the result of a joint public-private partnership between the Region of Sicily through ARNAS Civico Hospital in Palermo and UPMC (University of Pittsburgh Medical Center), a U.S.-based health care system. In June 2017 the Ri.MED Foundation, established by the President of the Council of Ministers, entered the governance of ISMETT. ISMETT offers solid organ transplant programs with results consistent with those of top international health care facilities. World-Class Care in the Mediterranean An International Partnership for ISMETT is the first hospital in Southern Italy to receive Joint Commission International (JCI) Research and Patient Care accreditation, an advanced accreditation system that assesses the quality and safety of hospital facilities. JCI accreditation confirms ISMETT's top standards of patient care and patient safety, as well as an ongoing commitment to continuous improvement. -

Sam's Club Operates 597 Membership Warehouse Clubs in 44 U.S
1 Absolute NNN Lease Investment Opportunity 2500 W Plank Rd | Altoona, PA 16601 Actual Property Image EXCLUSIVELY MARKETED BY: 2 MAX FREEDMAN Lic. # 644481 512.766.2711 | DIRECT [email protected] 2101 S IH 35, Suite 402 Austin, TX 78741 CHRIS SANDS JENNIFER STEIN 844.4.SIG.NNN Lic. # 93103 Lic. # RM422728 www.SIGnnn.com 310.870.3282 | DIRECT 213.446.5366 | DIRECT In Cooperation with JDS Real Estate Services – Lic # RB068057 [email protected] [email protected] © 2018 Sands Investment Group (SIG). The information contained in this ‘Offering Memorandum,’ has been obtained from sources believed to be reliable. Sands Investment Group does not doubt its accuracy, however, Sands Investment Group makes no guarantee, representation or warranty about the accuracy contained herein. It is the responsibility of each individual to conduct thorough due diligence on any and all information that is passed on about the property to determine it’s accuracy and completeness. Any and all projections, market assumptions and cash flow analysis are used to help determine a potential overview on the property, however there is no guarantee or assurance these projections, market assumptions and cash flow analysis are subject to change with property and market conditions. Sands Investment Group encourages all potential interested buyers to seek advice from your tax, financial and legal advisors before making any real estate purchase and transaction. TABLE OF CONTENTS 3 Sam’s Club | 2500 W Plank RD | Altoona, PA 16601 Investment Overview Investment Summary Investment Highlights Area Overview Location Map Retail Map Demographics City Overview Tenant Overview Tenant Profile Lease Abstract Lease Summary Rent Roll INVESTMENT OVERVIEW 4 INVESTMENT SUMMARY 5 Sands Investment Group is pleased to present for sale the Sam’s Club located at 2500 W Plank Road in Altoona, Pennsylvania. -

(Allegheny County, Pennsylvania) UPMC REVENUE BONDS, SERIES 2012
PRELIMINARY OFFICIAL STATEMENT DATED JULY 13, 2012 NEW ISSUE—BOOK ENTRY ONLY RATINGS: Moody’s: S&P: Fitch: (See “RATINGS” herein) In the opinion of Bond Counsel, under existing law and assuming continuing compliance by the Monroeville Finance Authority (the “Authority”) and UPMC (the “Corporation”) with certain covenants related to the Internal Revenue Code of 1986, as amended (the “Code”), interest on the 2012 Bonds (including any original issue discount properly allocable to an owner thereof) is excludable from gross income for federal income tax purposes and is not an item of tax preference for purposes of the federal alternative minimum tax; however, interest with respect to the 2012 Bonds may be taken into account in determining “adjusted current earnings” for purposes of computing the alternative minimum tax on certain corporations. Bond Counsel’s opinion assumes compliance by the Authority and the Corporation with all requirements of the Code that must be satisfied subsequent to the issuance of the 2012 Bonds in order that the interest thereon be, and continue to be, excludable from gross income for federal income tax purposes. Furthermore, in the opinion of Bond Counsel, the 2012 Bonds are exempt from personal property taxes in Pennsylvania and the interest on the 2012 Bonds is exempt from Pennsylvania corporate net income tax and personal income tax. See “TAX EXEMPTION AND OTHER TAX MATTERS”. $420,000,000* MONROEVILLE FINANCE AUTHORITY (Allegheny County, Pennsylvania) UPMC REVENUE BONDS, SERIES 2012 DATED: Date of Delivery MATURITY: February 15, As shown herein The UPMC Revenue Bonds, Series 2012 (the “2012 Bonds”), being issued by the Monroeville Finance Authority (the “Authority”), will be issued as fully registered bonds and initially registered in the name of Cede & Co., as nominee for The Depository Trust Company (“DTC”), New York, New York, which will act as securities depository for the 2012 Bonds.